The reimbursement rates are the monetary amounts that Medicare pays to health care providers, hospitals, laboratories, and medical equipment companies for performing certain services and providing medical supplies for individuals enrolled in Medicare insurance.
Full Answer
Who develops the Medicare reimbursement rates?
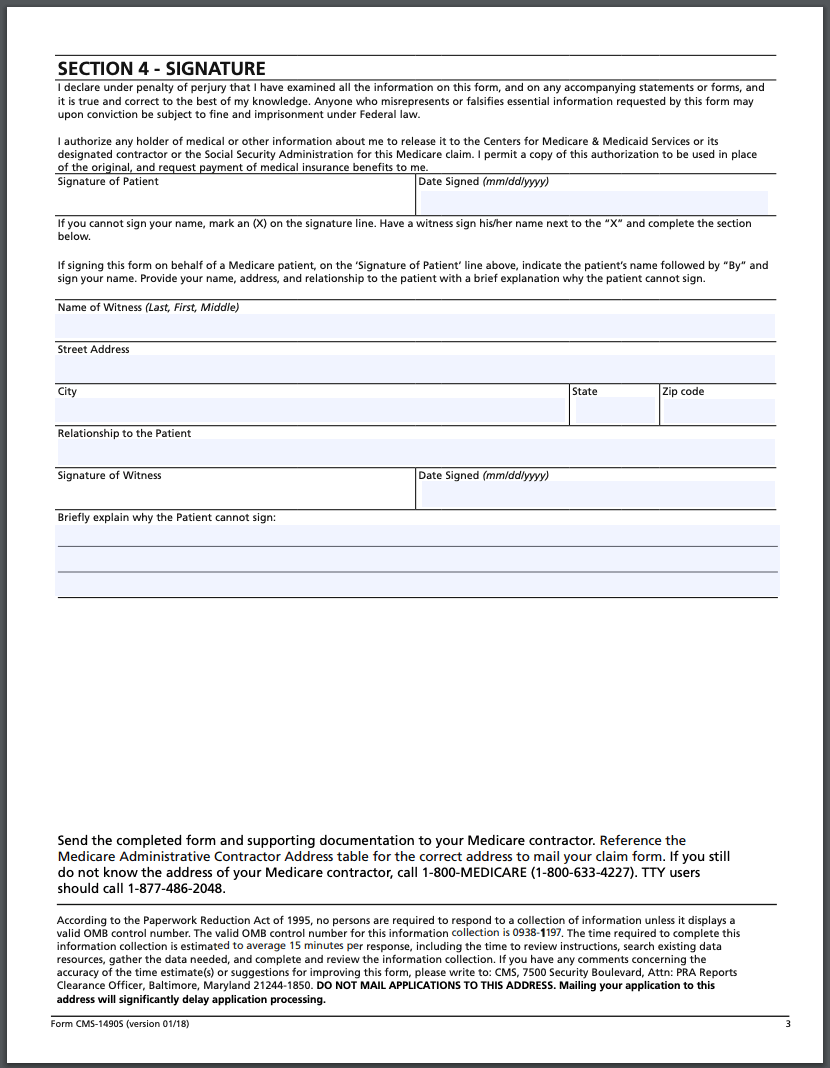
· For Medicare recipients, however, the system may work a little bit differently. When someone who receives Medicare benefits visits a physician’s office, they provide their Medicare information, and instead of making a payment, the bill gets sent to Medicare for reimbursement. There may be times when a patient with Medicare is responsible for ...
How do I receive reimbursement for my Medicare reimbursement account?
According to the Centers for Medicare & Medicaid Services (CMS), Medicare’s reimbursement rate on average is roughly 80 percent of the total bill. 1. Not all types of health care providers are reimbursed at the same rate. For example, clinical nurse specialists are reimbursed at 85% for most services, while clinical social workers receive 75%. 1.
What is the $800 Medicare reimbursement account?
Medicare Part A is free for most people. For Part B, you pay a premium. Basic Option members who have Medicare Part A and Part B can get up to $800 with a Medicare Reimbursement Account. All you have to do is provide proof that you pay Medicare Part B premiums. Each eligible active or retired member on a contract with Medicare Part A and Part B ...
