When does a benefit period for Medicare begin and end?
Dec 16, 2021 · Medicare benefit periods usually involve Part A (hospital care). A period begins with an inpatient stay and ends after you’ve been out of …
What does Medicare mean by benefit period?
Jan 20, 2022 · A benefit period under Part A begins the day you’re admitted to the hospital and ends when you’ve been discharged for at least 60 days. If you’ve been out of the hospital for more than 60 days and are admitted again, a new benefit period begins. Each benefit period requires that you meet a deductible. It’s $1,556 in 2022, but can change each year.
Does Medicare Advantage have benefit periods?
Your benefit period begins the very day you enter a hospital for care or a skilled nursing facility. The benefit period ends when 60 days have passed since you last received either hospital care or care from a skilled nursing facility. The concept of a benefit period is important because the Medicare Part A deductible is based on the benefit period, rather than a calendar year.
Do I have to pay for Medicare Part?
The Medicare Part A hospital benefit period starts when you’re admitted as an inpatient at a hospital or skilled nursing facility and ends once you’ve gone 60 days in a row without inpatient care. Let’s say you end up in the hospital for a week with pneumonia. You get admitted on November 4th and you’re discharged on November 11th.
How long is a Part A benefit period?
60 daysMedicare benefit periods usually involve Part A (hospital care). A period begins with an inpatient stay and ends after you've been out of the facility for at least 60 days.
What does per benefit period mean?
A benefit period is the length of time during which an insurance policyholder or their dependents may file and receive payment for a covered event. All insurance plans will include a benefit period, which can vary based on policy type, insurance provider, and policy premium.
What does Medicare consider a calendar year?
The Medicare Part D plan year runs from January 1st through December 31st of each year, so the plan year runs for a calendar year rather than 365 days from the date of your initial enrollment (or Initial Enrollment Period).
Does Medicare start over each year?
By definition, these are the only reserve days Medicare will give you in your lifetime. They are not renewed each year. After you exhaust your lifetime reserve days, you will pay all out-of-pocket costs.Nov 22, 2021
Can Medicare benefits be exhausted?
A. In general, there's no upper dollar limit on Medicare benefits. As long as you're using medical services that Medicare covers—and provided that they're medically necessary—you can continue to use as many as you need, regardless of how much they cost, in any given year or over the rest of your lifetime.
Is Medicare Part B deductible based on calendar year?
Does Medicare Part B run on a calendar year? Yes, Medicare Part B does run on a calendar year. The annual deductible will reset each January 1st.
What is the difference between calendar year and benefit year?
All Individual and Family plans are on a calendar year. A plan on a contract year (also called benefit year) runs for any 12-month period within the year. Items like deductible, maximum out-of-pocket expense, etc. will reset at the plan's renewal date.Jun 26, 2015
How often do you pay the Medicare Part B deductible?
annualTo pay, Medicare offers an online payment option called Easy Pay, which you can access with a MyMedicare account. Additionally, you may pay your quarterly premium by mail instead. Alongside the premium, Medicare Part B includes an annual deductible and 20% coinsurance for which you are responsible to pay out-of-pocket.Feb 14, 2022
What is Part A deductible for 2021?
$1,484 inThe Medicare Part A inpatient hospital deductible that beneficiaries will pay when admitted to the hospital will be $1,484 in 2021, an increase of $76 from $1,408 in 2020.Nov 6, 2020
What happens when Medicare runs out?
It will have money to pay for health care. Instead, it is projected to become insolvent. Insolvency means that Medicare may not have the funds to pay 100% of its expenses. Insolvency can sometimes lead to bankruptcy, but in the case of Medicare, Congress is likely to intervene and acquire the necessary funding.Dec 20, 2021
What is the benefit period for the Part A deductible?
After you meet your Part A deductible at the beginning of the benefit period, the first 60 days of your inpatient hospital stay are covered with no daily coinsurance. Similarly, if you qualify for a Medicare-covered SNF stay, you will pay nothing for the first 20 days of your SNF stay within a benefit period.Jun 14, 2016
How often do Medicare days reset?
Your benefits will reset 60 days after not using facility-based coverage. This question is basically pertaining to nursing care in a skilled nursing facility. Medicare will only cover up to 100 days in a nursing home, but there are certain criteria's that needs to be met first.
How many reserve days are there for Medicare Part A?
Starting on Day 91, you start tapping into your lifetime reserve days for Medicare Part A. You have 60 reserve days. Once they are used up and you encounter a long hospitalization, you are responsible for all costs starting with Day 91 in the hospital.
What does Medicare Part A cover?
