Medicare Secondary Payer: When Is Medicare Primary or Secondary?
- Medicare can work alongside other health insurance plans to cover more costs and services.
- Medicare is often the primary payer when working with other insurance plans.
- A primary payer is the insurer that pays a healthcare bill first.
- A secondary payer covers remaining costs, such as coinsurances or copayments.
How does Medicare calculate secondary payment?
The Medicare Secondary Payer (MSP) provisions protect the Medicare Trust Fund from making payments when another entity has the responsibility of paying first. Any entity providing items and services to Medicare patients must determine if Medicare is the primary payer.
What is a good secondary insurance to Medicare?
Medicare Secondary Payer (MSP) is a term used when Medicare is not responsible for paying first on a healthcare claim. The decision as to who is responsible for paying first on a claim and who pays second is known in the insurance industry as “coordination of benefits.”
Does Medicare ever pay for secondary?
Jun 30, 2020 · Medicare Secondary Payer (MSP) is the term generally used when the Medicare program does not have primary payment responsibility - that is, when another entity has the responsibility for paying before Medicare.
How to bill Medicare as secondary?
Mar 11, 2020 · A secondary payer assumes coverage of whatever amount remains after the primary payer has satisfied its portion of the benefit, up to any limit established by the policies of the secondary payer coverage terms. When Medicare coordinates benefits with other health insurance coverage providers, there are a variety of factors that play into whether Medicare is …
See more
Jan 06, 2022 · Being a “secondary payer” means that Medicare is second-in-line to paying your healthcare claims. The primary payer—whoever else you’re insured by on top of Medicare—will be the primary source responsible for covering your bills.
How does Medicare Secondary Payer work?
The insurance that pays first (primary payer) pays up to the limits of its coverage. The one that pays second (secondary payer) only pays if there are costs the primary insurer didn't cover. The secondary payer (which may be Medicare) may not pay all the remaining costs.
How do you know if Medicare is primary or secondary?
Medicare is always primary if it's your only form of coverage. When you introduce another form of coverage into the picture, there's predetermined coordination of benefits. The coordination of benefits will determine what form of coverage is primary and what form of coverage is secondary.
Under which circumstance is Medicare the secondary payer?
Medicare may be the secondary payer when: a person has a GHP through their own or a spouse's employment, and the employer has more than 20 employees. a person is disabled and covered by a GHP through an employer with more than 100 employees.Oct 29, 2020
Is Medicare primary or secondary payer?
After the coordination period ends, Medicare pays first and the group health plan pays second . If you originally got Medicare due to your age or a disability other than ESRD, and your group health plan was your primary payer, then it will continue to be the primary payer when you become eligible because of ESRD .
Is Medicare always the primary payer?
If you don't have any other insurance, Medicare will always be your primary insurance. In most cases, when you have multiple forms of insurance, Medicare will still be your primary insurance. Here are several common instances when Medicare will be the primary insurer.
Does Medicare cover copay as secondary?
Medicare will normally act as a primary payer and cover most of your costs once you're enrolled in benefits. Your other health insurance plan will then act as a secondary payer and cover any remaining costs, such as coinsurance or copayments.
How do I submit a secondary claim to Medicare?
Medicare Secondary Payer (MSP) claims can be submitted electronically to Novitas Solutions via your billing service/clearinghouse, directly through a Secure File Transfer Protocol (SFTP) connection, or via Novitasphere portal's batch claim submission.Sep 9, 2021
What are the MSP codes?
Medicare Secondary Payer (MSP) Condition CodesCondition CodeReport When02Employment-related condition03Patient covered by other insurance not reflected here05Lien has been filed06ESRD patient in 1st 30 months7 more rows•Feb 15, 2016
Can you have Medicare and Humana at the same time?
People eligible for Medicare can get coverage through the federal government or through a private health insurance company like Humana. Like Medicaid, every Medicare plan is required by law to give the same basic benefits.
What is Medicare Secondary Payer?
The Medicare Secondary Payer (MSP) provisions protect the Medicare Trust Fund from making payments when another entity has the responsibility of paying first. Any entity providing items and services to Medicare patients must determine if Medicare is the primary payer. This booklet gives an overview of the MSP provisions and explains your responsibilities in detail.
What happens if you don't file a claim with the primary payer?
File proper and timely claims with the primary payer. Not filing proper and timely claims with the primary payer may result in claim denial. Policies vary depending on the payer; check with the payer to learn its specific policies.
Why does Medicare make a conditional payment?
Medicare may make pending case conditional payments to avoid imposing a financial hardship on you and the patient while awaiting a contested case decision.
