Under the outpatient prospective payment system, hospitals are paid a set amount of money (called the payment rate) to give certain outpatient services to people with Medicare. For most services, you must pay the yearly Part B deductible before Medicare pays its share. Once you meet the deductible, Medicare pays most of the total payment and you pay a copayment. For some services, you don’t need to meet the yearly Part B deductible before Medicare pays (for example, for a screening mammography). The payment rate isn’t the same for all hospitals because it’s adjusted to reflect what people are paid to work in the area where the hospital is located. Also, each year the rate is adjusted for other factors.
How do I get hospital Medicare reimbursement?
You usually pay 20% of the Medicare-Approved Amount for the doctor's or other health care provider's services. You may pay more for outpatient services you get in a hospital than you’ll pay for the same care in a doctor’s office. However, the hospital outpatient copayment for the service is capped at the inpatient deductible amount.
How does Medicare reimburse hospitals?
The Outpatient Prospective Payment System (OPPS) is a Medicare reimbursement methodology used to determine fees for Part B outpatient services. Also called Hospital OPPS or HOPPS, the OPPS was mandated as part of the Balanced Budget Act of 1997 to ensure appropriate payment of services and delivery of quality medical care to patients.
What does inpatient versus outpatient mean for Medicare?
Your hospital status—whether you're an inpatient or an outpatient—affects how much you pay for hospital services (like X-rays, drugs, and lab tests ). Your hospital status may also affect whether Medicare will cover care you get in a skilled nursing facility (SNF) following your hospital stay. You're an inpatient starting when you're ...
Can a hospital refuse to bill Medicare?
Under the outpatient prospective payment system, hospitals are paid a set amount of money (called the payment rate) to give certain outpatient services to people with Medicare. For most services, you must pay the yearly Part B deductible before Medicare pays its share. Once you meet the deductible, Medicare pays most of the
How is Medicare outpatient reimbursement calculated?
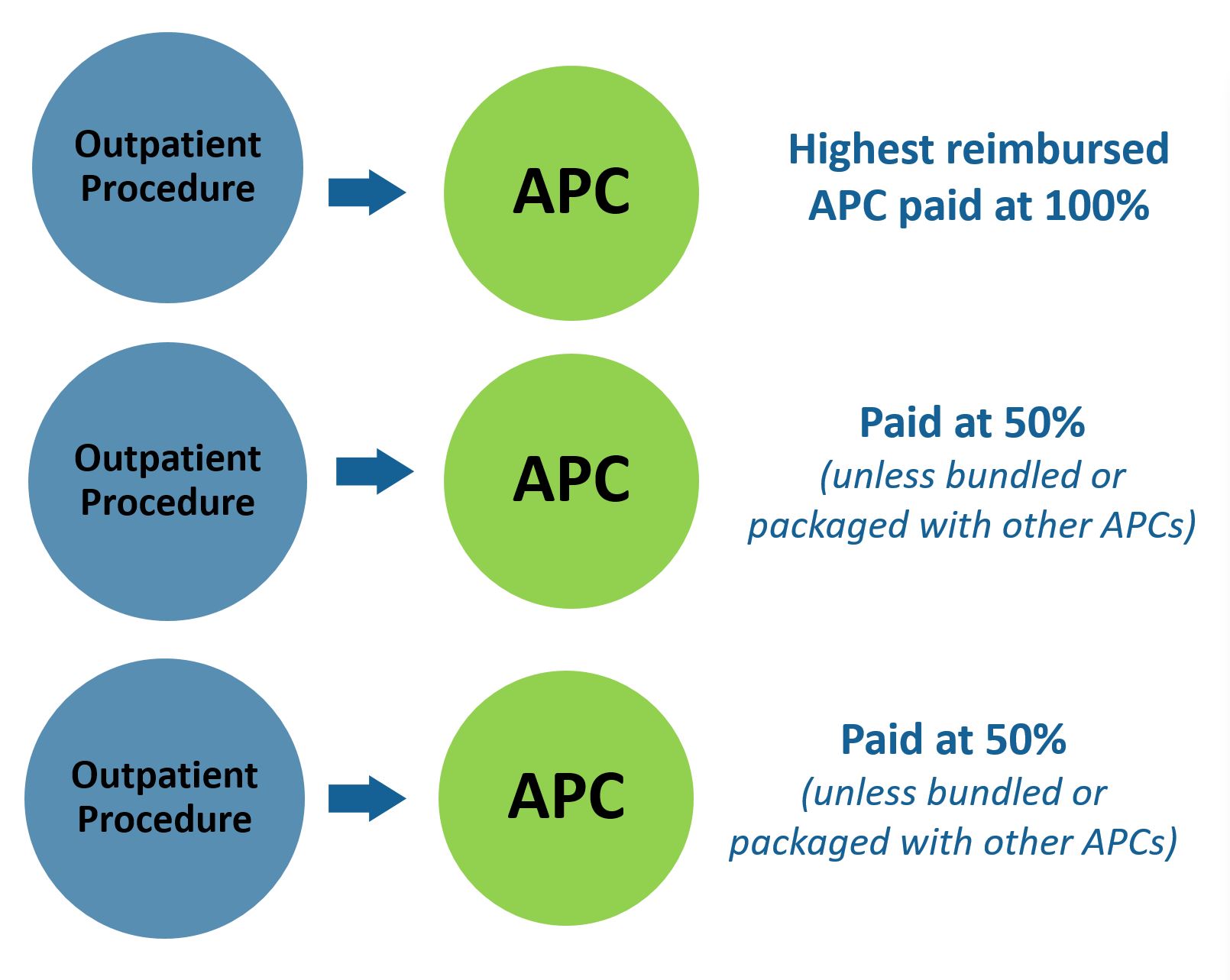
The payments are calculated by multiplying the APCs relative weight by the OPPS conversion factor and then there is a minor adjustment for geographic location. The payment is divided into Medicare's portion and patient co-pay. Co-pays vary between 20 and 40% of the APC payment rate.
Does Medicare pay for outpatient care?
