The 2022 Part B deductible is $233 per year. After you meet your deductible, you typically pay 20 percent of the Medicare-approved amount for qualified Medicare Part B services and devices. Medicare typically pays the other 80 percent of the cost, no matter what your income level may be.
Full Answer
How are Medicare supplement insurance rates stated?
Medicare health plan appeals - Level 2: Independent Review Entity (IRE) If your plan decides against your reconsideration, they must send you a notice that gives you the specific reason (s) for any full or partial denial. You may send an Independent Review Entity (IRE) information about your case. They must get this information within 10 days ...
How to compare Medicare supplement plans for 2020?
Feb 15, 2022 · The 2022 Part B deductible is $233 per year. After you meet your deductible, you typically pay 20 percent of the Medicare-approved amount for qualified Medicare Part B services and devices. Medicare typically pays the other 80 percent of …
What is the best pricing model for Medicare supplement plans?
Generally, you will have the most options available and the lowest costs if you join a Medicare Supplement plan when you are first eligible. 2. Gender. Some insurance companies offer lower rates on Medicare Supplement plans for women. According to research, women typically live longer, which means they pay more for their coverage over their ...
How much does Medicare Part a cost in 2022?
Nov 16, 2021 · Most people will pay the standard premium amount. In 2022, the standard premium is $170.10. However, if you make more than the preset income limits, you’ll pay more for your premium. The added ...
What is the supplemental Medicare rate?
Is AARP Medicare Supplement community rated?
Which Medicare supplement plan has the highest level of coverage?
Why is my Medicare supplement so expensive?
Do Medigap premiums increase with age?
Why do doctors not like Medicare Advantage plans?
What is the difference between Plan G and high deductible plan G?
Are Medicare supplement plans being phased out?
Is Medicare supplement the same as Medigap?
Does Medigap have an out-of-pocket maximum?
What is Medicare Plan G deductible for 2021?
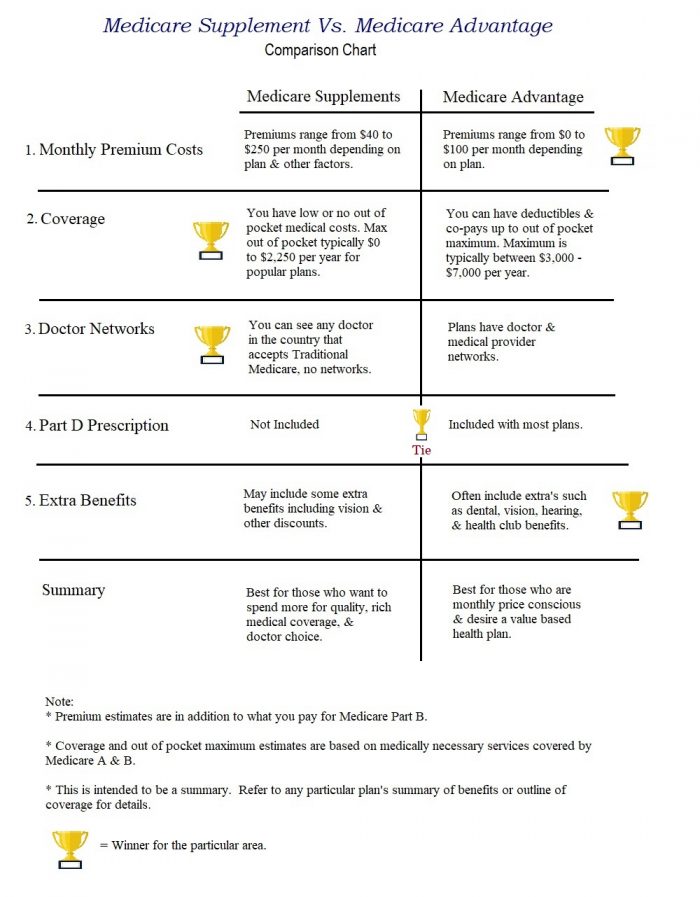
What is the difference between a Medicare Supplement and a Medicare Advantage plan?
How to compare Medicare Supplement Plans 2021?
How to Compare Medicare Supplement Plans. You can use the 2021 Medigap plan chart below to compare the benefits that are offered by each type of plan. Use the scroll bar at the bottom of the chart to view all plans and information. Click here to view enlarged chart. Scroll to the right to continue reading the chart. Scroll for more.
What is the second most popular Medicare plan?
Medigap Plan G is the second most popular Medigap plan, and it is quickly growing in popularity. Plan G enrollment spiked 39 percent in recent years. 2. Medigap Plan G covers all of the same out-of-pocket Medicare costs than Plan F covers, except for the Medicare Part B deductible.
What is the most popular Medicare Supplement?
Medigap Plan F is the most popular Medicare Supplement Insurance plan . 53 percent of all Medigap beneficiaries are enrolled in Plan F. 2. Plan F covers more standardized out-of-pocket Medicare costs than any other Medigap plan. In fact, Plan F covers all 9 of the standardized Medigap benefits a plan may offer.
