
A Medicare Special Enrollment Period is an opportunity for people in special circumstances to enroll in Medicare. Learn more and use this guide to help you sign up for Medicare. A Special Enrollment Period (SEP) is an enrollment period that takes place outside of the annual Medicare enrollment periods, such as the annual Open Enrollment Period.
Who is eligible for Medicare special enrollment period?
Medicare SNPs are a type of Medicare Advantage Plan (like an HMO or PPO). Medicare SNPs limit membership to people with specific diseases or characteristics. Medicare SNPs tailor their benefits, provider choices, and drug formularies to best meet the specific needs of the groups they serve. Find out who can join a Medicare SNP.
What is a special needs plan Medicare Advantage?
Nov 24, 2021 · A Special Enrollment Period (SEP) is an enrollment period that takes place outside of the annual Medicare enrollment periods, such as the annual Open Enrollment Period. They are granted to people who were prevented from enrolling in Medicare during the regular enrollment period for a number of specific reasons.
What is a special enrollment period (Sep)?
Nov 05, 2021 · When it comes time for open enrollment each fall, you may hear about the Medicare Advantage Special Needs Plans (SNPs). These are a type of Medicare Advantage plan for people with additional heath needs, often due to a serious or chronic condition such as diabetes or dementia.
How do I qualify for a Medicare special needs plan?
Apr 12, 2022 · What is the Medicare Special Enrollment Period? Published by: Medicare Made Clear There are actually two kinds of Medicare Special Enrollment Periods. A Medicare Special Enrollment Period allows you to switch plans or sign up for Medicare outside of the standard Medicare enrollment periods.

What are the three types of Medicare special needs plans?
- Chronic Condition SNP (C-SNP)
- Dual Eligible SNP (D-SNP)
- Institutional SNP (I-SNP)
Who is eligible for C SNP?
What is the difference between D SNP and MMP?
What does CSNP mean?
Does diabetes qualify for C SNP?
Is SNP a Medicare Advantage Plan?
Is Mmai better than Medicare?
Is MMP the same as Dsnp?
What is oh MMP?
What does CMS consider a chronic condition?
...
Chronic Conditions.
| Alcohol Abuse | Drug Abuse/ Substance Abuse |
|---|---|
| Cancer (Breast, Colorectal, Lung, and Prostate) | Ischemic Heart Disease |
| Chronic Kidney Disease | Osteoporosis |
What does ISNP stand for in Medicare?
Is hyperlipidemia considered a chronic condition?
What is a special enrollment period?
Special circumstances (Special Enrollment Periods) You can make changes to your Medicare Advantage and Medicare prescription drug coverage when certain events happen in your life, like if you move or you lose other insurance coverage. These chances to make changes are called Special Enrollment Periods (SEPs).
What can I do with my Medicare Advantage Plan?
What can I do? Join a Medicare Advantage Plan with drug coverage or a Medicare Prescription Drug Plan. Switch from your current plan to another Medicare Advantage Plan with drug coverage or a Medicare Prescription Drug Plan. Drop your Medicare Advantage Plan with drug coverage and return to Original Medicare .
When does Medicare change coverage?
You can’t use this Special Enrollment Period from October–December. However, all people with Medicare can make changes to their coverage from October 15–December 7, and the changes will take effect on January 1.
What is the difference between Medicare and Original Medicare?
Original Medicare. Original Medicare is a fee-for-service health plan that has two parts: Part A (Hospital Insurance) and Part B (Medical Insurance). After you pay a deductible, Medicare pays its share of the Medicare-approved amount, and you pay your share (coinsurance and deductibles).
What is a special enrollment period?
A Special Enrollment Period (SEP) is an enrollment period that takes place outside of the annual Medicare enrollment periods, such as the annual Open Enrollment Period. They are granted to people who were prevented from enrolling in Medicare during the regular enrollment period for a number of specific reasons.
When is open enrollment for Medicare Part D?