What is a COB in health insurance?
Coordination of Benefits (COB) allows plans to determine their payment responsibilities. The BCRC collects, manages, and uploads information to the Common Working File (CWF) about patients’ other health insurance coverage. Providers, physicians, and other suppliers must collect accurate MSP patient information to ensure that claims are filed properly.
How long does it take to pay a no fault claim?
For no-fault insurance and WC claims, “paid promptly” means payment within 120 days after the no-fault insurance or WC carrier got the claim for specific items and services. Without contradicting information, you must treat the service date for specific items and services as the claim date when determining the paid promptly period; for inpatient services, you must treat the discharge date as the service date.
Can Medicare make a payment?
Medicare can’t make payment when payment “has been made or can reasonably be expected to be made” under liability insurance (including self-insurance), no-fault insurance, or a WC law or plan of the United States, called a primary plan.
Can Medicare deny a claim?
Medicare may mistakenly pay a claim as primary if it meets all billing requirements, including coverage and medical necessity guidelines . However, if the patient’s CWF MSP record shows another insurer should pay primary to Medicare, we deny the claim.
What is Medicare Secondary Payer?
Medicare Secondary Payer (MSP) is the term generally used when the Medicare program does not have primary payment responsibility - that is, when another entity has the responsibility for paying before Medicare. When Medicare began in 1966, it was the primary payer for all claims except for those covered by Workers' Compensation, ...
When did Medicare start?
When Medicare began in 1966 , it was the primary payer for all claims except for those covered by Workers' Compensation, Federal Black Lung benefits, and Veteran’s Administration (VA) benefits.
How long does ESRD last on Medicare?
Individual has ESRD, is covered by a GHP and is in the first 30 months of eligibility or entitlement to Medicare. GHP pays Primary, Medicare pays secondary during 30-month coordination period for ESRD.
What age does GHP pay?
Individual is age 65 or older, is covered by a GHP through current employment or spouse’s current employment AND the employer has 20 or more employees (or at least one employer is a multi-employer group that employs 20 or more individuals): GHP pays Primary, Medicare pays secondary. Individual is age 65 or older, ...
What are the responsibilities of an employer under MSP?
As an employer, you must: Ensure that your plans identify those individuals to whom the MSP requirement applies; Ensure that your plans provide for proper primary payments whereby law Medicare is the secondary payer; and.
What is conditional payment?
A conditional payment is a payment Medicare makes for services another payer may be responsible for.
Why is Medicare conditional?
Medicare makes this conditional payment so that the beneficiary won’t have to use his own money to pay the bill. The payment is “conditional” because it must be repaid to Medicare when a settlement, judgment, award or other payment is made. Federal law takes precedence over state laws and private contracts.
What is secondary payer?
A secondary payer assumes coverage of whatever amount remains after the primary payer has satisfied its portion of the benefit, up to any limit established by the policies of the secondary payer coverage terms.
Who is responsible for making sure their primary payer reimburses Medicare?
Medicare recipients may be responsible for making sure their primary payer reimburses Medicare for that payment. Medicare recipients are also responsible for responding to any claims communications from Medicare in order to ensure their coordination of benefits proceeds seamlessly.
How does Medicare work with insurance carriers?
Generally, a Medicare recipient’s health care providers and health insurance carriers work together to coordinate benefits and coverage rules with Medicare. However, it’s important to understand when Medicare acts as the secondary payer if there are choices made on your part that can change how this coordination happens.
How old do you have to be to be covered by a group health plan?
Over the age of 65 and covered by an employment-related group health plan as a current employee or the spouse of a current employee in an organization that shares a plan with other employers with more than 20 employees between them.
Is Medicare a secondary payer?
Medicare is the secondary payer if the recipient is: Over the age of 65 and covered by an employment-related group health plan as a current employee or the spouse of a current employee in an organization with more than 20 employees.
Is ESRD covered by COBRA?
Diagnosed with End-Stage Renal Disease (ESRD) and covered by a group health plan or COBRA plan; Medicare becomes the primary payer after a 30-day coordination period. Receiving coverage through a No-Fault or Liability Insurance plan for care related to the accident or circumstances involving that coverage claim.
Does Medicare pay conditional payments?
In any situation where a primary payer does not pay the portion of the claim associated with that coverage, Medicare may make a conditional payment to cover the portion of a claim owed by the primary payer. Medicare recipients may be responsible for making sure their primary payer reimburses Medicare for that payment.
When Is Medicare A Primary Payer?
Knowing the difference between Medicare being a primary or secondary payer matters when you are covered by at least one other insurance plan other than Medicare. So if Medicare is the only insurer you have, they’ll be the primary payer on all of your claims, and then you will have to pay the remainder of the bill.