What percentage of Medicare reimbursement do nurses receive?
· The reimbursement rates are the monetary amounts that Medicare pays to health care providers, hospitals, laboratories, and medical equipment companies for performing certain services and providing medical supplies for individuals enrolled in Medicare insurance. To receive reimbursement payments at the current rates established by Medicare, health care …
What does Medicare reimbursement mean?
Medicare reimbursement is the process by which a doctor or health facility receives funds for providing medical services to a Medicare beneficiary. However, Medicare enrollees may also need to file claims for reimbursement if they receive care from a provider that does not accept assignment.
What is a CMS reimbursement?
The Centers for Medicare and Medicaid (CMS) sets reimbursement rates for all medical services and equipment covered under Medicare. When a provider accepts assignment, they agree to accept Medicare-established fees. Providers cannot bill you for the difference between their normal rate and Medicare set fees.
How do you qualify for Medicare reimbursement?
You must be a retired member or qualified survivor who is receiving a pension and is eligible for a health subsidy, and enrolled in both Medicare Parts A and B. 2.
How do I find out my Medicare reimbursement rate?
You can search the MPFS on the federal Medicare website to find out the Medicare reimbursement rate for specific services, treatments or devices. Simply enter the HCPCS code and click “Search fees” to view Medicare's reimbursement rate for the given service or item.
Can my employer reimburse me for Medicare premiums?
In general, when an employee is eligible for Medicare due to age, an employer may reimburse his or her Medicare premiums only when: The employer's group health plan is a secondary payer to Medicare because the employer has fewer than 20 employees; AND.
What is reimbursement payment?
Reimbursement is compensation paid by an organization for out-of-pocket expenses incurred or overpayment made by an employee, customer, or another party.
How do you qualify to get $144 back from Medicare?
How do I qualify for the giveback?Are enrolled in Part A and Part B.Do not rely on government or other assistance for your Part B premium.Live in the zip code service area of a plan that offers this program.Enroll in an MA plan that provides a giveback benefit.
Why would I get a letter from CMS?
In general, CMS issues the demand letter directly to: The Medicare beneficiary when the beneficiary has obtained a settlement, judgment, award or other payment.
Is Medicare Part B reimbursement considered income?
The Medicare Part B reimbursement payments are not taxable to the retiree.
How do I calculate Medicare amount?
Thus, if the allowable fee is $100 for a participating provider, the allowable fee for a non-participating provider is $95. Medicare will pay 80% of the $95. If assignment is accepted the patient is responsible for 20% of the $95. If assignment is not accepted, the patient will pay out of pocket for the service.
What does CMS stand for?
The Centers for Medicare & Medicaid Services, CMS, is part of the Department of Health and Human Services (HHS).
Does Medicare reimbursement vary by state?
Over the years, program data have indicated that although Medicare has uniform premiums and deductibles, benefits paid out vary significantly by State of residence of the beneficiary. These variations are due in part to the fact that reimbursements are based on local physicians' prices.
What does CMS stand for?
The Centers for Medicare & Medicaid Services, CMS, is part of the Department of Health and Human Services (HHS).
How does Part B reimbursement work?
The Medicare Part B Reimbursement program reimburses the cost of eligible retirees' Medicare Part B premiums using funds from the retiree's Sick Leave Bank. The Medicare Part B reimbursement payments are not taxable to the retiree.
How long does a Medicare reimbursement take?
Claims processing by Medicare is quick and can be as little as 14 days if the claim is submitted electronically and it's clean. In general, you can expect to have your claim processed within 30 calendar days. However, there are some exceptions, such as if the claim is amended or filed incorrectly.
What percentage of Medicare is reimbursed?
According to the Centers for Medicare & Medicaid Services (CMS), Medicare’s reimbursement rate on average is roughly 80 percent of the total bill. 1. Not all types of health care providers are reimbursed at the same rate.
What does Medicare reimburse for?
