What is SEP for Medicare?
Sep 23, 2021 · How does SEP OCC work? Language: I would like to diesnroll from either a MAPD or PDP to enroll in a a MA-only plan because I receive or will receive other creditable drug coverage, such as VA or Tribal benefits. Timeline: One-time use, or 2 months after disenrollment from a MAPD or PDP. Special Notes: Currently only accepted by UHC and Humana ...
When should I sign up for Medicare?
Special circumstances (Special Enrollment Periods) You can make changes to your Medicare Advantage and Medicare prescription drug coverage when certain events happen in your life, like if you move or you lose other insurance coverage. These chances to make changes are called Special Enrollment Periods (SEPs).
What is the initial enrollment period for Medicare?
Nov 24, 2021 · A Special Enrollment Period (SEP) is an enrollment period that takes place outside of the annual Medicare enrollment periods, such as the annual Open Enrollment Period. They are granted to people who were prevented from enrolling in Medicare during the regular enrollment period for a number of specific reasons.
When will my Medicare coverage start?
Aug 18, 2021 · Medicare Special Enrollment Periods. There are multiple life events that can make you eligible for a Special Enrollment Period. A SEP allows you to make changes to your Medicare coverage outside the standard enrollment periods. Below, we’ll go over the most common Special Enrollment Periods for Medicare.

What is Sep OCC?
Page Content.
What is OCC in Medicare?
What is OCC coverage? The Traditional Indemnity option includes a $50,000 lifetime maximum benefit on those services designated as OCC. Medicare-eligible retirees and their covered dependent(s) can purchase (buy-up) additional OCC coverage for an additional level of insurance.
What is the 8 month SEP for Medicare Part B?
What is the Medicare Part B special enrollment period (SEP)? The Medicare Part B SEP allows you to delay taking Part B if you have coverage through your own or a spouse's current job. You usually have 8 months from when employment ends to enroll in Part B.Mar 7, 2020
What is a Sep 65?
People who enroll in a Medicare Advantage plan when they are first eligible for Medicare Part A at age 65 get a “trial period” (up to 12 months) to try out Medicare Advantage. This SEP allows them to disenroll from their first Medicare Advantage plan and go to Original Medicare.
What does OCC mean in insurance?
Occupational Accident Insurance is a type of contingent liability insurance that provides coverage for the owner-operator who may be leased onto a motor carrier.
How long is SEP for Medicare?
Your chance to join lasts for 2 full months after you drop your Medicare Cost Plan.
Are you automatically enrolled in Medicare if you are on Social Security?
Yes. If you are receiving benefits, the Social Security Administration will automatically sign you up at age 65 for parts A and B of Medicare. (Medicare is operated by the federal Centers for Medicare & Medicaid Services, but Social Security handles enrollment.)
What does Sep mean in Social Security?
Special Enrollment PeriodYou may qualify for a "Special Enrollment Period" (SEP) that will let you sign up for Part B: During any month you remain covered under the group health plan and your, or your spouse's, current employment continues; or.Jun 7, 2021
Do I automatically get Medicare when I turn 65?
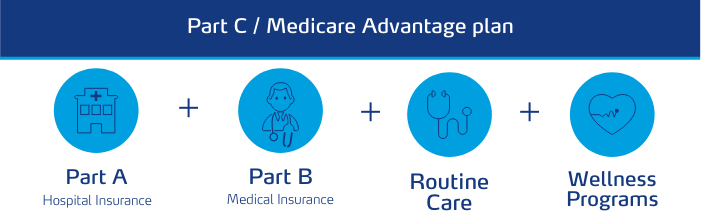
You automatically get Medicare when you turn 65 Part A covers inpatient hospital stays, skilled nursing facility care, hospice care, and some home health care. Part B covers certain doctors' services, outpatient care, medical supplies, and preventive services.
What is the proper hierarchy of Medicare election periods?
If this is you, your first chance to sign up for Medicare is usually your Initial Enrollment Period, goes for seven months. It starts three months before your 65th birthday, includes the month of your 65th birthday, and ends three months later.
What are the 3 enrollment periods for Medicare?