When Is Medicare A Secondary Payer?
In situations where Medicare is a secondary payer, it will still cover all the same things as a primary payer situation—they’ll just be second-in-line for coverage after the primary payer takes care of as much as they can.
What is the primary payer?
The primary payer is required to process and make primary payment on the claim in accordance with the coverage provisions of its contract. If, after the primary payer processes the claim, it does not pay in full for the services, Medicare secondary benefits may be paid for the services.
What is no fault insurance?
No-fault insuranceis a form of insurance that pays for medical expenses for injuries sustained on the property or premises of the insured, or in the use, occupancy, or operation of an automobile regardless of who may have been responsible for causing the accident.
Can you get workers compensation under Medicare?
Workers' Compensation (WC) Payment under Medicare may not be made for any items and services to the extent that payment has been made or can reasonably be expected to be made for such items or services under a Workers' Compensation(WC) law or plan of the United States or any State.
When will Medicare not pay a contractor?
The contractor will not make any Medicare payment if the beneficiary has not filed a claim or cooperated fully with the provider, physician or other supplier or the GHP. Also, the contractor will not make any Medicare payments until the beneficiary has exhausted the entire claims process. Conditional benefits are not payable if payment cannot be made under the GHP because the beneficiary failed to file a proper claim (See §20 for definition of proper claim) unless the failure to file a proper claim is due to mental or physical incapacity of the beneficiary. A beneficiary need not file any appeal if not inclined to do so.
What is the prohibition on Medicare?
An employer or other entity is prohibited from offering Medicare beneficiaries financial or other benefits as incentives not to enroll in or to terminate enrollment in a GHP or LGHP that is or would be primary to Medicare. This prohibition precludes the offering of benefits to Medicare beneficiaries that are alternatives to the employer's primary plan (e.g., prescription drugs) unless the beneficiary has primary coverage other than Medicare. An example would be primary plan coverage through his/her own or a spouse's employer. This rule applies even if the payments or benefits are offered to all other individuals who are eligible for coverage under the plan. It is a violation of the Medicare law every time a prohibited offer is made regardless of whether it is oral or in writing. Any entity that violates the prohibition is subject to a civil money penalty of up to $5,000 for each violation.
What is leased employee?
Leased employees (as defined in §414(n)(2) of the IRC) are treated as employees of the recipient. The term "leased employee" means any person who is not an employee of the recipient of the services but who provides services to the recipient if the:
What is a senior federal judge?
Senior Federal judges are retired judges of the U.S. court system and the Tax Court. They may continue to adjudicate cases, but they are entitled to full salary as a retirement benefit whether or not they perform judicial services for the Government. By law, the remuneration they receive as senior judges is not considered wages for Social Security retirement offset purposes. Since they are considered retired for Social Security purposes, they are not considered to have current employment status for purposes of the working aged and disability provisions.
How long does a CMS hearing take?
Employer and employee organizations have 65 days from the date of their notice to request a hearing.
What is the right to collect double damages?
Section 1862(b)(3)(A) of the Act provides that any claimant (including a beneficiary, provider, physician, or supplier) has the right to take legal action against, and to collect double damages from a GHP, that fails to pay primary benefits for services covered by the GHP. Any claimant, also, has the right to take legal action against, and to collect double damages from, a no-fault or liability insurer that fails to pay primary benefits for services covered by the no-fault or liability insurer where required to do so under §1862(b) of the Act.
What age do you have to be to get Medicare?
Section 1862(b)(1)(A)(i)(II) of the Act provides that GHPs of employers of 20 or more employees must provide to any employee or spouse age 65 or older the same benefits under the same conditions that they provide to employees and spouses under 65 if those 65 or older are covered under the plan on the basis of the individual's current employment status or the current employment status of a spouse of any age. The requirement applies regardless of whether the individual or spouse 65 or older is entitled to Medicare.
What is Medicare Secondary Payer questionnaire?
Medicare Secondary Payer Questionnaire. (Short Form) The information contained in this form is used by Medicare to determine if there is other insurance that should pay claims primary to Medicare.
What is the purpose of Medicare Secondary Payer questionnaire?
CMS developed an MSP questionnaire for providers to use as a guide to help identify other payers that may be primary to Medicare. This questionnaire is a model of the type of questions you should ask to help identify MSP situations.
What is the purpose of the Medicare questionnaire?
What is it? The Medicare Current Beneficiary Survey (MCBS) is a survey of people with Medicare. We use it to learn more about things like how people get their health care, the rising cost of health care, and how satisfied people are with their care.
