
What does MIPS stand for Medicare?
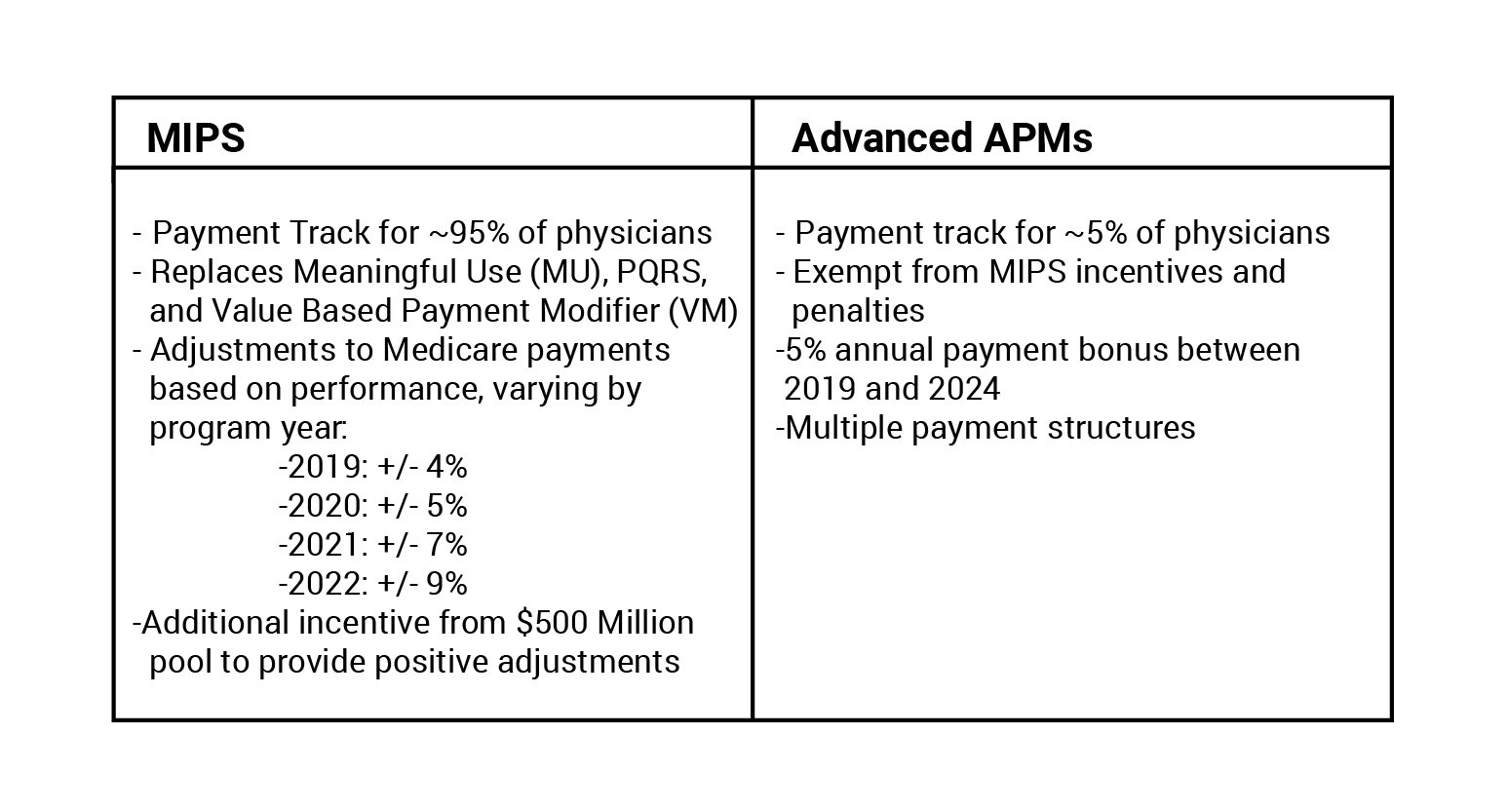
The Merit-based Incentive Payment System (MIPS) is one of two tracks under the Quality Payment Program, which moves Medicare Part B providers to a performance-based payment system. MIPS streamlines three historical Medicare programs — the Physician Quality Reporting System (PQRS), the Value-based Payment Modifier (VM) Program and the Medicare Electronic …
What is MIPS and what is it used for?
Jan 07, 2020 · MIPS (Merit-based Incentive Payment System) The Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) is a federal legislation that required CMS to create the metric-driven Merit-based Incentive Payment System (MIPS) track of the Quality Payment Program to reward clinicians for value over volume based on performance points scored …
What does MIPS stand for medical?
Sep 25, 2016 · What is MIPS? The Merit based Incentive Payment System ( MIPS ), established by the Medicare Access and CHIP Reauthorization Act of 2015 ( MACRA ), came into effect on January 1, 2017. It is a major catalyst towards transforming the healthcare industry from fee-for-service to pay-for-value.
What do you need to know about Macra and MIPS?
What is MIPS? The Merit-based Incentive Payment System (MIPS) is one of the two tracks of the Quality Payment Program, which implements provisions of the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA). Visit QPP.CMS.GOV to understand program basics, including submission timelines and how to participate.
What is the purpose of MIPS?
According to the HHS, “MIPS was designed to tie payments to quality and cost-efficient care, drive improvement in care processes and health outcomes, increase the use of healthcare information, and reduce the cost of care.”Nov 5, 2019
Is MIPS just for Medicare patients?
MIPS reporting of individual measures applies to all patients. Eligibility for a measure is based on CMS documentation (denominator criteria).
What is MIPS eligibility?
In order to be MIPS eligible as an individual clinician, you must: Be identified as a MIPS eligible clinician type on Medicare Part B claims, Have enrolled as a Medicare provider before 2022, Not be a Qualifying Alternative Payment Model Participant (QP), and. Exceed the low-volume threshold as an individual.
How does MIPS payment adjustment work?
MIPS payment adjustments are applied on a per-claim basis. MAOs may apply MIPS payment adjustments either at the time payment is made to a MIPS eligible non-contract clinician for covered professional services furnished during the applicable MIPS payment year or as a retroactive adjustment to paid claims.
Who is exempt from MIPS?
A. A clinician is exempt from MIPS under the Low Volume Threshold if they have fewer than or equal to $90,000 annual allowed Medicare Part B charges and/or see 200 or fewer unique Medicare Part B patients, and/or offer 200 or fewer Medicare services.
What happens if I don't participate in MIPS?
Unless you qualify for an exemption from MIPS in 2022, you will receive a -9% payment adjustment to your Medicare Part B fee-for-service (FFS) claims in 2024.
What is a good MIPS score for 2021?
If you are an EC, MIPS performance in 2021 will determine your MIPS payment adjustment in 2023. Therefore, in 2021, you must achieve at least 60 points through your performance in the four MIPS performance categories to avoid a negative payment adjustment in 2023.Feb 3, 2021
What is a MIPS provider?
Medicare's legacy quality reporting programs were consolidated and streamlined into the Merit-based Incentive Payment System, referred to as "MIPS." This consolidation reduced the aggregate level of financial penalties physicians otherwise faced, and it also provides a greater potential for bonus payments.
What is CMS QPP?
Quality Payment Program Overview. Prior to the Quality Payment Program (QPP), payment increases for Medicare services were set by the Sustainable Growth Rate (SGR) law. This capped spending increases according to the growth in the Medicare population, and a modest allowance for inflation.
How do I find out my MIPS score?
If you submitted 2020 Merit-based Incentive Payment System (MIPS) data, you can now view your performance feedback and MIPS final score on the Quality Payment Program website.
Do I have to participate in MIPS?
MIPS participation is mandatory for therapists who exceed all three low-volume threshold criteria: Billed Medicare for more than $90,000 in Part B allowed charges; Provided care to more than 200 Medicare Part B beneficiaries; and.Dec 11, 2020
What is the penalty for not reporting MIPS?
Avoiding a MIPS penalty can have a huge impact on your bottom line. Penalties for failing 2021 MIPS range up to 9% levied on your 2023 Part B professional service reimbursements.Nov 1, 2021
What is MIPS
The Merit based Incentive Payment System (MIPS), established by the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA), came into effect...
What are the differences between MIPS 2020 and MIPS 2021?
Rules: Low Volume Threshold to be Eligible MIPS 2020: $90,000 in Medicare Part B allowed charges for covered professional services only AND provide...
Who has to report MIPS in 2021?
2021 MIPS eligible clinicians who bill for Medicare Part B (otherwise known as the Physician Fee Schedule) or Critical Access Hospital (CAH) Method...
Can providers participate in MIPS as an individual provider or a group practice?
Providers can choose to participate in MIPS as either: An Individual (defined as a single National Provider Identifier (NPI) tied to a single Tax I...
What are the 2021 MIPS Categories?
Providers participating in the MIPS program will receive a “composite performance score” based on their performance in 4 categories: Quality Qualit...
What determines my final MIPS Score (CPS)?
MIPS COMPOSITE PERFORMANCE SCORE (CPS) - Max Score = 100 points Final MIPS Score = Quality Weighted Score (40%) + PI Weighted Score (25%) + IA Weig...
What impact does MIPS have on my Medicare payments and clinical reputation?
MIPS eligible clinicians will receive neutral, positive or negative payment adjustments based on their composite performance score (CPS). The maxim...
What is the minimum MIPS score I have to acheive to avoid a penalty in 2023?
For 2021 the performance threshold is set at 60 points (increased from 45 in 2020).
Is there flexibility within MIPS for Small Practices?
If reporting as individuals or as a group, and your TIN has 15 or less eligible clinicians (CMS Small Practice Definition: 1-15 eligible clinicians...
How do I get started reporting MIPS through MDinteractive?
You can report 3 categories of MIPS through MDinteractive: Quality Improvement Activities Promoting Inteoperability (requires use of a 2015 certifi...
What is MIPS in Medicare?
MIPS (Merit-based Incentive Payment System) The Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) is a federal legislation that required CMS to create the metric-driven Merit-based Incentive Payment System (MIPS) track of the Quality Payment Program to reward clinicians for value over volume based on performance points scored according ...
How many providers are included in the additional measure for all cause hospital readmissions?
Practices with 16 or more providers and at least 200 eligible cases are included in the additional measure for All-Cause Hospital Readmissions. CMS will calculate this measure from claims data and will score in the same way as the other Quality measures (that have benchmarks), from 3 to 10 points.
What is MIPS point?
As you probably know, each MIPS point a provider earns above the performance threshold (PT) results in higher incentives. Conversely, each MIPS point below the PT, to an established limit, penalizes the provider. Because few providers will receive a zero-payment adjustment resulting from their 2020 MIPS scores, rewards in the 2022 payment year will exceed dollar amounts awarded in the first 3 years of the program.
How does TPCC measure Medicare?
The TPCC measure assesses total Medicare Parts A and B expenditures for a patient attributed to an individual clinician or clinician group during a performance period (Jan. 1 – Dec. 31) by calculating the risk-adjusted, per capita costs. Patients are attributed to a clinician or clinician group based on the amount of primary care services (shown in Table A) they received by their primary care clinician (PCC)—or specialist, if they don’t see a PCC—during the performance period. Attributable patients must reside in the United States and be enrolled in both Medicare Parts A and B (unless newly enrolled) for the full year. The case minimum for this measure is 20 attributable patients.
What is improvement activity?
The Improvement Activities (IA) performance category focuses on care coordination, beneficiary engagement, and patient safety. Changes in Year 4 include two new activities, seven modified activities, and 15 removed activities.
What is episode based measure?
Episode-based measures only look at items and services related to applicable episodes of care, identified by procedure and diagnosis codes reported on Medicare B claims or Medicare Severity Diagnosis-related Group (MS-DRG) codes on Medicare Part A claims.
What is a virtual group?
Virtual Group Reporting: Virtual Groups are composed of solo practitioners and groups of 10 or fewer eligible clinicians, eligible to participate in MIPS, who come together “virtually” with at least 1 other such solo practitioner or group to participate in MIPS for a performance period of a year.
How many measures are in a specialty measure set?
A clinician may choose to report a specialty measure set, defined by CMS for a particular specialty. If a specialty measure set contains fewer than 6 measures, then a clinician could still achieve the maximum possible score for the Quality category by reporting all the measures in the measure set.
When does CMS publish MIPS scores?
MACRA requires CMS to publish each eligible clinician’s annual MIPS score and performance category scores within approximately 12 months after the end of the performance year.
