What is the purpose of prior authorization?
What is meant by prior authorization?
How do I find my Medicare authorization?
What is the difference between pre authorization and prior authorization?
Why does my medication need a prior authorization?
Who is responsible for getting pre authorization?
How do I get a prior authorization for medication?
- Call your physician and ensure they have received a call from the pharmacy.
- Ask the physician (or his staff) how long it will take them to fill out the necessary forms.
- Call your insurance company and see if they need you to fill out any forms.
How long does it take for Medicare to approve a procedure?
How do I know if Medicare will cover a procedure?
What services typically require prior authorizations?
- MRI/MRAs.
- CT/CTA scans.
- PET scans.
- Durable Medical Equipment (DME)
- Medications and so on.
What happens if a prior authorization is denied?
How long does prior authorization for medication take?
What services do you need prior authorization for?
The services most often requiring prior approval are durable medical equipment, skilled nursing facility stays, and Part B drugs.
What does prior authorization mean?
Prior authorization means your doctor must get approval before providing a service or prescribing a medication. Now, when it comes to Advantage and Part D, coverage is often plan-specific. Meaning, you should contact your plan directly to confirm coverage.
How to know if your treatment requires approval?
Refer to your plan documents, including the drug formulary, to see if your treatment requires approval. This information should be on your plan’s website. The Medicare & You handbook also contains more information.
Does Medicare cover MRI?
If the purpose of the MRI is to treat a medical issue, and all providers involved accept Medicare assignment, Part B would cover the inpatient procedure. An Advantage beneficiary might need prior authorization to visit a specialist such as a radiologist.
Do you need prior authorization for Medicare Part B?
Part B covers the administration of certain drugs when given in an outpatient setting. As part of Medicare, you’ll rarely need to obtain prior authorization. Although, some meds may require your doctor to submit a Part B Drug Prior Authorization Request Form. Your doctor will provide this form.
Does Medicare Advantage cover out of network care?
Unfortunately, if Medicare doesn’t approve the request, the Advantage plan typically doesn’t cover any costs, leaving the full cost to you.
Do you need a Part B prior authorization form?
Although, some meds may require your doctor to submit a Part B Drug Prior Authorization Request Form. Your doctor will provide this form. Once the request gets approval, coverage begins.
How does prior authorization work?
Prior authorization works by having your health care provider or supplier submit a prior authorization form to their Medicare Administrator Contractor (MAC). They must then wait to receive a decision before they can perform the Medicare services in question or prescribe the prescription drug being considered.
Why do we need prior authorization?
Prior authorization can help protect a beneficiary’s rights to covered Medicare benefits, and it can also act as a means of reducing improper billing, waste and fraud within the Medicare system . It also helps to cut down on over-utilization of unnecessary care.
Does Medicare have prior authorization?
Medicare coverage contains a lot of qualifiers, exceptions and other criteria. Prior authorization addresses much of the same information required for submitting Medicare claims or filing Medicare appeals, but it does so earlier in the process before the services are provided.
Does Medicare Advantage require prior authorization?
Medicare Advantage plans may sometimes require prior authorization for things like non-emergency hospital care outside of your plan provider network, visiting specialists and some other services.
Do you have to file a claim for Medicare?
In some instances, you may have to file a Medicare claim for care that you already received. This ensures that your health care provider is properly reimbursed and that you aren’t charged for more out-of-pocket Medicare costs than you actually owe.
Do you need prior authorization for Medicare Part C?
It’s not uncommon, however, for beneficiaries of Medicare Advantage (Medicare Part C) plans and Medicare Part D Prescription Drug plans to need prior authorization before receiving some types of care. Prior authorization is most common for getting certain prescription drugs covered by your plan.
What is prior authorization?
Healthcare.gov defines prior authorization as “approval from a health plan that may be required before you get a service or fill a prescription in order for the service or prescription to be covered by your plan”. The general process has many names including precertification, pre-authorization, prior approval, and predetermination.
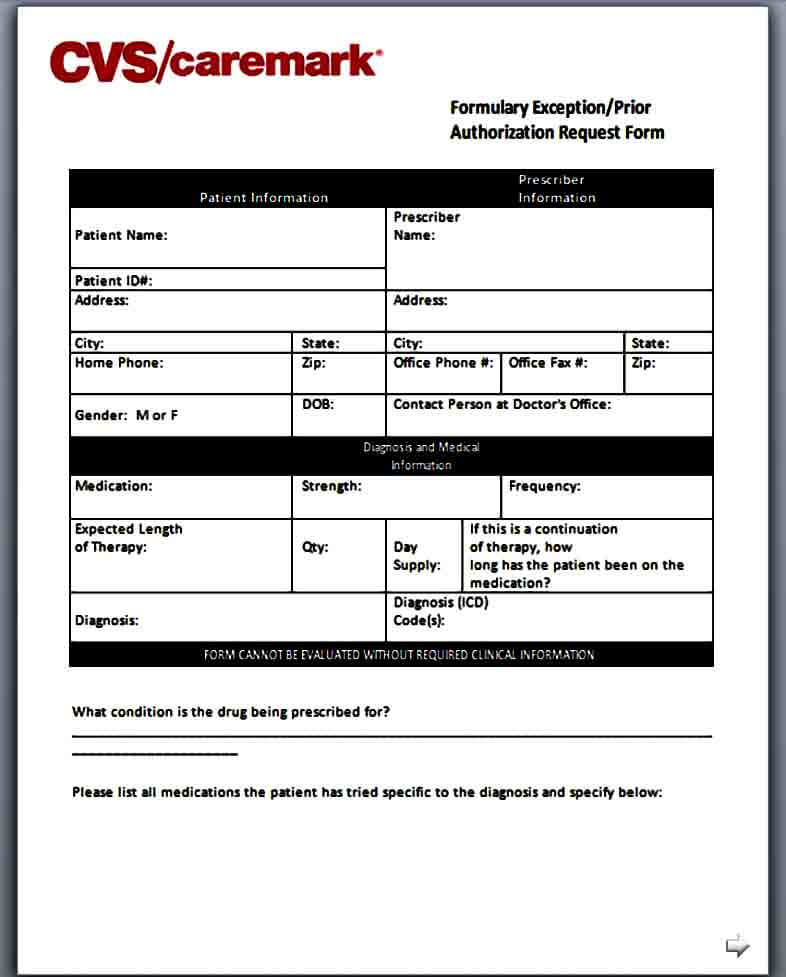
How to get prior authorization for a medication?