What does Medicare Secondary Payer mean?
Medicare Secondary Payer (MSP) is the term generally used when the Medicare program does not have primary payment responsibility – that is, when another entity has the responsibility for paying before Medicare. … Medicare is also the primary payer in certain instances, provided several conditions are met.
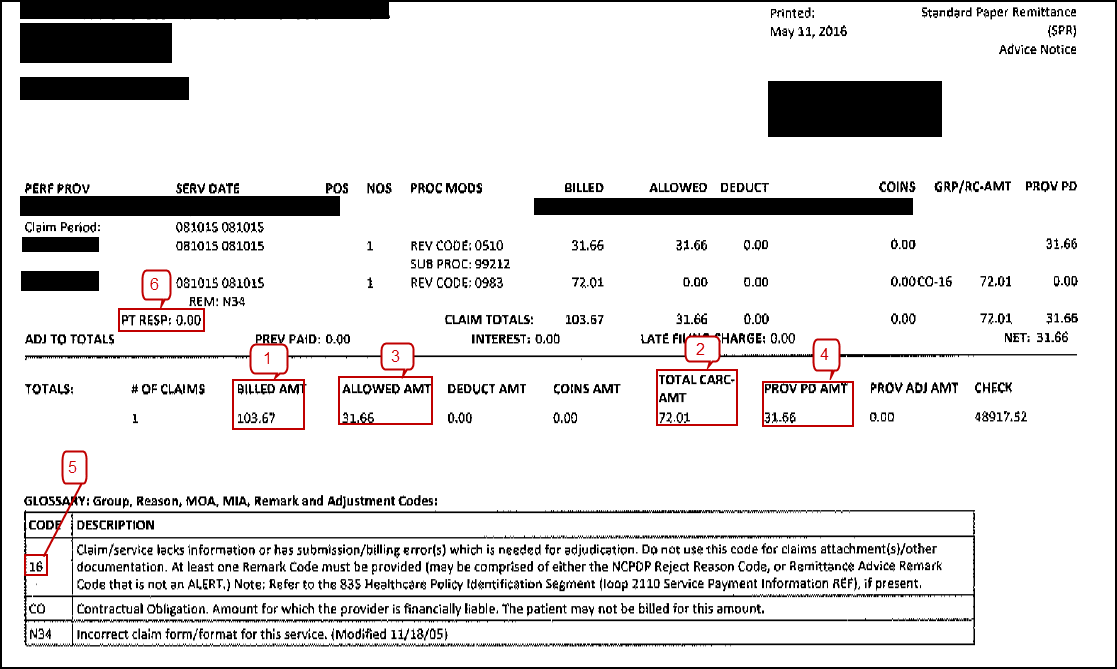
How does Medicare process secondary claims?
When Medicare is the secondary payer, submit the claim first to the primary insurer. … If, after processing the claim, the primary insurer does not pay in full for the services, submit a claim via paper or electronically, to Medicare for consideration of secondary benefits.
Does Medicare automatically send claims to secondary insurance?
Medicare will send the secondary claims automatically if the secondary insurance information is on the claim. … Medicare crosses over most claims automatically and you can see this on the remittance.
Does Medicare pay copays as secondary insurance?
Medicare will normally act as a primary payer and cover most of your costs once you’re enrolled in benefits. Your other health insurance plan will then act as a secondary payer and cover any remaining costs, such as coinsurance or copayments.
Medicare Second Payer
Medicare Secondary Payer (MSP) is the term used by Medicare when Medicare is not responsible for paying first. (The private insurance industry generally talks about “ Coordination of Benefits ” when assigning responsibility for first and second payment.)
Precedence of Federal Law
Federal law takes precedence over State law and private contracts. Thus, for the categories of people described below, Medicare is the secondary payer regardless of state law or plan provisions. These Federal requirements are found in Section 1862 (b) of the Social Security Act {42 USC Section 1395y (b) (5)}.
Group Health Plans (GHP)
An employer cannot offer, subsidize, or be involved in the arrangement of a Medicare supplement policy where the law makes Medicare the secondary payer. Even if the employer does not contribute to the premium, but merely collects it and forwards it to the appropriate individual’s insurance company, the GHP policy is the primary payer to Medicare.
Responsibilities of Attorneys Under MSP
Immediately, upon taking a case, that involves a Medicare beneficiary, inform the COB Contractor about a potential liability lawsuit, and
Responsibilities of Insurers Under MSP
Report to the COB Contractor if you find that CMS has paid primary when you are primary to Medicare (i.e. 411.25).