Open Enrollment: The fall Medicare Open Enrollment Period has officially begun and lasts from October 15 to December 7, 2020. You may be able to enroll in or switch to another Medicare Advantage plan or Medicare Part D prescription drug plan, or you can drop your plan and return to Original Medicare. View a complete list of Medicare Enrollment ...
When is the open enrollment period for Medicare?
Learn more and use this guide to help you sign up for Medicare. Open Enrollment: The fall Medicare Open Enrollment Period has officially begun and lasts from October 15 to December 7, 2020. You may be able to enroll in ...
What happens if you don't enroll in Medicare at 65?
If you did not enroll in Medicare when you turned 65 because you were still employed and were covered by your employer’s health insurance plan, you will be granted a Special Enrollment Period.
How often can you change your Medicare Advantage plan?
If you move into, out of, or currently reside in a facility of special care such as a skilled nursing home or long-term care hospital, you may enroll in, disenroll from, or change a Medicare Advantage plan one time per month.
How long do you have to disenroll from Medicare Advantage?
If you enrolled in a Medicare Advantage plan when you first became eligible for Medicare, you have 12 months to disenroll from the plan and transition back to Original Medicare.
How long does it take to switch to another Medicare Advantage plan?
If you permanently move out of your Medicare Advantage plan’s coverage area or move to an area with more available plans, you may switch to another Medicare Advantage plan beginning the month before your move and lasting for two months.
What is a Medicare Special Needs Plan?
A Medicare Special Needs plan is a type of Medicare Advantage Plan available only to people who have certain qualifying health conditions or situations.
Who can join an SNP?
Anyone who is eligible for Medicare Part A (hospital insurance) and Medicare Part B (medical insurance), lives in the plan’s service area, and meets the plan’s eligibility requirements can join an SNP.
What are the different types of SNP plans and eligibility requirements?
There are several kinds of SNPs, and to be eligible to sign up, enrollees must meet the qualifications for at least one of these:
How does a Medicare SNP work?
Medicare SNPs must provide you with the same benefits as Original Medicare, but they usually offer more help and covered benefits than Original Medicare or other Medicare Advantage plans. This additional care includes:
How much do SNP plans cost?
That depends. SNPs generally don’t cost more than other Medicare Advantage plans. But because some SNPs offer additional care, they may charge a monthly premium in addition to the base premium.
Can I get my healthcare from any doctor or network?
Usually, you need to stay in the Medicare SNP network, which is generally geared toward your specific needs or condition. There are two exceptions, however:
What questions should I ask before I enroll in an SNP?
Just as you would before joining any plan, your questions should be geared toward your individual needs. Here are some examples of things to ask to help you narrow down your choices.
What is a special needs plan?
A special needs plan (SNP) is a Medicare Advantage (MA) coordinated care plan (CCP) specifically designed to provide targeted care and limit enrollment to special needs individuals. A special needs individual could be any one of the following: An institutionalized individual, A dual eligible, or. An individual with a severe or disabling chronic ...
Do SNPs have to follow Medicare?
SNPs are expected to follow existing MA program rules, including MA regulations at 42 CFR 422, as modified by guidance, with regard to Medicare- covered services and Prescription Drug Benefit program rules. All SNPs must provide Part D prescription drug coverage because special needs individuals must have access to prescription drugs to manage and control their special health care needs. SNPs should assume that, if no modification is contained in guidance, existing Part C and D rules apply.
What is a dual eligible plan?
A dual eligible, or. An individual with a severe or disabling chronic condition, as specified by CMS. A SNP may be any type of MA CCP, including either a local or regional preferred provider organization (i.e., LPPO or RPPO) plan, a health maintenance organization (HMO) plan, or an HMO Point-of-Service (HMO-POS) plan.
Did CMS accept SNP applications in 2008?
Accordingly, CMS did not accept SNP applications in 2008 for contract year (CY) 2009. The Medicare Improvements for Patients and Providers Act of 2008 (MIPPA) lifted the Medicare, Medicaid, and SCHIP Extension Act of 2007 moratorium on approving new SNPs.
