Medicare’s Recovery Process
- Reporting the case to the BCRC: Whenever there is a pending liability, no-fault, or workers’ compensation case, it...
- BCRC issues a Rights and Responsibilities letter: After the MSP occurrence is posted, the BCRC will send you the...
- BCRC identifies Medicare’s interim recovery amount and issues the CPL: The BCRC begins identifying...
What is Medicare Secondary Payer recovery?
you owe Medicare, as well as your right to an appeal or waiver. Medicare Secondary Payer rules say that liability insurance (including self-insurance), no-fault insurance, and workers’ compensation must pay for medical items and services before Medicare pays. However, Medicare makes “conditional payments” (payments made to make
What is BCRC Medicare?
The Benefits Coordination & Recovery Center (BCRC) consolidates the activities that support the collection, management, and reporting of other insurance coverage for Medicare beneficiaries.
How to get secondary insurance for Medicare?
- Vision: Your medical plan will not cover you for vision care. ...
- Dental: A dental plan can cover you for preventive care such as routine teeth cleanings and some X-rays. ...
- Disability: Short- and long-term disability plans are a type of secondary insurance coverage. ...
What is Medicare reimbursement policy?
The itemized bill must contain the following information:
- Date of service
- Place of service
- The charge for each service
- Description of your illness or injury
- Description of the medical and surgical supplies
- The name and address of the doctor or supplier
- The doctor or supplier’s National Provider Identifier Number, if you know it.
Do you ever have to pay Medicare back?
The payment is "conditional" because it must be repaid to Medicare if you get a settlement, judgment, award, or other payment later. You're responsible for making sure Medicare gets repaid from the settlement, judgment, award, or other payment.
What does MSP recovery do?
Recovery Specialists MSP Recovery is the leading Medicaid and Medicare Secondary Payer Act Recovery Specialist. MSP has the most comprehensive platform to recover on any claims where the law places primary payment responsibility on another payer.
What is Medicare Secondary Payer Recovery?
The Medicare Secondary Payer Recovery Portal (MSPRP) is a web-based tool designed to assist in the resolution of liability insurance, no-fault insurance, and workers' compensation Medicare recovery cases. The MSPRP gives you the ability to access and update certain case specific information online.
Why would I be getting a letter from CMS?
In general, CMS issues the demand letter directly to: The Medicare beneficiary when the beneficiary has obtained a settlement, judgment, award or other payment.
Who owns MSP recovery?
CEO John H. RuizMSP Recovery CEO John Ruiz speaks on Bloomberg Television. 10:04 a.m. in New York, less than an hour after its debut. MSP Recovery Founder and CEO John H. Ruiz speaks with Kriti Gupta and Jon Erlichman on “Bloomberg Markets.” John H. Ruiz, 55, owns a 65% stake in the company.
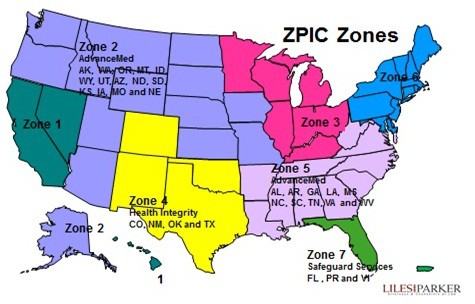
What is CRC MSP?
The MSP CRC is a single contractor with national jurisdiction that became fully operational in the second quarter of FY 2014. The CMS, through its Coordination of Benefits & Recovery (COB&R) program, routinely collects data on other insurance coverage for Medicare beneficiaries.
How far back can Medicare recoup payments?
(1) Medicare contractors can begin recoupment no earlier than 41 days from the date of the initial overpayment demand but shall cease recoupment of the overpayment in question, upon receipt of a timely and valid request for a redetermination of an overpayment.
Does Medicare automatically send claims to secondary insurance?
Medicare will send the secondary claims automatically if the secondary insurance information is on the claim. As of now, we have to submit to primary and once the payments are received than we submit the secondary.
Does Medicare pay first or second?
Medicare pays first and your group health plan (retiree) coverage pays second . If the employer has 100 or more employees, then the large group health plan pays first, and Medicare pays second .
How does Medicare calculate final demand?
Step number two: take the gross settlement amount and subtract the total procurement cost to determine Medicare's final lien demand.
What is a CMS notice?
CMS model notices contain all of the elements CMS requires for proper notification to enrollees or non-contract providers, if applicable. Plans may modify the model notices and submit them to the appropriate CMS regional office for review and approval. Plans may use these notices at their discretion.
What is a CMS approval letter?