Medicare reimburses health care providers for services and devices they provide to beneficiaries. Learn more about Medicare reimbursement rates and how they may affect you.
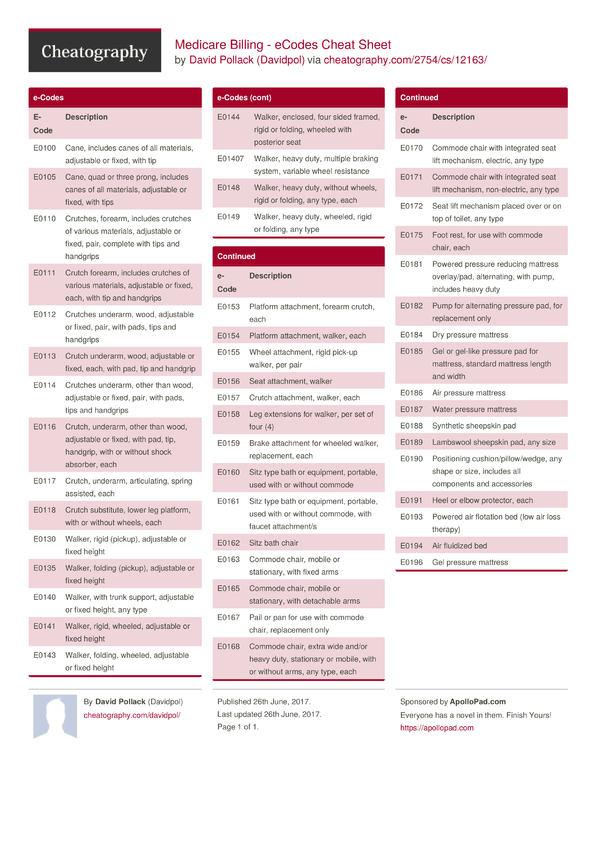
What is Medicare coded number?
Medicare uses a coded number system to identify health care services and items for reimbursement. The codes are part of what’s called the Healthcare Common Procedure Coding System (HCPCS).
How much back is Medicare Part A?
Basic Option members with Medicare Part A and Part B can get up to $800 back. Medicare Part A is free for most people. For Part B, you pay a premium. Basic Option members who have Medicare Part A and Part B can get up to $800 with a Medicare Reimbursement Account.
How much does Medicare Part A cost?
Medicare Part A is free for most people. For Part B, you pay a premium. Basic Option members who have Medicare Part A and Part B can get up to $800 with a Medicare Reimbursement Account. All you have to do is provide proof that you pay Medicare Part B premiums. Each eligible active or retired member on a contract with Medicare Part A and Part B, including covered spouses, can get their own $800 reimbursement.
How long does it take to get a reimbursement for $800?
There are no restrictions on how you can use your $800 reimbursement. Most claims will be reviewed within one to two business days after they have been received. Upon approval, you will receive reimbursement by direct deposit or check, depending on how you set up your account.
How to submit proof of premium payment?
You can submit proof of premium payments through the online portal, EZ Receipts mobile app (available at the App Store® and Google Play™) or by mail or fax. You have until December 31 of the following benefit year to submit your claim for reimbursement.
What is Medicare beneficiary?
The Medicare beneficiary when the beneficiary has obtained a settlement, judgment, award or other payment. The liability insurer (including a self-insured entity), no-fault insurer, or workers’ compensation (WC) entity when that insurer or WC entity has ongoing responsibility for medicals (ORM). For ORM, there may be multiple recoveries ...
What is included in a demand letter for Medicare?
The demand letter also includes information on administrative appeal rights. For demands issued directly to beneficiaries, Medicare will take the beneficiary’s reasonable procurement costs (e.g., attorney fees and expenses) into consideration when determining its demand amount.
How long does interest accrue?
Interest accrues from the date of the demand letter, but is only assessed if the debt is not repaid or otherwise resolved within the time period specified in the recovery demand letter. Interest is due and payable for each full 30-day period the debt remains unresolved; payments are applied to interest first and then to the principal. Interest is assessed on unpaid debts even if a debtor is pursuing an appeal or a beneficiary is requesting a waiver of recovery; the only way to avoid the interest assessment is to repay the demanded amount within the specified time frame. If the waiver of recovery or appeal is granted, the debtor will receive a refund.