Medicare Part B covers medically necessary outpatient hospital care, which is care you receive when you have not been formally admitted to the hospital as an inpatient. Covered services include but are not limited to: Observation services. Emergency room and outpatient clinic services, including same-day surgery.
What reimbursement system is associated with the Medicare outpatient prospective payment system?
The Hospital Outpatient Prospective Payment System (HOPPS) is used by CMS to reimburse for hospital outpatient services. The CMS created HOPPS to reduce beneficiary copayments in response to rapidly growing Medicare expenditures for outpatient services and large copayments being made by Medicare beneficiaries.
How does Medicare define outpatient?
You're an outpatient if you're getting emergency department services, observation services, outpatient surgery, lab tests, X-rays, or any other hospital services, and the doctor hasn't written an order to admit you to a hospital as an inpatient.
What are examples of outpatient services?
What Are Outpatient Services?Wellness and prevention services, such as psychological counseling and weight-loss programs.Diagnostic services, such as blood and urine lab tests, x-rays, and cranial scans, like MRIs and CATS.Treatments such as some surgeries and chemotherapy; and.Rehabilitation such as physical therapy.
Which of the following applies to Medicare coverage that pays for outpatient services?
Part B covers certain doctors' services, outpatient care, medical supplies, and preventive services.
How does Medicare reimbursement work?
Medicare pays for 80 percent of your covered expenses. If you have original Medicare you are responsible for the remaining 20 percent by paying deductibles, copayments, and coinsurance. Some people buy supplementary insurance or Medigap through private insurance to help pay for some of the 20 percent.
What is the difference between APC and opps?
APCs are used in outpatient surgery departments, outpatient clinic emergency departments, and observation services. An OPPS payment status indicator is assigned to every CPT/HCPCS code and the indicators identify if the code is paid under OPPS and if it is a separate or packaged code.
What is the main difference between APC and DRG?
The unit of classification for DRGs is an admission while APCs utilize a visit. The initial variable used in the classification process is the diagnosis for DRGs and the procedure for APCs. Only one DRG is assigned per admission, while APCs assign one or more APCs per visit.
What's the difference between inpatient and outpatient?
Outpatient care is cheaper as costs typically only need to cover the doctor and any tests you need to undergo. When you're admitted to hospital as an inpatient, factors like the use of facilities and any equipment necessary to monitor your health come into play on top of what outpatient care would cost.
