First, Medicare, abuse and waste occurs when false claims are made on behalf of a Medicare beneficiary. For example, you visit a particular physician or medical clinic, they ask for your original Medicare card and give you a certain amount that is due, but then bill original Medicare for more than that amount.
What is a medicare waste?
An error, intentionally or unintentionally, is Medicare waste. Medicare creates the Program Integrity Enhancements to the Provider Enrollment Process rule to end fraud, waste, and abuse.
What is the difference between Medicare fraud waste and abuse?
Differences between Medicare Fraud, Abuse, and Waste. Fraud requires intent to obtain payment and knowing the action is wrong; Abuse creates an unnecessary cost to the Medicare Program, without knowledge; Waste may involve intent or knowledge but could also be unintentional; CMS Efforts to Stop Fraud, Waste, and Abuse
What is considered Medicare abuse?
Medicare abuse includes practices that result in unnecessary costs to the Medicare program. Any activity that does not meet professionally recognized standards or provide patients with medically necessary services is considered abuse. Committing abuse is illegal and should be reported.
What is in the Medicare fraud and abuse booklet?
This booklet provides the following tools to help protect the Medicare Program, your patients, and yourself: ● Medicare fraud and abuse examples ● Overview of fraud and abuse laws ● Government agencies and partnerships dedicated to preventing, detecting, and fighting fraud and abuse ● Resources for reporting suspected fraud and abuse

What is considered Medicare abuse?
What Is Medicare Abuse? Abuse describes practices that may directly or indirectly result in unnecessary costs to the Medicare Program. Abuse includes any practice that does not provide patients with medically necessary services or meet professionally recognized standards of care.
What is the difference between waste and abuse?
What is it exactly? Well, fraud is when someone intentionally lies to a health insurance company, Medicaid or Medicare to get money. Waste is when someone overuses health services carelessly. And abuse happens when best medical practices aren't followed, leading to expenses and treatments that aren't needed.
What is the meaning of waste in the context of Medicare?
▪ Waste means over-utilization of services, or practices that result in. unnecessary costs.
What is the most common type of Medicare abuse?
The most common type of Medicare abuse is the filing of inaccurate or falsified Medicare claims to increase profits.
What is an example of waste in healthcare?