This letter is to inform you that the Centers for Medicare and Medicaid Services (CMS) has approved the attached evaluation design for the Whole Person Care (WPC) Pilots authorized under the section 111 S(a) demonstration entitled "Medi-Cal 2020" (11-W-00193/9), as submitted by the state and as modified through our ...
How to release information from Medicare?
Medicare does not release information from a beneficiary’s records without appropriate authorization. If you have an attorney or other representative , he or she must send the BCRC documentation that authorizes them to release information. Your attorney or other representative will receive a copy of the RAR letter and other letters from the BCRC as long as he or she has submitted a Consent to Release form. A Consent to Release (CTR) authorizes an individual or entity to receive certain information from the BCRC for a limited period of time. With that form on file, your attorney or other representative will also be sent a copy of the Conditional Payment Letter (CPL) and demand letter. If your attorney or other representative wants to enter into additional discussions with any of Medicare’s entities, you will need to submit a Proof of Representation document. A Proof of Representation (POR) authorizes an individual or entity (including an attorney) to act on your behalf. Note: In some special circumstances, the potential third-party payer can submit Proof of Representation giving the third-party payer permission to enter into discussions with Medicare’s entities. If potential third-party payers submit a Consent to Release form, executed by the beneficiary, they too will receive CPLs and the demand letter. It is in the best interest of both sides to have the most accurate information available regarding the amount owed to the BCRC. Please see the following documents in the Downloads section at the bottom of this page for additional information: POR vs. CTR, Proof of Representation Model Language and Consent to Release Model Language.
What happens if a BCRC determines that another insurance is primary to Medicare?
If the BCRC determines that the other insurance is primary to Medicare, they will create an MSP occurrence and post it to Medicare’s records. If the MSP occurrence is related to an NGHP, the BCRC uses that information as well as information from CMS’ systems to identify and recover Medicare payments that should have been paid by another entity as primary payer.
How to remove CPL from Medicare?
If you or your attorney or other representative believe that any claims included on CPL/PSF or CPN should be removed from Medicare's interim conditional payment amount, documentation supporting that position must be sent to the BCRC. This process can be handled via mail, fax, or the MSPRP. Click the MSPRP link for details on how to access the MSPRP. The BCRC will adjust the conditional payment amount to account for any claims it agrees are not related to the case.
How long does it take for a BCRC to send a CPL?
Within 65 days of the issuance of the RAR Letter, the BCRC will send the CPL and Payment Summary Form (PSF). The PSF lists all items or services that Medicare has paid conditionally which the BCRC has identified as being related to the pending case.
What is BCRC in Medicare?
The BCRC begins identifying claims that Medicare has paid conditionally that are related to the case, based upon details about the type of incident, illness or injury alleged. Medicare's recovery case runs from the “date of incident” through the date of settlement/judgment/award (where an “incident” involves exposure to or ingestion of a substance over time, the date of incident is the date of first exposure/ingestion).
How long does it take for a CPN to be reviewed?
If a response is received within 30 calendar days, it will be reviewed and the BCRC will issue a demand (request for repayment) as applicable. If a response is not received in 30 calendar days , a demand letter will automatically be issued without any reduction for fees or costs. For more information about the CPN, refer to the document titled Conditional Payment Notice (Beneficiary) in the Downloads section at the bottom of this page.
What is a BCRC termination date?
The BCRC will apply a termination date (generally the date of settlement, judgment, award, or other payment ) to the case. The BCRC will identify any new, related claims that have been paid since the last time the CPL was issued up to and including the settlement/judgment/award date. Once this process is complete, the BCRC will issue a formal recovery demand letter advising you of the amount of money owed to the Medicare program. The amount of money owed is called the demand amount. The demand letter includes the following:
Does Medicare require proof of representation?
Medicare works to protect your privacy. We are not allowed to communicate with anyone other than you about your recovery case unless you tell us to do so. If you have a representative, BCRC will need a signed Proof of Representation or Authorization.
Does Medicare pay attorney fees?
be repaid. Medicare reduces the fnal demand amount based on attorney fees and costs you have incurred. A Demand Letter is then issued, which explains how the BCRC calculated the amount
What does a Recovery Audit Contractor (RAC) do?
RAC's review claims on a post-payment basis. The RAC's detect and correct past improper payments so that CMS and Carriers, FIs, and MACs can implement actions that will prevent future improper payments.
What Topics do RAC's Review?
Stay in the know on proposed and approved topics that RAC's are able to review. These topics will be updated monthly on the RAC reviews topic page and include:
What is Medicare Secondary Payer?
The Medicare Secondary Payer (MSP) program is in place to ensure that Medicare is aware of situations where it should not be the primary, or first, payer of claims. If a beneficiary has Medicare and other health insurance, Coordination of Benefits (COB) rules decide which entity pays first. There are a variety of methods ...