What is the 2 Midnight Rule Medicare?
The Two-Midnight rule, adopted in October 2013 by the Centers for Medicare and Medicaid Services, states that more highly reimbursed inpatient payment is appropriate if care is expected to last at least two midnights; otherwise, observation stays should be used.
How does Medicare explain Outpatient observation Notice?
The notice must explain the reason that the patient is an outpatient (and not an admitted inpatient) and describe the implications of that status both for cost-sharing in the hospital and for subsequent “eligibility for coverage” in a skilled nursing facility (SNF).
What is outpatient reimbursement?
Outpatient facility reimbursement is the money the hospital or other facility receives for supplying the resources needed to perform procedures or services in their facility. The resources typically include the room, nursing staff, supplies, medications, and other items and staffing the facility bears the cost for. The facility captures the charges and codes, typically on the UB-04 claim form, and sends the claim to the payer for reimbursement.
What is the code for a Medicare outpatient clinic?
When a Medicare patient is evaluated in the outpatient hospital clinic, the clinic visit is coded using HCPCS Level II code G0463 Hospital outpatient clinic visits for assessment and management instead of the standard E/M CPT ® code (99202-99215) a pro-fee coder uses when reporting professional fee services.
What are the three coding systems used in outpatient facilities?
The three main coding systems used in the outpatient facility setting are ICD-10-CM, CPT ®, and HCPCS Level II. These are often referred to as code sets.
How does coding for outpatient surgery affect reimbursement?
As an example, suppose a patient with Medicare presents for a same-day surgery in an outpatient hospital setting. Coding for outpatient services affects reimbursement because the facility bills CPT ® code (s) for the surgery on the UB-04 claim form to be reimbursed for the resources (room cost, nursing staff, etc.) based on the APCs under the OPPS system. The surgeon that performed the surgery will bill the same CPT ® code (s) and any applicable modifiers for the professional work (pro-fee) on the CMS-1500 claim form. The pro-fee reimbursement for that claim is based on the relative value units (RVUs) on the MPFS. The final payment is calculated by multiplying the RVUs by the associated conversion factor, with a slight adjustment based on the geographic location.
What is an outpatient facility?
Outpatient facility coding is the assignment of ICD-10-CM, CPT ®, and HCPCS Level II codes to outpatient facility procedures or services for billing and tracking purposes. Examples of outpatient settings include outpatient hospital clinics, emergency departments (EDs), ambulatory surgery centers (ASCs), and outpatient diagnostic and testing departments (such as laboratory, radiology, and cardiology).
What is the CPT code for a gastroenterologist?
The specialist then bills the professional fee using the appropriate outpatient consultation CPT ® code (99241-99245) or other appropriate E/M code based on payer guidelines. (Medicare, for instance, no longer accepts the consult codes, and providers and coders should check with their individual payers to determine the appropriate codes for billing consultations.)
What is the role of ICD-10 codes in the outpatient process?
The role of diagnosis codes in the outpatient reimbursement process is to support the medical necessity of the services provided. Consequently, complete and accurate assignment of ICD-10-CM codes is essential to the outpatient reimbursement process. The ICD-10-CM code set is updated annually in October by the Centers for Disease Control and Prevention (CDC) National Center for Health Statistics (NCHS). In rare cases, ICD-10-CM codes are implemented on dates other than Oct. 1.
What is deductible in Medicare?
deductible. The amount you must pay for health care or prescriptions before Original Medicare, your prescription drug plan, or your other insurance begins to pay. , coinsurance. An amount you may be required to pay as your share of the cost for services after you pay any deductibles.
How does hospital status affect Medicare?
Inpatient or outpatient hospital status affects your costs. Your hospital status—whether you're an inpatient or an outpatient—affects how much you pay for hospital services (like X-rays, drugs, and lab tests ). Your hospital status may also affect whether Medicare will cover care you get in a skilled nursing facility ...
What is an inpatient hospital admission?
The decision for inpatient hospital admission is a complex medical decision based on your doctor’s judgment and your need for medically necessary hospital care. An inpatient admission is generally appropriate when you’re expected to need 2 or more midnights of medically necessary hospital care. But, your doctor must order such admission and the hospital must formally admit you in order for you to become an inpatient.
What is an ED in hospital?