How much does Medicare Part A cover?
Medicare Part A helps cover your hospital costs if you are admitted to a hospital for inpatient treatment (after you reach your Medicare Part A deductible, which is $1,484 per benefit period in 2021). For the first 60 days of your hospital stay, you aren't required to pay any Part A coinsurance.
How much is the Medicare Part B deductible for 2021?
In 2021, the Part B deductible is $203 per year. Medicare Part B coinsurance or copayment. After you meet your Part B deductible, you are typically required to pay a coinsurance or copay of 20 percent of the Medicare-approved amount for your covered services.
What is the maximum out of pocket for Medicare 2021?
The Plan K out-of-pocket maximum is $6,220 in 2021. The 2021 Plan L out-of-pocket spending limit is $3,110.
How much coinsurance is required for skilled nursing?
There is no coinsurance requirement for the first 20 days of inpatient skilled nursing facility care. However, a $185.50 per day coinsurance requirement begins on day 21 of your stay, and you are then responsible for all costs after day 101 of inpatient skilled nursing facility care (in 2021).
How long does it take to get an IRE?
You may send an Independent Review Entity (IRE) information about your case. They must get this information within 10 days after the date you get the notice telling you your case file has been sent to the IRE.
How long does it take to get a reconsideration?
How long it takes for the IRE to send you its decision in a written Reconsideration Determination depends on the type of request: 1 Expedited (fast) request—72 hours 2 Standard service request—30 days 3 Payment request—60 days
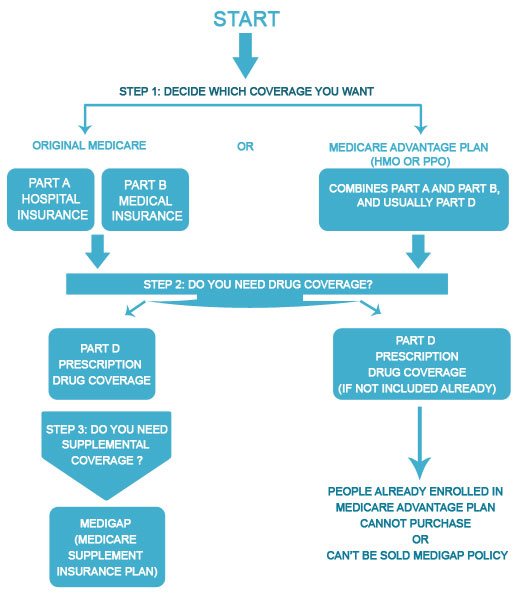
What is Medicare Advantage Plan?
A Medicare Advantage Plan (Part C) (like an HMO or PPO) or another Medicare health plan that offers Medicare prescription drug coverage. Creditable prescription drug coverage. In general, you'll have to pay this penalty for as long as you have a Medicare drug plan.
Do you have to pay late enrollment penalty for Medicare?
In general, you'll have to pay this penalty for as long as you have a Medicare drug plan. The cost of the late enrollment penalty depends on how long you went without Part D or creditable prescription drug coverage. Learn more about the Part D late enrollment penalty.
What happens if you don't buy Medicare?
If you don't buy it when you're first eligible, your monthly premium may go up 10%. (You'll have to pay the higher premium for twice the number of years you could have had Part A, but didn't sign up.) Part A costs if you have Original Medicare. Note.
Does Medicare cover room and board?
Medicare doesn't cover room and board when you get hospice care in your home or another facility where you live (like a nursing home). $1,484 Deductible for each Benefit period . Days 1–60: $0 Coinsurance for each benefit period. Days 61–90: $371 coinsurance per day of each benefit period.
Does Medicare Advantage have a monthly premium?
Some of these additional benefits – such as prescription drug coverage or dental benefits – can help you save some costs on your health care, no matter what your income level may be. Some Medicare Advantage plans even feature $0 monthly premiums, though $0 premium plans may not be available in all locations.
What percentage of Medicare Part B is paid?
After you meet your deductible, you typically pay 20 percent of the Medicare-approved amount for qualified Medicare Part B services and devices. Medicare typically pays the other 80 percent of the cost, no matter what your income level may be.
What is Medicare Part B based on?
Medicare Part B (medical insurance) premiums are based on your reported income from two years prior. The higher premiums based on income level are known as the Medicare Income-Related Monthly Adjustment Amount (IRMAA).
Does income affect Medicare Part A?
Medicare Part A costs are not affected by your income level. Your income level has no bearing on the amount you will pay for Medicare Part A (hospital insurance). Part A premiums (if you are required to pay them) are based on how long you worked and paid Medicare taxes.
Who is Christian Worstell?
Christian Worstell is a licensed insurance agent and a Senior Staff Writer for MedicareAdvantage.com. He is passionate about helping people navigate the complexities of Medicare and understand their coverage options. .. Read full bio
When is the best time to buy Medicare Supplement?
The best time to purchase a Medicare Supplement is during your Medicare Supplement Open Enrollment Period, which starts the first six months that you are enrolled in Medicare Part B and are 65 or older. During this period, you have the right to join any Medicare Supplement plan, regardless of pre-existing conditions or disabilities.
