When to use modifier TC in JL in Medicare?
Medicare JL. Providers in DC, DE, MD, NJ & PA. Modifier TC is used when only the technical component of a procedure is being billed when certain services combine both the professional and technical portions in one procedure code. Use modifier TC when the physician performs the test but does not do the interpretation.
What is a Medicare fee schedule?
Fee Schedules - General Information | CMS A fee schedule is a complete listing of fees used by Medicare to pay doctors or other providers/suppliers. This comprehensive listing of fee maximums is used to reimburse a physician and/or other providers on a fee-for-service basis.
What is a Medicare reimbursement rate for CPT codes?
A Medicare reimbursement rate is the amount of money that Medicare pays doctors and other health care providers for the services and items they administer to Medicare beneficiaries. CPT codes are the numeric codes used to identify different medical services, procedures and items for billing purposes.
How do I find Medicare reimbursement rates?
You can also find Medicare reimbursement rates if you know the CPT or HCPCS code for the service or item being billed and have access to the Medicare Physician Fee Schedule, which is essentially a master list of all reimbursement rates. The MPFS is updated on a quarterly basis to reflect the most recent changes to reimbursement rates.
How do I find Medicare reimbursement rates?
You can search the MPFS on the federal Medicare website to find out the Medicare reimbursement rate for specific services, treatments or devices. Simply enter the HCPCS code and click “Search fees” to view Medicare's reimbursement rate for the given service or item.
What is Medicare reimbursement rate?
According to the Centers for Medicare & Medicaid Services (CMS), Medicare's reimbursement rate on average is roughly 80 percent of the total bill. 1. Not all types of health care providers are reimbursed at the same rate.
How much does Medicare reimburse per RVU?
On the downside, CMS set the 2022 conversion factor (i.e., the amount it pays per RVU) at $33.59, which is $1.30 less than the 2021 conversion factor. There was also mixed news on telehealth.
How much does Medicare reimburse for a 99213?
The most common codes a doctor will use for follow up office visits are 99213 (follow up office visit, low complexity) and 99214 (follow up office visit, moderate complexity). A 99213 pays $83.08 in this region ($66.46 from Medicare and $16.62 from the patient).
What is the reimbursement rate for?
Reimbursement rates means the formulae to calculate the dollar allowed amounts under a value-based or other alternative payment arrangement, dollar amounts, or fee schedules payable for a service or set of services.
Is the Medicare 2021 fee schedule available?
The CY 2021 Medicare Physician Fee Schedule Final Rule was placed on display at the Federal Register on December 2, 2020. This final rule updates payment policies, payment rates, and other provisions for services furnished under the Medicare Physician Fee Schedule (PFS) on or after Jan. 1, 2021.
How much is an RVU worth in 2021?
For each year, work RVUs and conversion factors of that specific year were applied to the formula, $36.04 for 2019 and $32.41 for 2021.
How is Medicare RVU calculated?
Basically, the relative value of a procedure multiplied by the number of dollars per Relative Value Unit (RVU) is the fee paid by Medicare for the procedure (RVUW = physician work, RVUPE = practice expense, RVUMP = malpractice)....ABBREVIATIONS:RVURelative Value UnitSGRSustainable Growth Rate6 more rows
What is the Medicare RVU for 2022?
The new 2022 conversion factor is $34.6062. (The conversion factor is multiplied by the RVUs to calculate the dollar reimbursement amount.) The estimated impact of these and other adjustments on the allergy/immunology specialty is 0.8% overall decrease in Medicare payments for 2022, compared to 2021.
How Much Does Medicare pay for 99214 in 2021?
$132.94By Christine Frey posted 12-09-2020 15:122021 Final Physician Fee Schedule (CMS-1734-F)Payment Rates for Medicare Physician Services - Evaluation and Management99213Office/outpatient visit est$93.5199214Office/outpatient visit est$132.9499215Office/outpatient visit est$185.9815 more rows•Dec 9, 2020
How Much Does Medicare pay for a level 3 office visit?
The Medicare allowable reimbursement (2021) for this visit is $113.75 and it is worth 1.6 work RVUs. This level of care requires low complexity MDM or a total of 30 - 44 minutes devoted to the encounter on the day of the visit.
What is Medicare approved amount for doctor visit?
Medicare's approved amount for the service is $100. A doctor who accepts assignment agrees to the $100 as full payment for that service. The doctor bills Medicare who pays him or her 80% or $80, and you are responsible for the 20% coinsurance (after you have paid the Part B annual deductible).
What is fee schedule?
A fee schedule is a complete listing of fees used by Medicare to pay doctors or other providers/suppliers. This comprehensive listing of fee maximums is used to reimburse a physician and/or other providers on a fee-for-service basis. Providers may access the most current fee schedules from the CMS link (s) below.
Does PC TC apply to physician services?
The concept of PC / TC does not apply since physician services cannot be split into professional and technical components. Modifiers 26 and TC cannot be used with these codes. The RVUS include values for physician work, practice expense and malpractice expense. There are some codes with no work RVU s.
When to use modifier TC?