What is Medicare Part A and what services does it cover? Medicare Part A provides health insurance coverage for inpatient hospital services, in addition to hospice care and limited coverage for skilled nursing care and certain home health services.
How to avoid confusion with Medicare Part A?
One way to avoid the confusion associated with Part A’s benefit periods is to enroll in a Medicare Supplement Insurance plan. These private insurance plans help pay for certain out-of-pocket costs associated with Medicare, including the Medicare Part A costs listed above.
How many people are on Medicare in 2019?
Understanding Medicare Part A Benefit Periods. More than 61 million people in the United States received Medicare benefits in 2019, making it a popular and essential health insurance option for seniors and younger people with certain disabilities and medical conditions.1.
How much will Medicare pay for a day in 2021?
If you’re in the hospital between 61 and 90 days during one benefit period in 2021, each day will cost $371. If you’re in the hospital for more than 90 days during one benefit period, each day beyond that will cost $742. Starting on Day 91, you start tapping into your lifetime reserve days for Medicare Part A. You have 60 reserve days.
How much is the deductible for 2021?
Each benefit period requires that you meet a deductible. It’s $1,484 in 2021, but can change each year. Because hospital care is generally pretty expensive, you should brace yourself to pay that full amount each time you’re in the hospital.
How old is Marge from Medicare?
Meet Marge. She’s over 65 and enrolled in Original Medicare. She’s had some health issues recently and has made a few trips to the hospital. Here’s what she paid under Part A.
When does the benefit period end?
The benefit period ends when 60 days have passed since you last received either hospital care or care from a skilled nursing facility.
Why is a benefit period important?
The concept of a benefit period is important because the Medicare Part A deductible is based on the benefit period, rather than a calendar year. With most other types of health insurance (ie, non-Medicare), the deductible is based on the calendar year. Once you meet it, your plan will pay all or part of your costs for the remainder of the year, ...
When does deductible reset for hospitalization?
Once you meet it, your plan will pay all or part of your costs for the remainder of the year, but then your deductible resets on January 1. So if you happen to be hospitalized from December 30 to January 2, you’d have to pay two deductibles with most non-Medicare plans.
Can you have two deductibles in the same year?
However, you could also end up in a situation where you have two benefit periods — and have to pay your deductible twice — in the same calendar year. For example, if you’re hospitalized for a week in March, that would be the start of a benefit period.
How long does Medicare cover in-hospital care?
After this deductible is met, Medicare will start to cover the remainder of your costs for in-hospital services, such as food, nursing and your bed, for a limit of 60 days following your date of admission. There is $0 copay or coinsurance during this period of time as well. Should you spend the entire period in the hospital, ...
What happens after 90 days of Medicare?
After day 90 in a benefit period, and if the person has no more lifetime reserve days available to use, the Medicare recipient is responsible to pay all of the costs associated with their hospital stay. After you’ve spent 60 days out of the hospital, your benefit period will start all over again. At the start of each new period, you will receive ...
How many days do you have to be out of the hospital to get Medicare?
In order to help you make better sense of this, here’s a breakdown. 60 days: How many days you are required to be out of the hospital or after-care facility to become eligible for another hospital benefit period. 60 days: The maximum number of days that Medicare will pay for all of your inpatient hospital care once you’ve paid your deductible ...
How long do you have to stay in a hospital?
In an Original Medicare plan, you have to stay for a minimum of three days, or more than two nights, to officially be admitted as a patient in a hospital. Only then will Medicare start to pay for your care in a skilled nursing center for additional treatment, like physical therapy or for regular IV injections. The amount of time you spend in the hospital as well as the skilled nursing center will be counted as part of your hospital benefit period. Furthermore, you are required to have spent 60 days out of each in order to be eligible for another benefit period.#N#However, the portion you are expected to pay for the costs of a skilled nursing center differs from the portion you pay for hospital care. In facilities like these, you must pay in any given benefit period: 1 $0 for your room, bed, food and care for all days up to day 20 2 A daily coinsurance rate of $161 for days 21 through 100 3 All costs starting on day 101
How much is Medicare coinsurance?
The Medicare recipient is charged a daily coinsurance for any lifetime reserve days used. The standard coinsurance amount is $682 per day. If you’re enrolled in a supplemental Medicare insurance program, also known as “Medigap,” you will receive another 365 days in your lifetime reserve with no additional copayments.
How much is the hospital stay deductible for Medicare?
You will be expected to pay for the initial cost of your hospital stay up to a limit of $1,364. This is your hospital deductible for Medicare Part A. As opposed to other Medicare deductibles, it begins anew with every hospital benefit period, rather than your first admission to the hospital each year. After this deductible is met, Medicare will ...