When it comes to a medication prior authorization, the process typically starts with a prescriber ordering a medication for a patient. When this is received by a pharmacy, the pharmacist will be made aware of the prior authorization status of the medication. At this point, they will alert the prescriber or physician. With this notification, the physician’s office will start the prior authorization process. They will collect the information needed for the submission of PA forms to the patient’s insurance. This can be done via automated messages, fax, secure email, or phone.
Why do insurance companies require prior authorization?
These prior authorizations save money for insurers by bypassing unnecessary or expensive treatment options when other equally effective options exist that are included in the plan’s formulary. The formulary includes the list of medications that are covered under an insurance plan. This process is needed not only to ensure minimizing prescription costs, but also to verify that what is being prescribed is medically necessary and appropriate for the patient.
Why do insurance companies update their formularies?
Insurance companies continually update their formularies to include drugs that are most effective to treat different disease states that are also cost effective. This ensures that medications that are covered by plans will reflect guideline changes. Prior authorizations also verify that certain medications aren’t being duplicated if patients see multiple specialists. This keeps patients safe from potential adverse effects and encourages appropriate medication usage.
Why is it important to have a prior authorization certified specialist?
There are great benefits to having a Prior Authorization Certified Specialist on staff to help with the administrative process.
Why is prior authorization important?
It is also be important to have good documentation policies. If a prior authorization requires step therapy in its criteria, each trial will need to be documented.
What is a PA?
Prior authorization (prior auth, or PA) is a management process used by insurance companies to determine if a prescribed product or service will be covered. This means if the product or service will be paid for in full or in part. This process can be used for certain medications, procedures, or services before they are given to the patient.
What is pre claim review?
Under pre-claim review, the provider or supplier submits the pre-claim review request and receives the decision prior to claim submission; however, the provider or supplier can render services before submitting the request. A provider or supplier submits either the prior authorization request or pre-claim review request with all supporting medical ...
How does a preclaim review work?
Under pre-claim review, the provider or supplier submits the pre-claim review request and receives the decision prior to claim submission; however, the provider or supplier can render services before submit ting the request. A provider or supplier submits either the prior authorization request or pre-claim review request with all supporting medical documentation for provisional affirmation of coverage for the item or service to their Medicare Administrator Contractor (MAC). The MAC reviews the request and sends the provider or supplier an affirmed or non-affirmed decision.
What is CMS in Medicare?
The Centers for Medicare & Medicaid Services (CMS) runs a variety of programs that support efforts to safeguard beneficiaries’ access to medically necessary items and services while reducing improper Medicare billing and payments. Through prior authorization and pre-claim review initiatives, CMS helps ensure compliance with Medicare rules.
When will OPDs receive notice of exemption?
Hospital OPD providers who met the affirmation rate threshold of 90% or greater will receive a written Notice of Exemption no later than March 1, 2021. Those hospital OPDs will be exempt from submitting prior authorization requests for dates of service beginning May 1, 2021.
What is the CMS 1736-FC?
As part of the Calendar Year 2021 Outpatient Prospective Payment System/Ambulatory Surgical Center Final Rule (CMS-1736-FC), CMS is adding Implanted Spinal Neurostimulators and Cervical Fusion with Disc Removal to the nationwide prior authorization process for hospital outpatient department (OPD) services, effective July 1, 2021. These two services will be in addition to the existing list of services requiring prior authorization, which include blepharoplasty, botulinum toxin injection, rhinoplasty, panniculectomy, and vein ablation.
What is the HCPCS code for ear cartilage grafting?
CMS is removing HCPCS code 21235 (Obtaining ear cartilage for grafting) from the list of codes that require prior authorization as a condition of payment, because it is more commonly associated with procedures unrelated to rhinoplasty that are not likely to be cosmetic in nature. The updated list of codes that require prior authorization as a condition of payment can be found below.
Does prior authorization for OPD help Medicare?
CMS believes prior authorization for certain hospital OPD services will ensure that Medicare beneficiaries continue to receive medically necessary care – while protecting the Medicare Trust Fund from improper payments and, at the same time, keeping the medical necessity documentation requirements unchanged for providers.
Phone
For specific billing questions and questions about your claims, medical records, or expenses, log into your secure Medicare account, or call us at 1-800-MEDICARE.
1-800-MEDICARE (1-800-633-4227)
For specific billing questions and questions about your claims, medical records, or expenses, log into your secure Medicare account, or call us at 1-800-MEDICARE.