What is community rated Medicare?
There are three methods that a company can use to set rates for their Medicare Supplement policies: • Community-rated: With this pricing policy, every member, regardless of age, pays the same price. Hence, the name “Community.”. • Issue-age-rated: Your age is used for pricing, and is locked in on your policy start date.
Do women get lower Medicare?
Some insurance companies offer lower rates on Medicare Supplement plans for women. According to research, women typically live longer, which means they pay more for their coverage over their lifetime. Women also tend to enjoy better health and thus claim less.
What is household discount?
Household discounts are given by insurance companies to encourage couples to both select the same company as their provider. Some companies even offer discounts if you have anyone over the age of 18 living in the house with you. Discount amounts vary depending on the provider, and not all providers offer them. 7.
What is the Medicare Part D premium for 2021?
Part D plans have their own separate premiums. The national base beneficiary premium amount for Medicare Part D in 2021 is $33.06, but costs vary. Your Part D Premium will depend on the plan you choose.
How much is Medicare Part B 2021?
For Part B coverage, you’ll pay a premium each year. Most people will pay the standard premium amount. In 2021, the standard premium is $148.50. However, if you make more than the preset income limits, you’ll pay more for your premium.
What is Medicare Part B?
Medicare Part B. This is medical insurance and covers visits to doctors and specialists, as well as ambulance rides, vaccines, medical supplies, and other necessities.
Do you pay for Medicare Part A?
Medicare Part A premiums. Most people will pay nothing for Medicare Part A. Your Part A coverage is free as long as you’re eligible for Social Security or Railroad Retirement Board benefits. You can also get premium-free Part A coverage even if you’re not ready to receive Social Security retirement benefits yet.
How many types of Medicare savings programs are there?
Medicare savings programs. There are four types of Medicare savings programs, which are discussed in more detail in the following sections. As of November 9, 2020, Medicare has not announced the new income and resource thresholds to qualify for the following Medicare savings programs.
How much do you need to make to qualify for SLMB?
If you make less than $1,296 a month and have less than $7,860 in resources, you can qualify for SLMB. Married couples need to make less than $1,744 and have less than $11,800 in resources to qualify. This program covers your Part B premiums.
What is the income limit for QDWI?
You must meet the following income requirements to enroll in your state’s QDWI program: an individual monthly income of $4,339 or less. an individual resources limit of $4,000.
How much is Medicare Part A deductible?
Plan A. Hospital Services for Medicare Part A: With Plan A, you are responsible for the Part A deductible of $1,484 for the first 60 days of hospitalization. This plan includes semiprivate room and board and general nursing costs. For days 61 to 90, the plan pays the $371 per day that Medicare does not cover.
Does AARP provide Medicare Supplement?
AARP Medicare Supplement Plans are provided through UnitedHealthcare Insurance Company. For seniors who are concerned that their Medicare plan may not provide all the health insurance coverage they need, these plans are available to supplement their Medicare coverage.
What are the benefits of AARP?
Benefits of AARP Medicare Plans 1 Coverage provided for anywhere in the U.S. 2 You can use any doctor who accepts Medicare, including your current doctor 3 No referrals are necessary 4 Your policy can’t be canceled, or your premium increased, because of health problems 5 A supplement plan can be combined with Medicare Part D to help lower your prescription drug costs 1
What is Plan K for Medicare?
Plan K. Plan K is similar to Plan C, but it pays only 50% rather than 100% of certain costs. Hospital Services for Medicare Part A: Plan K pays only 50%—or $742—of the $1,484 Part A deductible. Regarding care at a skilled nursing facility, it pays up to $92.75, instead of $185.50, per day for days 21 to 100.
How much does Plan B pay?
For days 91 and beyond, Plan B pays $742 per day while using the 60 lifetime reserve days. After the lifetime reserve days are used, Plan B continues to pay 100% of Medicare-eligible expenses for an additional 365 days. After that period, you are responsible for all costs. If you have been in the hospital for at least three days ...
Does Plan G cover Part B?
Plan G. Plan G does not cover one item Plan C covers, but it does cover one item Plan C doesn't cover: Plan G does not cover the Part B deductible of $203. However, like Plan F, it covers 100% of Part B excess medical expense charges above the Medicare-approved amounts. 6 .
Is UnitedHealthcare part of AARP?
Here is a brief overview of the AARP Medical Supplement Plans offered by UnitedHealthcare, which is part of UnitedHealth Group Inc. Note that specific coverage, co-insurance, co-payments, and deductibles may vary by state.
How much does Medicare cost for retirees?
That drives monthly healthcare costs higher, but for most people, standard Medicare costs just $148.50 per month. For your Part B premiums, the federal government—thanks in part to your decades of deductions—pays 75% of the cost.
How much of your paycheck never reached your pocket?
During your working years, you paid into Medicare, albeit reluctantly. You watched as somewhere around 15% of your paycheck never reached your pocket, because the federal government took it for Social Security and Medicare payments. 1