Can CMS issue more than one demand letter?
For ORM, there may be multiple recoveries to account for the period of ORM, which means that CMS may issue more than one demand letter. When Medicare is notified of a settlement, judgment, award, or other payment, including ORM, the recovery contractor will perform a search of Medicare paid claims history.
Can Medicare waive recovery of demand?
The beneficiary has the right to request that the Medicare program waive recovery of the demand amount owed in full or in part. The right to request a waiver of recovery is separate from the right to appeal the demand letter, and both a waiver of recovery and an appeal may be requested at the same time. The Medicare program may waive recovery of the amount owed if the following conditions are met:
What is Medicare reimbursement rate?
The reimbursement rates are the monetary amounts that Medicare pays to health care providers, hospitals, laboratories, and medical equipment companies for performing certain services and providing medical supplies for individuals enrolled in Medicare insurance. To receive reimbursement payments at the current rates established by Medicare, health care professionals and service companies need to be participants in the Medicare program. While non-participating professionals and companies are able to submit claims and receive reimbursements for their services, their reimbursements will be slightly lower than the rates paid to participants.
How much does Medicare pay for medical services?
The Medicare reimbursement rates for traditional medical procedures and services are mostly established at 80 percent of the cost for services provided. Some medical providers are reimbursed at different rates. Clinical nurse specialists are paid 85 percent for most of their billed services and clinical social workers are paid 75 percent ...
What is the Medicare coinsurance?
Today, Medicare enrollees who use the services of participating health care professionals will be responsible for the portion of a billing claim not paid by Medicare. The majority of enrollee responsibility will be 20 percent, often referred to as coinsurance. With clinical nurse specialists that responsibility would be 15 percent and 25 percent for clinical social workers.
How many specialists are on the Medicare committee?
Medicare establishes the reimbursement rates based on recommendations from a select committee of 52 specialists. The committee is composed of 29 medical professionals and 23 others nominated by professional societies.
Why use established rates for health care reimbursements?
