What is PQRS and why should I participate?
The Physician Quality Reporting System (PQRS) has been using incentive payments, and will begin to use payment adjustments in 2015, to encourage eligible health care professionals (EPs) to report on specific quality measures. Why PQRS . PQRS gives participating EPs the opportunity to assess the quality of care they are providing to their
What is PQRS and why is it important?
The Physician Quality Reporting System (PQRS) was a reporting program of the Centers for Medicare and Medicaid Services (CMS). It gave eligible professionals (EPs) the opportunity to assess the quality of care they were providing to their patients, helping to ensure that patients get the right care at the right time.
What does PQRS stand for?
Formerly known as the Physician Quality Reporting Initiative (PQRI), the Physician Quality Reporting System (PQRS) was a voluntary reporting program that provided a financial incentive for certain health care professionals, including psychologists, who participated in Medicare to submit data on specified quality measures to the Centers for Medicare and Medicaid Services …
What are the PQRS requirements?
What is Medicare’s PQRS? (formerly PQRI) A voluntary individual reporting program that provides an incentive payment to eligible professionals (EPs) who satisfactorily report data on quality measures for covered Physician Fee Schedule (PFS) services furnished to Medicare Part B beneficiaries. What is the Incentive Payment?

What is a function of the PQRS?
The PQRS measures address various aspects of care, such as prevention, chronic- and acute-care management, care processes and procedures, resource utilization, and care coordination.Oct 30, 2015
What is PQRS stand for?
PQRS stands for the Physician Quality Reporting System. This program, which began is 2007, provides an incentive payment for eligible physicians who satisfactorily report data on quality measures for covered PFS services furnished to Medicare Part B Fee-for-Service beneficiaries.
What is a PQRS adjustment?
Physician Quality Reporting System. The Physician Quality Reporting System (PQRS) applies negative payment adjustments to eligible professionals who fail to satisfactorily report data on quality measures for covered services provided to Medicare Part B fee-for-service beneficiaries.
Is PQRS and MIPS the same thing?
How Is MIPS Different From PQRS? Because MIPS streamlines PQRS, the VM Program and the Medicare EHR Incentive Program, it is more comprehensive and extensive than PQRS alone. MIPS performance is measured by four categories — Quality, Improvement Activities, Promoting Interoperability and Cost.
What replaced PQRS?
A new quality program, the Merit-Based Incentive Payment System (MIPS), will replace PQRS on January 1, 2017.May 1, 2016
What is a physician quality reporting system PQRS now known as MIPS and who created it?
Background. The PQRS is one of several long-term quality initiatives developed by the Centers for Medicare and Medicaid Services (CMS). It is intended to, among other things; obtain information on the quality of care across the healthcare system.
What is MIPS healthcare?
The Merit-Based Incentive Payment System (MIPS) is the program that will determine Medicare payment adjustments. Using a composite performance score, eligible clinicians (ECs) may receive a payment bonus, a payment penalty or no payment adjustment. Look up if you need to participate in MIPS.
What is PQRS in healthcare?
Physician Quality Reporting System (PQRS) The Physician Quality Reporting System (PQRS) was a reporting program of the Centers for Medicare and Medicaid Services (CMS). It gave eligible professionals (EPs) the opportunity to assess the quality of care they were providing to their patients, helping to ensure that patients get the right care at ...
What is the most common method of reporting nuclear medicine?
The most common method the Nuclear Medicine community has for reporting measures is individual measures reporting. The three mechanisms that can be used to report these measures are described below:
What is PQRS in medical terms?
What is the Physician Quality Reporting System ? Formerly known as the Physician Quality Reporting Initiative (PQRI), the Physician Quality Reporting System (PQRS) was a voluntary reporting program that provided a financial incentive for certain health care professionals, including psychologists, who participated in Medicare to submit data on ...
When did PQRS end?
PQRS ended as a stand-alone program on Dec. 31. 2016; the PQRS quality measures became part of the Merit-based Incentive Payment System (MIPS) in 2017.
What is PQRS program?
PQRS is a reporting program that uses a combination of incentive payments and payment adjustments to promote reporting of quality information by eligible professionals (EPs). The program provides an incentive payment to practices with EPs (identified on claims by their individual National Provider Identifier [NPI] and Tax Identification Number ...