Why do SNPs need to provide Part D coverage?
All SNPs must provide Part D prescription drug coverage because special needs individuals must have access to prescription drugs to manage and control their special health care needs. SNPs should assume that, if no modification is contained in guidance, existing Part C and D rules apply.
When did the SNP program end?
Most recently, section 206 of the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) extended the SNP program through December 31, 2018.
What is a special enrollment period for Medicare?
A Medicare Special Enrollment Period allows you to switch plans or sign up for Medicare outside of the standard Medicare enrollment periods. If you have Medicare: For people who already have Medicare and who experience a qualifying life event, there is a two-month Special Enrollment Period for switching a Medicare Advantage or Part D plan.
How long is the Medicare Advantage enrollment period?
If you have Medicare: For people who already have Medicare and who experience a qualifying life event, there is a two-month Special Enrollment Period for switching a Medicare Advantage or Part D plan.
How long is the Medicare enrollment period for people working past 65?
When Working Past 65: 8-Month Special Enrollment Period. For people who work past 65 and qualify to delay Medicare with creditable employer coverage, there is an 8-month Special Enrollment Period that allows you to enroll in Part A (if you haven’t yet), Part B , Part C and Part D without late penalties. This Special Enrollment Period is tricky ...
What happens if you enroll in Medicare after 2 months?
If you enroll after the two-month mark, you’ll face late enrollment penalties for Part D (regardless of whether you end up with a stand-alone Part D plan or a Medicare Advantage plan that includes drug coverage).
What is Medicare Made Clear?
Medicare Made Clear is brought to you by UnitedHealthcare to help make understanding Medicare easier. Click here to take advantage of more helpful tools and resources from Medicare Made Clear including downloadable worksheets and guides.
How long does it take to enroll in a 5 star plan?
You want to enroll in a 5-star plan at any time or drop your first Medicare Advantage plan within 12 months of enrolling. You move into or out of a qualified institutional facility, like a nursing home. You are enrolled in or lose eligibility for a qualified State Pharmaceutical Assistance Program.
Does Medicare Special Needs include prescription drug coverage?
Like all Medicare Advantage plans, Special Needs Plans will provide all of the same coverage as Medicare Part A and Part B. Additionally, Special Needs Plans may feature a custom set of benefits designed specifically for the needs of the beneficiary. All Medicare Special Needs Plans include prescription drug coverage.
How to qualify for a special needs plan?
In order to qualify for a Special Needs Plan, you must meet each of the following criteria: Be enrolled in Medicare Part A and Part B. Have one of the chronic conditions above, reside in a nursing home or require home nursing care or be Medicare dual-eligible. Reside in the plan’s service area. A Chronic Condition SNP will require a note ...
What is Medicare Advantage?
Medicare Advantage plans are a form of private Medicare coverage. These plans, sold by private insurance companies, offer all the same benefits as Original Medicare (Part A and Part B). Many Medicare Advantage plans also offer some additional coverage, which may include coverage for dental, vision, hearing, prescription drugs and more.
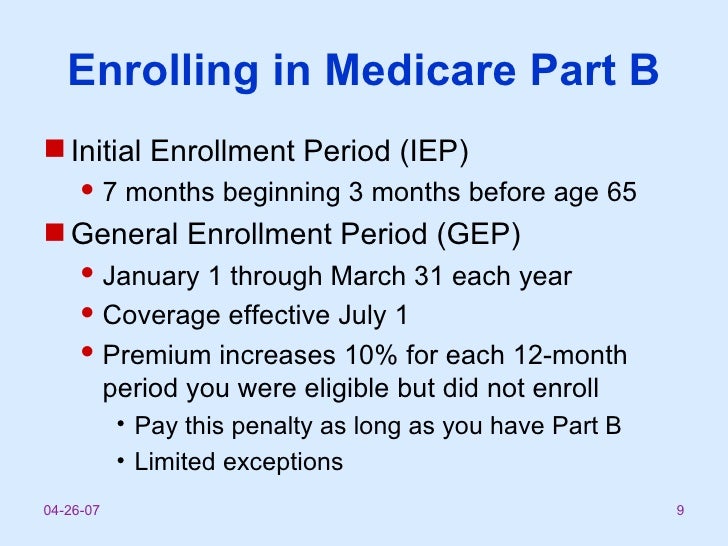
How long does Medicare IEP last?