How long do you have to be hospitalized before you can be moved to a skilled nursing facility?
For instance, with most policies, you don’t have to be hospitalized for three days before you can be moved to a skilled nursing center.
How long does Medicare Part A last?
A benefit period begins when you enter the hospital and ends when you are out for 60 days in a row. One benefit period may include more than one hospitalization.
When does Medicare kick in?
Starting January 1 or whenever your plan year begins, you pay your health care costs up to the deductible amount. After that, your health plan kicks in to help pay the cost of your care for the rest of the plan year. The cycle starts over at the beginning of each new plan year. Medicare Part A deductibles are different.
How much is the Medicare deductible for 2021?
She is in the hospital over 60 days this time, so she must also pay a co-pay for 5 days. For 2021, the Part A deductible is $1,484 and the daily copay is $371. Item. Amount. First Stay. Medicare Part A deductible. $1,484.
How long is Roger's hospital stay?
Here's an example of how a single benefit period could span more than one hospitalization. Roger is admitted to the hospital in December and stays 5 days. He is readmitted in early February and stays for 3 days. He was out of the hospital less than 60 days before he went back.
How often is Medicare deductible charged?
Many homeowners and car insurance policies charge a deductible whenever you file a claim. A health insurance deductible is usually charged once for the plan year.
What is Medicare Made Clear?
Medicare Made Clear is brought to you by UnitedHealthcare to help make understanding Medicare easier. Click here to take advantage of more helpful tools and resources from Medicare Made Clear including downloadable worksheets and guides.
How long does it take to get a deductible back after a hospital stay?
If you go back into the hospital after 60 days, then a new benefit period starts, and the deductible happens again. You would be responsible for paying two deductibles in this case – one for each benefit period – even if you’re in the hospital both times for the same health problem.
How long is a Medicare benefit period?
Medicare defines a benefit period as: A hospital stay of any length, Plus any time you spend recovering in an inpatient rehabilitation facility , Plus the 60 consecutive days immediately following your release. Benefit Periods Can Be Longer or Shorter Than Illnesses: The term “benefit period” only determines how you get billed.
When does the Medicare benefit period start?
Benefit Period Start: A Medicare benefit period will begin the first day you are admitted to a hospital. Emergency room visits don’t count unless you are admitted to the hospital directly from the ER. When you are first admitted to a hospital, you will have to pay your Medicare Part A deductible, which is $1,484 in 2021.
How much is Medicare Part A deductible for 2021?
When you are first admitted to a hospital, you will have to pay your Medicare Part A deductible, which is $1,484 in 2021. Most popular Medicare Supplements will cover this cost for you. Benefit Period End: Your benefit period will officially end 60 consecutive days after your release from the hospital or from rehab if there are no additional stays.
What is Medicare Advantage?
Medicare Advantage: Medicare Advantage, also known as Part C, plans replace your standard Medicare Part A and Part B. Your copayments would depend on the specific policy you chose. When hospital bills come knocking, Original Medicare (Part A and Part B) begins to show its flaws.
How many times can you pay your Part A deductible?
Worst case, that means you could pay your Part A deductible up to five times in a calendar year – in addition to your regular ...
Does Medicare pay for Part A deductible?
Medicare Supplement: Joining Plan F, Plan G or Plan N would pay the entire Part A deductibles for you and extra hospital days, and 100% of days 21 to 100 in an SNF rehab facility, if they follow a hospital stay. (Note: Newly eligible Medicare beneficiaries can no longer enroll in Plan F as of 2020.
Is Original Medicare enough?
Many people find that having Original Medicare is not enough to shield them from big deductibles and copayments, like the two scenarios at the beginning of this article. If you feel the same way, then take the time to explore your extra coverage options on HealthCare.com.
When will Medicare Part A start?
on December 14, 2020. Medicare Part A has a benefit period that not only affects how much you will pay for care in the hospital or in a skilled nursing facility (SNF) but how long you will be covered. Unfortunately, understanding how these benefit periods work is not always clear cut.
How long does Medicare last?
Your Medicare benefit period starts the day you are hospitalized as an inpatient and ends once you have been out of the hospital or a skilled nursing facility for 60 days.
How often do you pay a Medicare deductible?
Most health insurance plans have you pay a deductible once a year. With Medicare, you could face multiple Part A deductibles over the course of the year depending on your need for hospital care. It is important to understand that the Medicare benefit period applies to inpatient hospital stays only.