Hospitals create waste when they incur excess inventory costs, storage and movement costs, spoilage and waste. One example is letting supplies expire and then disposing of them, including out-of-date medications.
What is abuse in healthcare billing?
Abuse is defined as practices that are inconsistent with accepted sound fiscal, business, or medical practices, and result in an unnecessary cost or in reimbursement for services that are not medically necessary or that fail to meet professionally recognized standards for health care.
What are some examples of waste in the healthcare system that lead to the need for value based care?
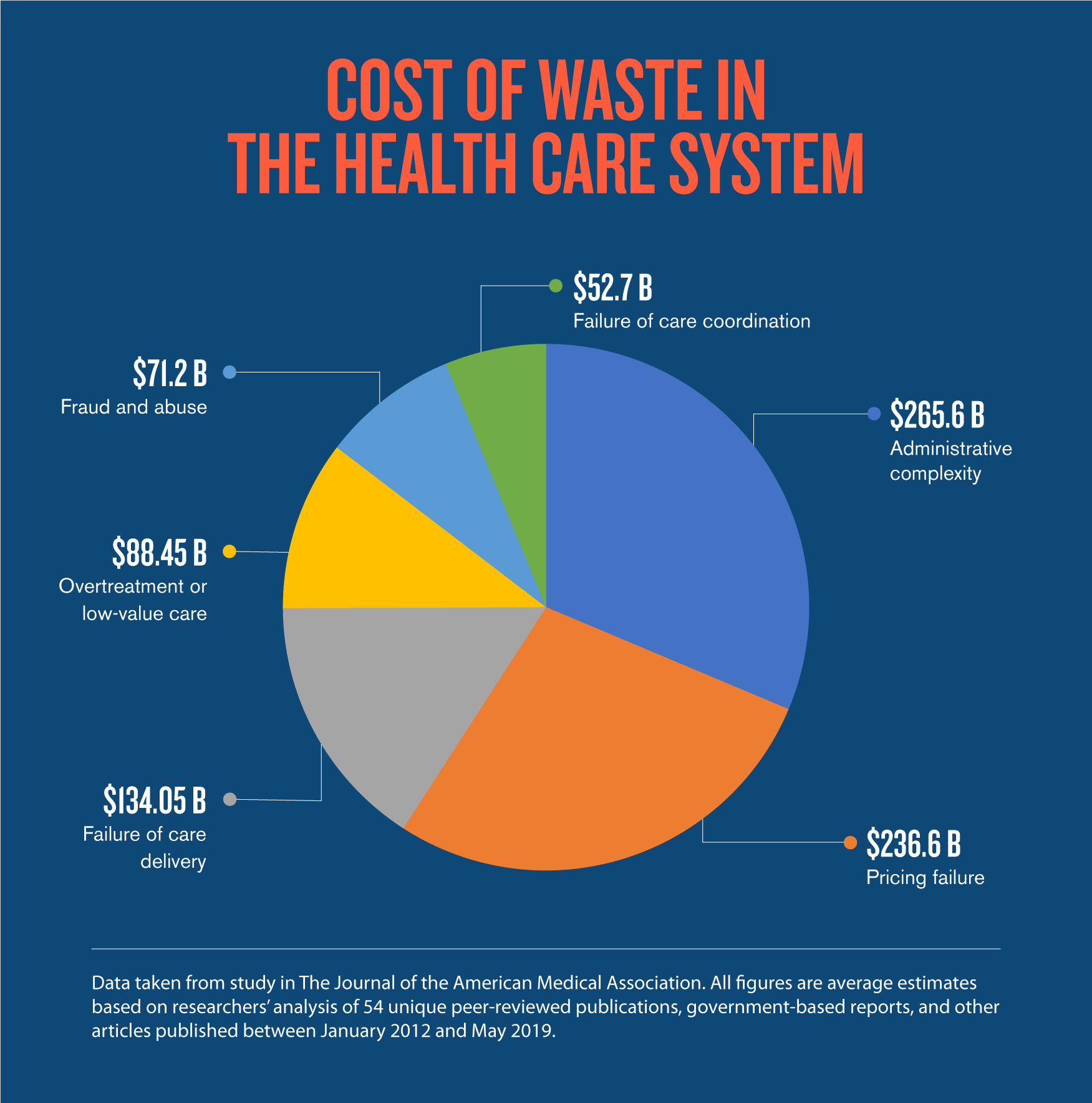
The report identified six areas of waste: failure of care delivery, failure of care coordination, overtreatment or low-value care, pricing failure, fraud and abuse, and administrative complexity.
What causes waste in healthcare?
Waste is caused by factors such as health insurance and medical uncertainties that encourage the production of inefficient and low-value services.
What are the three examples Medicare uses to describe abuse?
Common types of abuse include: Billing for unnecessary services (services that are not medically necessary) Overcharging for services or supplies. Misusing billing codes to increase reimbursement.
What is Medicare fraud, abuse and waste?
Medicare fraud, abuse and waste occur most frequently in the following two methods:
Join the battle against Medicare fraud, abuse and waste!
Detecting Medicare fraud, abuse and waste is easy if you keep an eye out for suspicious activities. Beware of providers that offer services for “free” when you have already given them your Medicare card.
What do I do if I suspect Medicare fraud, abuse and waste?
If you suspect that a provider has committed Medicare fraud, abuse and waste, double check with the provider to be sure it is not a simple mistake first. Sometimes human and computer errors do occur, so give your provider the benefit of the doubt from the start. If these “errors” seem to be happening often, then it is time to take action.
You can help prevent yourself or a loved one from falling victim to Medicare fraud, abuse and waste
By adhering to the following steps and precautions you can prevent yourself from falling victim to Medicare fraud, abuse and waste:
Targeted Probe and Educate
The Centers for Medicare and Medicaid Services (CMS) established the Targeted Probe and Educate (TPE) process in response to physicians concerns about how the Medicare Administrative Contractors (MAC) selected claims for review. TPE uses data analytics to target only those physicians who have high denial rates or unusual billing practices.