You may join a Medicare Special Needs Plan during the same enrollment periods used for standard Medicare Advantage plans. Your Medicare IEP is a seven-month period that begins three months before you turn 65 years old, includes the month of your birthday and extends for three more months thereafter.
When does Medicare enroll in AEP?
Annual Enrollment Period (AEP) The Medicare AEP takes place every year from October 15 to December 7.
When does Medicare IEP start?
Annual Enrollment Period (AEP) The Medicare AEP takes place every year from October 15 to December 7. Special Enrollment Period (SEP)
When does Medicare AEP take place?
The Medicare AEP takes place every year from October 15 to December 7. Special Enrollment Period (SEP) You may be granted a Special Enrollment Period at any time throughout the year, depending on your circumstances.
What Events Trigger a Special Enrollment Period for Medicare?
Lorraine Roberte is an insurance writer for The Balance. As a personal finance writer, her expertise includes money management and insurance-related topics. She has written hundreds of reviews of insurance products.
The Purpose of Medicare Special Enrollment
Normally, you can only enroll in Medicare or make changes to your plan during specific enrollment windows, including the initial enrollment period, open enrollment, and general enrollment. However, sometimes life’s events require that you make changes outside of these periods. That’s where Medicare's special enrollment comes in.
What if You Miss Special Enrollment?
If you miss special enrollment, you’ll have to wait for another enrollment period to make changes to or enroll in a plan.
How many times can you change Medicare plans during a special enrollment period?
During a special enrollment period, you can make the changes allowed by that type of SEP. Once you make the changes, you’ll need to wait until the next applicable enrollment period to change plans again.
What does an I-SNP need to document?
If an I-SNP enrollee changes residence, the I-SNP must document that it is prepared to implement a CMS-approved MOC at the enrollee’s new residence, or in another I-SNP contracted LTC setting that provides an institutional level of care.
What methodology do I-SNPs use?
In states and territories without a specific tool, I-SNPs must use the same LOC determination methodology used in the respective state or territory in which the I-SNP is authorized to enroll eligible individuals.
What Is A Special Needs Plan?
- A special needs plan (SNP) is a Medicare Advantage (MA) coordinated care plan (CCP) specifically designed to provide targeted care and limit enrollment to special needs individuals. A special needs individual could be any one of the following: 1. An institutionalized individual, 2. A dual eligible, or 3. An individual with a severe or disabling chr...
Statutory and Regulatory History
- The Medicare Modernization Act of 2003 (MMA) established an MA CCP specifically designed to provide targeted care to individuals with special needs. In the MMA, Congress identified “special needs individuals” as: 1) institutionalized individuals; 2) dual eligibles; and/or 3) individuals with severe or disabling chronic conditions, as specified by CMS. MA CCPs established to provide se…
Requirements and Payment Procedures
- SNPs are expected to follow existing MA program rules, including MA regulations at 42 CFR 422, as modified by guidance, with regard to Medicare-covered services and Prescription Drug Benefit program rules. All SNPs must provide Part D prescription drug coverage because special needs individuals must have access to prescription drugs to manage and control their special health c…
Site Overview
- Specific information about each of the three SNP types (C-SNPs, D-SNPs, and I-SNPs), as well as information on the SNP Application and the SNP Model of Care, can be found by clicking the appropriate links on the left-hand side of this page. In addition, there is a link below to the online Medicare Managed Care Manual, which contains Chapter 16b – CMS's current sub-regulatory gu…