Using established rates for health care reimbursements enables the Medicare insurance program to plan and project for their annual budget. The intent is to inform health care providers what payments they will receive for their Medicare patients.
What percentage of Medicare bill is not paid?
The majority of enrollee responsibility will be 20 percent , often referred to as coinsurance.
What is Medicare establishment rate schedule?
The establishment rate schedules are complex, multifunctional, and revised annually. The schedules for Medicare reimbursement rates are pre-determined base rates developed using a variety of factors that include the following.
What is published reimbursement policy?
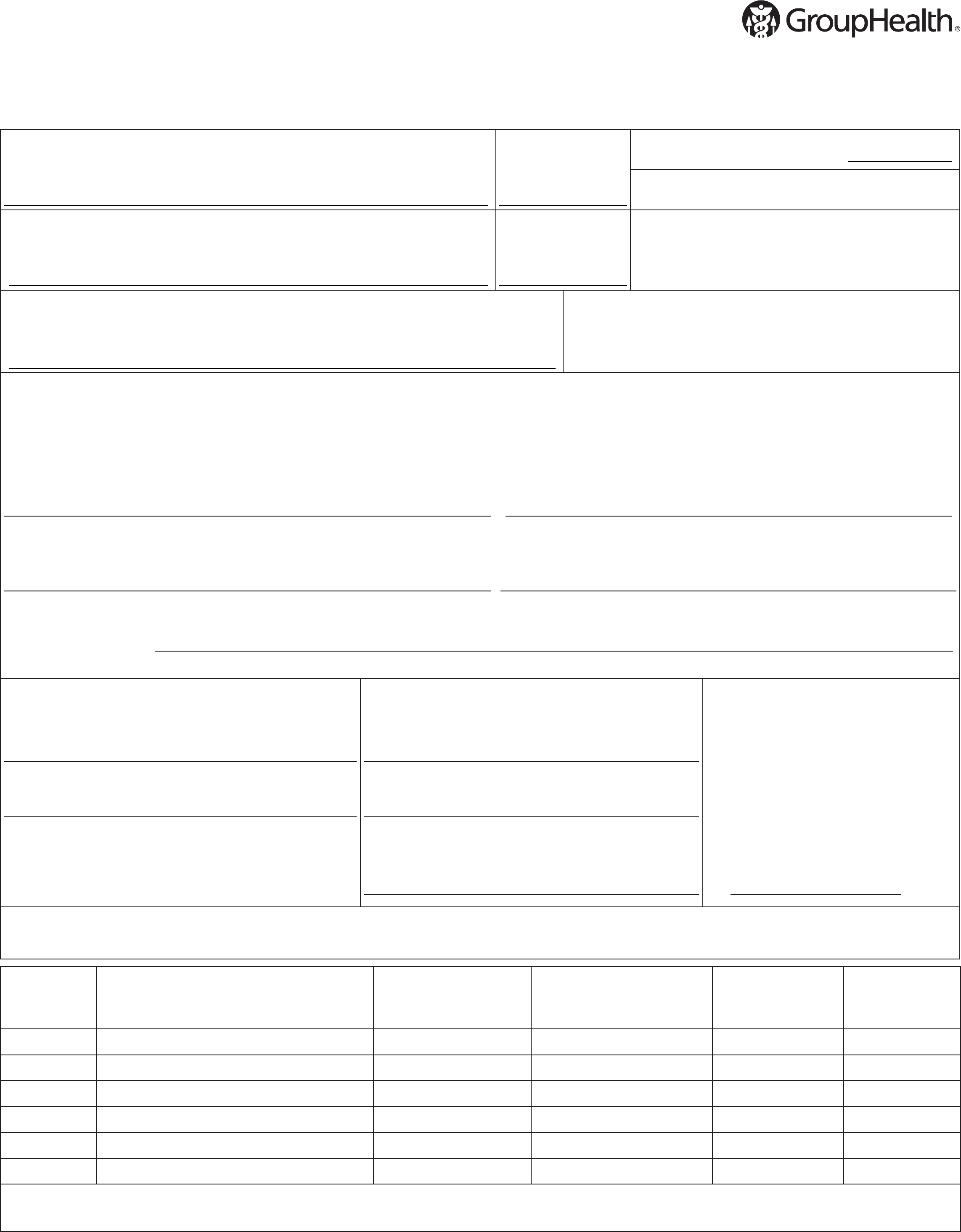
Published reimbursement policies are intended to ensure reimbursement based on the code or codes that correctly describe the health care services provided. Published reimbursement policies are intended to ensure reimbursement based on the code or codes that correctly describe the health care services provided.
What are the factors that affect reimbursement?
These factors may include, but are not limited to: legislative mandates, the physician or other provider contracts, and/or the member specific benefit plan documents**.
Where is the provider service number on a health card?
For questions, please contact your local Network Management representative or call the Provider Services number on the back of the member’s health ID card.
Medicare’s Demand Letter
Assessment of Interest and Failure to Respond
- Interest accrues from the date of the demand letter, but is only assessed if the debt is not repaid or otherwise resolved within the time period specified in the recovery demand letter. Interest is due and payable for each full 30-day period the debt remains unresolved; payments are applied to interest first and then to the principal. Interest is a...
Right to Appeal
- It is important to note that the individual or entity that receives the demand letter seeking repayment directly from that individual or entity is able to request an appeal. This means that if the demand letter is directed to the beneficiary, the beneficiary has the right to appeal. If the demand letter is directed to the liability insurer, no-fault insurer or WC entity, that entity has the ri…
Waiver of Recovery
- The beneficiary has the right to request that the Medicare program waive recovery of the demand amount owed in full or in part. The right to request a waiver of recovery is separate from the right to appeal the demand letter, and both a waiver of recovery and an appeal may be requested at the same time. The Medicare program may waive recovery of the amount owed if the following con…