What is consent to monitoring?
Consent to Monitoring. Warning: you are accessing an information system that may be a U.S. Government information system. If this is a U.S. Government information system, CMS maintains ownership and responsibility for its computer systems. Users must adhere to CMS Information Security Policies, Standards, and Procedures.
What is CDT used for?
Use of CDT is limited to use in programs administered by Centers for Medicare & Medicaid Services (CMS). You agree to take all necessary steps to ensure that your employees and agents abide by the terms of this agreement. You acknowledge that the ADA holds all copyright, trademark and other rights in CDT.
Is Noridian Medicare copyrighted?
Some of the Provider information contained on the Noridian Medicare web site is copyrighted by the American Medical Association, the American Dental Association, and/or the American Hospital Association. This includes items such as CPT codes, CDT codes, ICD-10 and other UB-04 codes.
What is Lindsey's job?
Lindsey works with healthcare providers and hospitals to advance the use of electronic health records (EHR) to improve patient care and health outcomes. She consults with physician practices and hospitals to successfully implement and meaningfully use EHRs, including assistance associated with vendor products, hardware, software and system configuration and troubleshooting, staffing considerations, workflow analysis, EHR utilization, security and privacy, and quality data reporting from EHR systems.
What is a PQRS negative payment adjustment?
A quality reporting program that uses negative payment adjustments to promote reporting of quality information by individual eligible professionals (EPs) and group practices. Those who do not satisfactorilyreport data on quality measures for covered Medicare Physician Fee Schedule (MPFS) services furnished to Medicare Part B beneficiaries (including Railroad Retirement Board, Medicare Secondary Payer, and Critical Access Hospitals [CAH] method II) will be subject to a negative payment adjustment under PQRS. Medicare Part C–Medicare Advantage beneficiaries are not included.
What is CMS collaborating with?
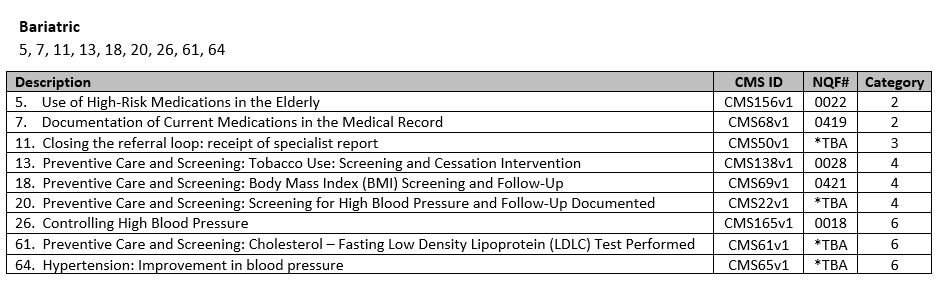
CMS is collaborating with specialty societies to ensure that the measures represented within Specialty Measure Sets accurately illustrate measures associates within a particular clinical area (suggested, NOT required); the following were established in 2015:
What is a VBM?
The Value Based Modifier (VBM) program will assess the PQRS quality data and Medicare cost data to calculate a provider’s overall VBM score and apply an upward, downward or neutral payment adjustment that will reflect payments in 2017.
What is PFS in Medicare?
Provides differential payment to a physician or group of physicians under the Medicare Physician Fee Schedule (PFS) based upon the quality of care furnished compared to the cost of care during a performance period.
What is MU in Medicare?
This category replaces the Medicare Electronic Health Record (EHR) Incentive Program for eligible professionals – also known as Meaningful Use (MU). It will account for 25% of your Final Score in 2017. Note: Hospital and Medicaid Meaningful Use are continued.
How many points do you need to get into MIPS?
It’s important to remember that the first year of MIPS is a transition year. You will only need to earn three points to avoid a penalty, and it will be easy to earn a small incentive.
When does MIPS apply?
MIPS most likely applies to you in the first year if you are a physician (MD/DO and DMD/DDS), PA, NP, clinical nurse specialist or a certified registered nurse anesthetist not participating in an Advanced Alternative Payment Model (APM).