Medicare Recovery Audit Contractors (RAC)
Congress created the RAC program to help identify improper Medicare payments. RAC auditors are private contractors paid a commission by the government to:
AMA-Advocated RAC improvements
RACs are required to maintain an accuracy rate of at least 95%. Failure to maintain this accuracy rate will result in a progressive reduction of the RACs ability to request medical records from physicians.
Overturn an audit
For those looking to overturn an audit, the AMA created an Medicare Recovery Audit Contractor Program Appeals Fact Sheet (PDF, members only) to help with the process.
What is Medicare fraud?
The Center for Medicare and Medicaid Services (CMS) states that Medicare fraud is: Intentionally billing Medicare for a service not provided. Billing Medicare at a higher rate. If a provider pays for referrals of Medicare beneficiaries.
What is the difference between fraud and waste?
Differences between Medicare Fraud, Abuse, and Waste. Fraud requires intent to obtain payment and knowing the action is wrong. Abuse creates an unnecessary cost to the Medicare Program, without knowledge. Waste may involve intent or knowledge but could also be unintentional.
What is Medicare program integrity enhancement?
Medicare creates the Program Integrity Enhancements to the Provider Enrollment Process rule to end fraud, waste, and abuse. Basically, Medicare expects providers and suppliers to meet specific standards to remain in the Medicare program.
What to do if you think there is an error in Medicare?
If you think the error is intentional or the doctor admits to an error, you’ll need to report it. An error, intentionally or unintentionally, is Medicare waste.
How long can you go to jail for health care fraud?
Health care fraud is a federal crime with serious consequences. If convicted you could serve up to 10 years in federal prison and pay hefty fines of up to $250,000. If you cause serious bodily harm/injury to someone, 20 years could be added to your sentence. However, if death is involved, you could face life in prison.
Is Medicare fraud a serious issue?
Medicare fraud is a serious issue that you need to report. The Center for Medicare and Medicaid Services says fraud can cost taxpayers billions of dollars . It can also interfere with the health of Medicare beneficiaries. That’s taxpayer money that’s going into the hands of unethical providers.
Can Medicare use your name?
However, if a provider misuses billing codes to increase reimbursement, the doctor commits Medicare abuse. Medicare won’t use your name during the investigation of Medicare fraud, waste, or abuse; if you don’t want them to, you can remain anonymous.
What is heat in Medicare?
The DOJ, OIG, and HHS established HEAT to build and strengthen existing programs combatting Medicare fraud while investing new resources and technology to prevent and detect fraud and abuse . HEAT expanded the DOJ-HHS Medicare Fraud Strike Force, which targets emerging or migrating fraud schemes, including fraud by criminals masquerading as health care providers or suppliers.
Is CPT copyrighted?
CPT codes, descriptions and other data only are copyright 2020 American Medical Association. All Rights Reserved. Applicable FARS/HHSAR apply. CPT is a registered trademark of the American Medical Association. Applicable FARS/HHSAR Restrictions Apply to Government Use. Fee schedules, relative value units, conversion factors and/or related components are not assigned by the AMA, are not part of CPT, and the AMA is not recommending their use. The AMA does not directly or indirectly practice medicine or dispense medical services. The AMA assumes no liability of data contained or not contained herein.
Is there a measure of fraud in health care?
Although no precise measure of health care fraud exists, those who exploit Federal health care programs can cost taxpayers billions of dollars while putting beneficiaries’ health and welfare at risk. The impact of these losses and risks magnifies as Medicare continues to serve a growing number of beneficiaries.
How to report Medicare fraud?
To report abuse, contact 1-800-MEDICARE (633-4227), the Senior Medicare Patrol (SMP) Resource Center (877-808-2468), or the Inspector General’s fraud hotline at 1-800-HHS-TIPS (447-8477). Medicare will not use your name while investigating if you do not want it to.
What are the types of abuse?
Common types of abuse include: 1 Billing for unnecessary services (services that are not medically necessary) 2 Overcharging for services or supplies 3 Misusing billing codes to increase reimbursement