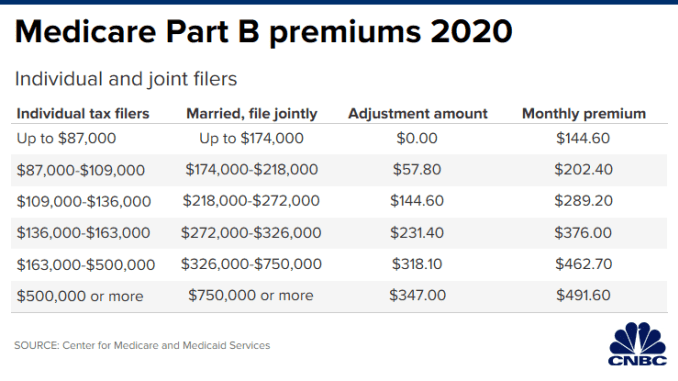
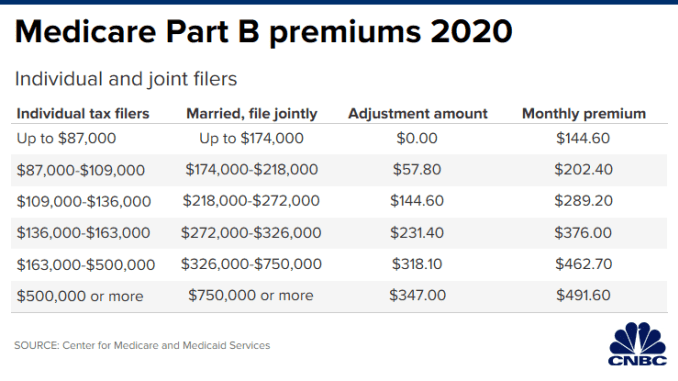
What is the Medicare deductible for 2020?
In 2020, the Part A deductible is $1,408. Any physician fees, however, will be charged to Medicare Part B and are not included as part of the Part A benefit.
How long do you have to be in a skilled nursing facility to be eligible for Medicare?
You also must enter a Medicare-certified skilled nursing facility within 30 days after leaving the hospital. In order for Medicare to pay for care in a skilled nursing facility (SNF), you first have to be hospitalized as an inpatient.
What are the 60-60-60-30 rules?
Understanding the 60-60-60-30 rules can help you to make sense of them. Know how much you are expected to pay and how much Medicare will cover. It may encourage you to consider enrolling in a Medigap plan for healthcare savings down the road.
How long does Medicare reserve days last?
Medicare offers you 60 lifetime reserve days to extend your Medicare benefit period. Any hospital stays lasting longer than 91 days will require use of lifetime reserve days. These reserve days cost $704 per hospital day in 2020. Medicare only allows you 60 lifetime reserve days total.
What is a Medicare benefit period?
A benefit period is how Original Medicare measures your use of hospital and SNF services. 1 It begins the day you're admitted as an inpatient in a hospital or SNF and ends when you haven't received any inpatient hospital care (or skilled care in an SNF) for 60 days in a row.
Medicare benefit period and Original Medicare Part A deductible
Unlike other types of health insurance, the deductible for a Medicare benefit period is not based on the calendar year. Instead, you pay a separate deductible for each benefit period—meaning you could pay more than one deductible in the same year.
Benefit period examples
To help you get a better understanding, here are 2 realistic examples:
The bottom line
Knowing how a benefit period works can help you understand your Medicare expenses. To learn more, check out this article on understanding Medicare's out-of-pocket costs.
What is a benefit period?
A benefit period is the way the Original Medicare program measures your use of inpatient hospital and skilled nursing facility (SNF) services. It begins the day that you enter a hospital or SNF and ends when you have not received inpatient hospital or Medicare-covered skilled care in a SNF for 60 days in a row.
When do you have to pay Part A deductible?
You must meet your Part A deductible at the beginning of each benefit period as well as pay a daily coinsurance depending on how many days you stay at the hospital or SNF during one benefit period.
How much is skilled nursing facility coinsurance?
Skilled nursing facility coinsurance: $0 for the first 20 days of inpatient care each benefit period; $161 per day for days 21-100. Let’s say you enter the hospital as an inpatient on May 1 and go home on May 15 (14 days in the hospital).
How long does it take to get a new benefit after leaving the hospital?
If you go into the hospital or SNF after one benefit period has ended (more than 60 days after you left), a new benefit period begins. There is no limit to the number of benefit periods you can have, or how long a benefit period can be.
Do you have to pay coinsurance for hospital?
In addition, since you will be on days 15-18 of your hospital benefit, you will not have to pay any coinsurance either. If you have questions about where you are in your benefit period, look at your most recent Medicare Summary Notice ...