Who is responsible for mistaken Medicare payment?
Based on this new information, CMS takes action to recover the mistaken Medicare payment. The BCRC is responsible for the recovery of mistaken liability, no-fault, and workers’ compensation (collectively referred to as Non-Group Health Plan or NGHP) claims where the beneficiary must repay Medicare.
What is Medicare beneficiary?
The Medicare beneficiary when the beneficiary has obtained a settlement, judgment, award or other payment. The liability insurer (including a self-insured entity), no-fault insurer, or workers’ compensation (WC) entity when that insurer or WC entity has ongoing responsibility for medicals (ORM). For ORM, there may be multiple recoveries ...
What happens if you don't respond to a debt recovery?
Failure to respond within the specified time frame may result in the initiation of additional recovery procedures, including the referral of the debt to the Department of Justice for legal action and/or the Department of the Treasury for further collection actions.
How long does interest accrue?
Interest accrues from the date of the demand letter, but is only assessed if the debt is not repaid or otherwise resolved within the time period specified in the recovery demand letter. Interest is due and payable for each full 30-day period the debt remains unresolved; payments are applied to interest first and then to the principal. Interest is assessed on unpaid debts even if a debtor is pursuing an appeal or a beneficiary is requesting a waiver of recovery; the only way to avoid the interest assessment is to repay the demanded amount within the specified time frame. If the waiver of recovery or appeal is granted, the debtor will receive a refund.
What is included in a demand letter for Medicare?
The demand letter also includes information on administrative appeal rights. For demands issued directly to beneficiaries, Medicare will take the beneficiary’s reasonable procurement costs (e.g., attorney fees and expenses) into consideration when determining its demand amount.
How long does it take to appeal a debt?
The appeal must be filed no later than 120 days from the date the demand letter is received. To file an appeal, send a letter explaining why the amount or existence of the debt is incorrect with applicable supporting documentation.
Does a waiver of recovery apply to a demand letter?
Note: The waiver of recovery provisions do not apply when the demand letter is issued directly to the insurer or WC entity. See Section 1870 of the Social Security Act (42 U.S.C. 1395gg).
Can Medicare waive recovery of demand?
The beneficiary has the right to request that the Medicare program waive recovery of the demand amount owed in full or in part. The right to request a waiver of recovery is separate from the right to appeal the demand letter, and both a waiver of recovery and an appeal may be requested at the same time. The Medicare program may waive recovery of the amount owed if the following conditions are met:
What happens if you enroll in a Medicaid plan through the exchange?
If they try to enroll in a plan through the health insurance exchanges, they will be directed to the Medicaid system instead, based on their income. In states that have MERP that go beyond long-term care costs, this has resulted in some people being caught off-guard by the estate recovery programs.
What was the impact of Obamacare?
Impact of Obamacare. The expansion of Medicaid under the Affordable Care Act (ACA), also known as Obamacare, pushed the issue of Medicaid estate recovery to the foreground in states that had strict estate recovery programs in place.
What happens if a state doesn't use Medicaid?
If a state does not use Medicaid managed care, they are not allowed to recoup more than the actual amount the state spent on the person's care. All states try to recover from estate assets that pass through probate, but some states also try to recover from other assets. 10.
What happens if you need care that exceeds your insurance?
If you eventually need care that exceeds the benefits of your policy, a portion of the cost of your care will be protected from estate recovery.
Can Medicaid beneficiaries recover money from their heirs?
And if the Medicaid beneficiary was truly without any assets at all, the estate recovery program won't be able to recover anything, as they cannot attempt to recover the money from the beneficiary's heirs (they can use the estate recovery process to recoup assets that may have passed to a surviving spouse, but only after that spouse has passed away as well).
Is the ACA based on income?
Like expanded Medicaid, eligibility for the ACA's premium subsidies (premium tax credits) is also based only on income, without regard for assets. And premium subsidies to offset the cost of private coverage are not available to those who are eligible for Medicaid. 6 .
Can you get Medicaid back after you die?
Medicaid, the state/federal health coverage program for low-income people, may take its money back from your estate after you die. It can do so if you received Medicaid-funded long-term care after the age of 55. In some states, this can happen if you received Medicaid-funded services before the age of 55 if you were permanently institutionalized, ...
What is estate recovery for Medicaid?
For individuals age 55 or older, states are required to seek recovery of payments from the individual's estate for nursing facility services, home and community-based services, and related hospital and prescription drug services.
Can you recover Medicaid from a deceased spouse?
States may not recover from the estate of a deceased Medicaid enrollee who is survived by a spouse, child under age 21, or blind or disabled child of any age. States are also required to establish procedures for waiving estate recovery when recovery would cause an undue hardship.