Modifier TC is used when only the technical component of a procedure is being billed when certain services combine both the professional and technical portions in one procedure code. Use modifier TC when the physician performs the test but does not do the interpretation.
Can a technical component be billed separately?
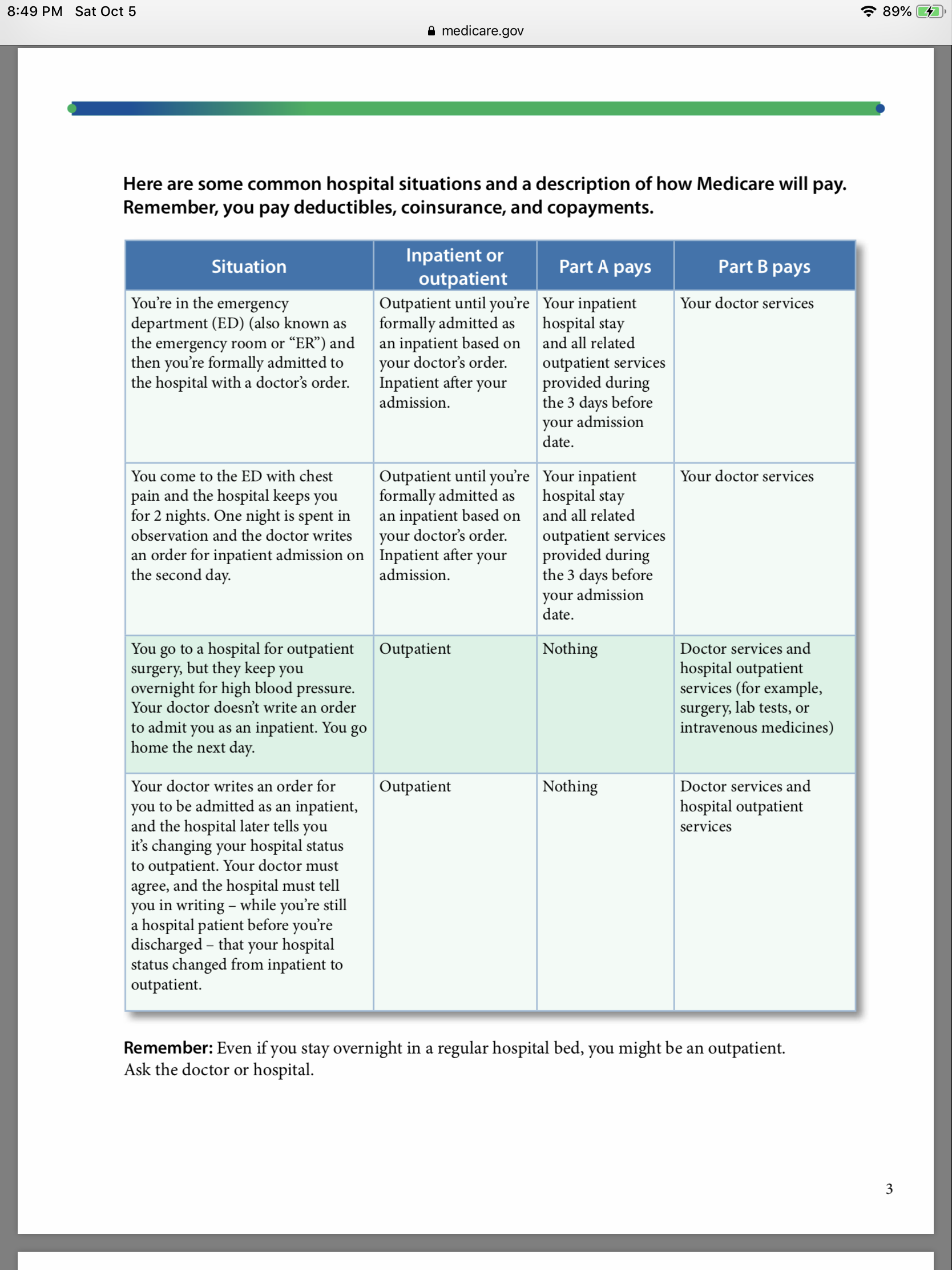
Technical component procedures are institutional and cannot be billed separately by the physician when the patient is: In a covered Part A stay in a skilled nursing facility (SNF) location. Inpatient. Outpatient.
What is CR 10882?
CR 10882 revises the “Medicare Claims Processing Manual”, Chapters 1 and 35, to add new sections on Global Billing and Separate TC/PC billing instructions. For both paper and electronic claims, when a global diagnostic service code is billed (for example, no modifier TC and no modifier -26), the address where the TC was performed must be reported on the claim. Global billing does not apply to anti-markup tests.
When TC and PC are billed separately, should providers report the name, address and NPI of the location where
When the TC and PC are billed separately (not billed globally), providers should report the name, address and NPI of the location where each component was performed. If the billing provider has an enrolled practice location at the address where the service was performed, the billing provider/supplier may report their own name, address and NPI in Items 32 and 32a (or the 837P electronic claim equivalent).