You're in the Emergency Department (ED) (also known as the Emergency Room or "ER") and then you're formally admitted to the hospital with a doctor's order. Outpatient until you’re formally admitted as an inpatient based on your doctor’s order. Inpatient after your admission.
How long does an inpatient stay in the hospital?
Inpatient after your admission. Your inpatient hospital stay and all related outpatient services provided during the 3 days before your admission date. Your doctor services. You come to the ED with chest pain, and the hospital keeps you for 2 nights.
What is a copayment?
copayment. An amount you may be required to pay as your share of the cost for a medical service or supply, like a doctor's visit, hospital outpatient visit, or prescription drug. A copayment is usually a set amount, rather than a percentage. For example, you might pay $10 or $20 for a doctor's visit or prescription drug.
Is observation an outpatient?
In these cases, you're an outpatient even if you spend the night in the hospital. Observation services are hospital outpatient services you get while your doctor decides whether to admit you as an inpatient or discharge you. You can get observation services in the emergency department or another area of the hospital.
What rights do you have if you have Medicare?
If you have Medicare, you have certain guaranteed rights to help protect you. One of these is the right to appeal. You may want to appeal in any of these situations:
What happens if you pay less than the amount on your Medicare summary notice?
If you paid less than the amount listed on your “Medicare Summary Notice”, the hospital or community mental health center may bill you for the difference if you don’t have another insurer who’s responsible for paying your deductible and copayments.
Spotlights
CMS issued the CY 2022 OPPS/ASC final rule and related files that update Medicare payment rates, quality reporting programs, and policies. See a summary of key provisions, effective January 1, 2022:
Hospital Center
For a one-stop resource web page focused on the informational needs and interests of Medicare Fee-for-Service (FFS) hospitals, go to the Hospital Center (see under "Related Links Inside CMS" below). Mailbox: [email protected].
What is an outpatient hospital?
A part of a hospital where you get outpatient services, like an observation unit, surgery center, or pain clinic.
What is an ambulatory surgical center?
ambulatory surgical centers. A non-hospital facility where certain surgeries may be performed for patients who aren’t expected to need more than 24 hours of care. and. hospital outpatient departments. A part of a hospital where you get outpatient services, like an observation unit, surgery center, or pain clinic.
What is Medicare reimbursement form?
The Medicare reimbursement form, also known as the “Patient’s Request for Medical Payment, ” is available in both English and Spanish on the Medicare website.
What if my doctor doesn't bill Medicare?
If your doctor doesn’t bill Medicare directly, you can file a claim asking Medicare to reimburse you for costs that you had to pay.
How long does it take for Medicare to process a claim?
Medicare claims to providers take about 30 days to process. The provider usually gets direct payment from Medicare. What is the Medicare Reimbursement fee schedule? The fee schedule is a list of how Medicare is going to pay doctors. The list goes over Medicare’s fee maximums for doctors, ambulance, and more.
What is Part D insurance?
Part D is prescription drug coverage provided by private insurance companies. These drug companies establish their own rules about which drugs are covered and what you will pay out-of-pocket.
Does Medicare cover out of network doctors?
Coverage for out-of-network doctors depends on your Medicare Advantage plan. Many HMO plans do not cover non-emergency out-of-network care, while PPO plans might. If you obtain out of network care, you may have to pay for it up-front and then submit a claim to your insurance company.
Do participating doctors accept Medicare?
Most healthcare doctors are “participating providers” that accept Medicare assignment. They have agreed to accept Medicare’s rates as full payment for their services. If you see a participating doctor, they handle Medicare billing, and you don’t have to file any claim forms.
Do you have to pay for Medicare up front?
But in a few situations, you may have to pay for your care up-front and file a claim asking Medicare to reimburse you. The claims process is simple, but you will need an itemized receipt from your provider.
Zipcode to Carrier Locality File
This file is primarily intended to map Zip Codes to CMS carriers and localities. This file will also map Zip Codes to their State. In addition, this file contains an urban, rural or a low density (qualified) area Zip Code indicator.
Provider Center
For a one-stop resource web page focused on the informational needs and interests of Medicare Fee-for-Service (FFS) providers, including physicians, other practitioners and suppliers, go to the Provider Center (see under "Related Links" below).