When you turn 65, you have a seven month window to enroll in Medicare. This includes three months before the month you turn 65, your birth month, and three months after the month you turn 65.
How many times can you use an SEP?
You have an SEP to choose once per year, at any time during the year, to join a Medicare Advantage Plan or Part D plan for the first time or to change to another Medicare Advantage Plan or Part D plan, including joining one that works with your SPAP.Jan 1, 2022
When is the open enrollment period for Medicare?
Learn more and use this guide to help you sign up for Medicare. Open Enrollment: The fall Medicare Open Enrollment Period has officially begun and lasts from October 15 to December 7, 2020. You may be able to enroll in ...
What is a special enrollment period?
A Special Enrollment Period (SEP) is an enrollment period that takes place outside of the annual Medicare enrollment periods, such as the annual Open Enrollment Period. They are granted to people who were prevented from enrolling in Medicare during the regular enrollment period for a number of specific reasons.
How often can you change your Medicare Advantage plan?
If you move into, out of, or currently reside in a facility of special care such as a skilled nursing home or long-term care hospital, you may enroll in, disenroll from, or change a Medicare Advantage plan one time per month.
Who is Christian Worstell?
Christian Worstell is a licensed insurance agent and a Senior Staff Writer for MedicareAdvantage.com. He is passionate about helping people navigate the complexities of Medicare and understand their coverage options. .. Read full bio
What happens if you don't enroll in Medicare at 65?
If you did not enroll in Medicare when you turned 65 because you were still employed and were covered by your employer’s health insurance plan, you will be granted a Special Enrollment Period.
How long do you have to disenroll from Medicare Advantage?
If you enrolled in a Medicare Advantage plan when you first became eligible for Medicare, you have 12 months to disenroll from the plan and transition back to Original Medicare.
How long does it take to switch to another Medicare Advantage plan?
If you permanently move out of your Medicare Advantage plan’s coverage area or move to an area with more available plans, you may switch to another Medicare Advantage plan beginning the month before your move and lasting for two months.
What is a SEP for Medicare?
A SEP allows you to make changes to your Medicare coverage outside the standard enrollment periods. Below, we’ll go over the most common Special Enrollment Periods for Medicare.
How long does a SEP last?
Your SEP starts the month the company knows of the move and lasts for two months after.
What are the dates for a symlink?
You can do this once throughout the following dates: 1 January-March 2 April-June 3 July-September
How long does Medicare coverage last after you lose it?
This Special Enrollment Period continues for two full months after the month you lose your drug coverage, or you get a notification.
Who is Lindsay Malzone?
Lindsay Malzone is the Medicare expert for MedicareFAQ. She has been working in the Medicare industry since 2017. She is featured in many publications as well as writes regularly for other expert columns regarding Medicare.
How long does it take for Medicare to end?
Contract ends early. Those that have a health plan coming to an end in the middle of the contract year can switch to another Medicare plan two months before the contract ending and up to one full month after it ends if the policy isn’t for another contract year.
Can you change your medicaid plan?
When eligible for Medicare and Medicaid, you can choose to change plans, whether it be switching, joining, or dropping plans. Changing plans is an option because dual-eligibility and low-income subsidy qualify you for a Special Enrollment Period.
What are the qualifying events for SEP?
Consumers may qualify for an SEP to enroll in or change plans if they experience a qualifying event in one (1) of the following six (6) categories: 1. Loss of qualifying health coverage 2. Change in household size 3. Change in primary place of living 4.
How long does a SEP last?
Consumers who experience a qualifying event can enroll in or change plans through an SEP. • SEPs provide a pathway to coverage. • Most SEPs last 60 days from the date of the qualifying event. • A qualifying event can occur at any point during the year outside of Open Enrollment. 5.
When did Emma leave her job?
Emma recently decided to leave her job to start her own business. She left her job on April 5, 2016, and her employer-sponsored coverage ended at the end of the month, on April 28.
Can a consumer qualify for SEP?
consumer may qualify for an SEP if he or she (or anyone in his or her household) has a change in his or her primary place of living and gains access to new QHPs as a result. This includes: