What are the advantages of Medicare Advantage?
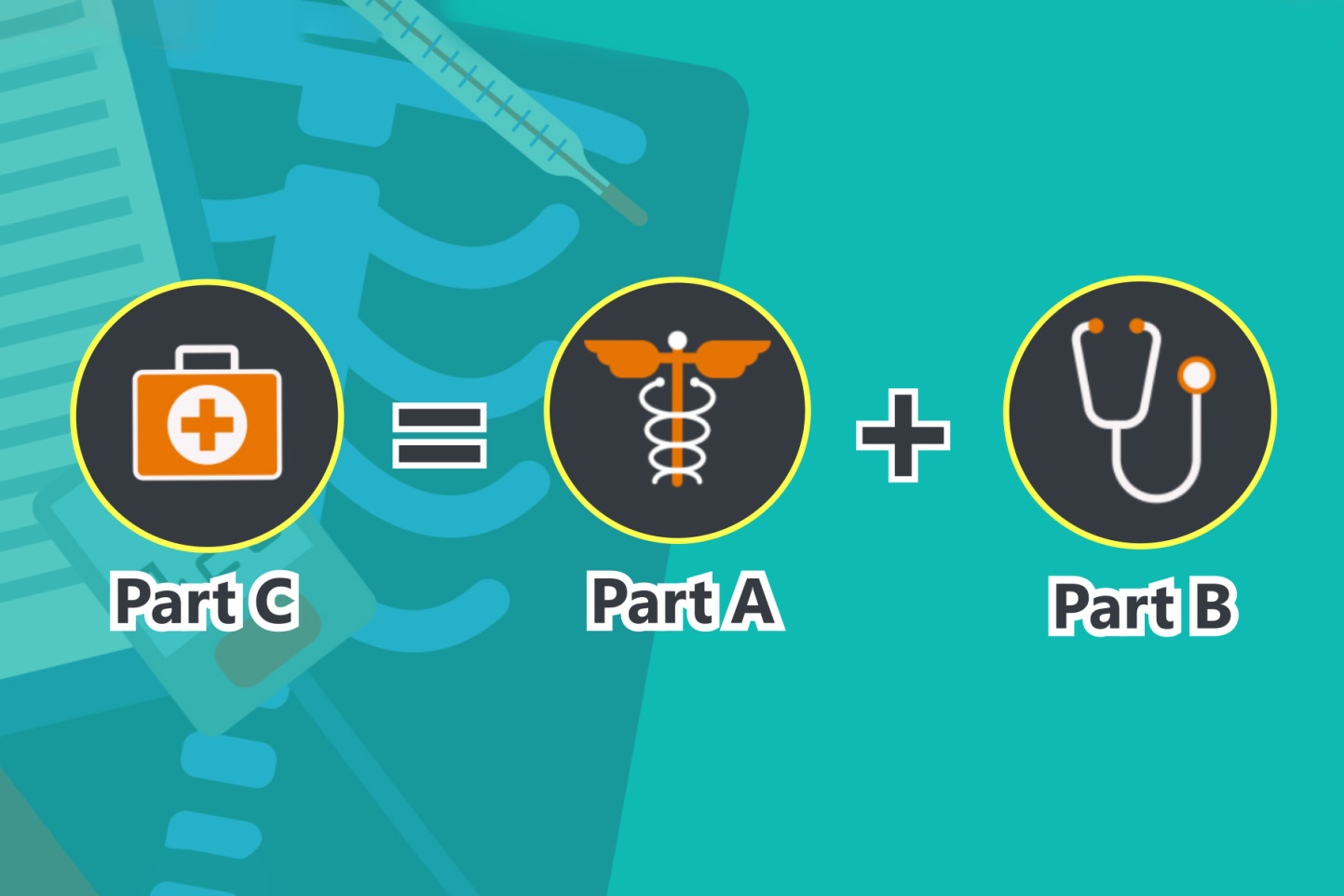
Aug 03, 2021 · Medicare Advantage Plans, sometimes called “Part C” or “MA Plans,” are offered by private companies approved by Medicare. If you join a Medicare Advantage Plan, the plan will provide all of your Part A (Hospital Insurance) and Part B (Medical Insurance) coverage. Medicare Advantage Plans may offer extra coverage, such as vision, hearing, dental, and/or health and …
Is Medicare Advantage worth it?
Apr 15, 2020 · Summary: Medicare Part C, also known as Medicare Advantage, is an alternative way to get your Original Medicare benefits. These plans often offer additional coverage for services like prescription drugs, vision and dental care. Plans vary in …
What are the pros and cons of Medicare Advantage plans?
Medicare Advantage (Part C) has more coverage for routine healthcare that you use every day. Medicare Advantage plans may include: Routine dental care including X-rays, exams, and dentures Vision care including glasses and contacts Hearing care including testing and hearing aids Wellness programs and fitness center memberships
What are the requirements for Medicare Advantage?
Jan 25, 2022 · No, signing up for Medicare Part C – Medicare Advantage is voluntary and there is not a direct penalty for signing up late. However, there is a penalty for signing up late for Part A and B, and due to the fact Part C bundles Original Medicare Part A and B into one plan, you may face the penalties associated with Part A and B when you sign up for Part C.

Is Medicare Part C the same as Medicare Advantage?
A Medicare Advantage is another way to get your Medicare Part A and Part B coverage. Medicare Advantage Plans, sometimes called "Part C" or "MA Plans," are offered by Medicare-approved private companies that must follow rules set by Medicare.
What is covered by Medicare Part C?
Medicare Part C inpatient coverage inpatient hospital care. inpatient mental health services. inpatient rehabilitation services. hospice care.
Is Medicare Part C required?
Medicare Part C, also called Medicare Advantage, is an insurance option for people who are eligible for Medicare. These plans are offered through private insurance companies. You don't need to buy a Medicare Part C plan. It's an alternative to original Medicare that offers additional items and services.
Is Medicare Part C the same as supplemental insurance?
These are also called Part C plans. Medicare Supplement insurance policies, also called Medigap, help pay the out-of-pocket expenses not covered by Original Medicare (Part A and B). It is not part of the government's Medicare program, but provides coverage in addition to it.Oct 1, 2021
What is the difference between Medicare Part C and Part D?
Medicare part C is called "Medicare Advantage" and gives you additional coverage. Part D gives you prescription drug coverage.
Can you switch back and forth between Medicare and Medicare Advantage?
If you currently have Medicare, you can switch to Medicare Advantage (Part C) from Original Medicare (Parts A & B), or vice versa, during the Medicare Annual Enrollment Period. If you want to make a switch though, it may also require some additional decisions.
At what age will a person normally enroll with an insurance carrier under a Part C Medicare Advantage Plan?
People can enroll in Original Medicare if they are 65 years of age or older and are a citizen of the United States or have been a legal permanent resident for at least 5 years. Specific rules apply to those younger than 65 who have certain illnesses or disabilities. Read more about eligibility under the age of 65 here.May 11, 2020
Does Medicare Part C cover prescriptions?
Unlike Original Medicare, Medicare Part C generally offers coverage for prescription drugs you take at home. The exact prescription drugs that are covered are listed in the plan's formulary. Formularies may vary from plan to plan.
Which company has the best Medicare Advantage plan?
List of Medicare Advantage plansCategoryCompanyRatingBest overallKaiser Permanente5.0Most popularAARP/UnitedHealthcare4.2Largest networkBlue Cross Blue Shield4.1Hassle-free prescriptionsHumana4.01 more row•Feb 16, 2022
Which two Medicare plans Cannot be enrolled together?
You generally cannot enroll in both a Medicare Advantage plan and a Medigap plan at the same time.Jun 2, 2021
What is the biggest difference between Medicare and Medicare Advantage?
Original Medicare covers inpatient hospital and skilled nursing services – Part A - and doctor visits, outpatient services and some preventative care – Part B. Medicare Advantage plans cover all the above (Part A and Part B), and most plans also cover prescription drugs (Part D).
How long before you turn 65 do you apply for Medicare?
3 monthsGenerally, you're first eligible starting 3 months before you turn 65 and ending 3 months after the month you turn 65. If you don't sign up for Part B when you're first eligible, you might have to wait to sign up and go months without coverage. You might also pay a monthly penalty for as long as you have Part B.
What is Medicare Advantage Part C?
Find Plans. Find Plans. Summary: Medicare Part C, also known as Medicare Advantage, is an alternative way to get your Original Medicare benefits. These plans often offer additional coverage for services like prescription drugs, vision and dental care. Plans vary in terms of both cost and benefits.
What are the parts of Medicare?
There are four basic parts to Medicare. Part A and Part B make up Original Medicare. Part A covers care you receive while you are in the hospital. Part B helps pay for expenses, like doctor visits and some medical equipment. Medicare Part C is an alternative way to get your Original Medicare coverage.
When do you enroll in Medicare?
This is the period when you first become eligible for Medicare. This enrollment period begins three months before the month you turn 65. It includes your birthday month and the three months following.
When can I switch Medicare Advantage plans?
This period runs annually from January 1 to March 31. During this time, you can switch from one Medicare Advantage plan to another.
What is a Silversneaker?
Wellness programs called SilverSneakers. Prescription medications. Medicare Part C plans can also offer additional benefits today, such as over-the-counter medications, transportation to and from doctor appointments, and adult daycare services.
Is Medicare Part D a stand alone plan?
Medicare Part D is prescription drug coverage. You can have a stand-alone prescription drug plan with Original Medicare, or you might have a Medicare Advantage plan that includes prescription medication benefits.
What is MSA plan?
Medicare Medical Savings Account (Msa) Plan. MSA Plans combine a high deductible Medicare Advantage Plan and a bank account. The plan deposits money from Medicare into the account. You can use the money in this account to pay for your health care costs, but only Medicare-covered expenses count toward your deductible.
What is a special needs plan?
Special Needs Plans (SNPs) Other less common types of Medicare Advantage Plans that may be available include. Hmo Point Of Service (Hmopos) Plans. An HMO Plan that may allow you to get some services out-of-network for a higher cost. and a. Medicare Medical Savings Account (Msa) Plan.
Does Medicare Advantage include drug coverage?
Most Medicare Advantage Plans include drug coverage (Part D). In many cases , you’ll need to use health care providers who participate in the plan’s network and service area for the lowest costs.
What is a copayment in Medicare?
Copays. A copayment may apply to specific services, such as doctor office visits. Coinsurance. Cost sharing amounts may apply to specific services. Out-of-Pocket Expenses. All Medicare Advantage plans have an annual limit on your out-of-pocket expenses, which is a feature not available through Original Medicare.
How to change Medicare plan?
The Medicare Open Enrollment Period provides an annual opportunity to review, and if necessary, change your Medicare coverage options. Coverage becomes effective on January 1. During Open Enrollment, some examples of changes that you can make include: 1 Join a Medicare Advantage (Part C) plan. 2 Discontinue your Medicare Advantage plan and return to Original Medicare (Part A and Part B). 3 Change from one Medicare Advantage plan to another. 4 Add or Change your Prescription Drug Coverage (Part D) plan if you are in Original Medicare.
What is the initial enrollment period for Medicare?
The Initial Enrollment Period is a limited window of time when you can enroll in Original Medicare (Part A and/or Part B) when you are first eligible. After you are enrolled in Medicare Part A and Part B, you can select other coverage options like a Medicare Advantage plan from approved private insurers.
Do you have to enroll in Medicare before joining a Medicare Advantage plan?
You must first enroll in Medicare Part A and Part B before joining a Medicare Advantage plan. Contact your local Blue Cross Blue Shield company for help choosing a Medicare Advantage plan and getting enrolled.
What happens if you get a health care provider out of network?
If you get health care outside the plan’s network, you may have to pay the full cost. It’s important that you follow the plan’s rules, like getting prior approval for a certain service when needed. In most cases, you need to choose a primary care doctor. Certain services, like yearly screening mammograms, don’t require a referral. If your doctor or other health care provider leaves the plan’s network, your plan will notify you. You may choose another doctor in the plan’s network. HMO Point-of-Service (HMOPOS) plans are HMO plans that may allow you to get some services out-of-network for a higher copayment or coinsurance. It’s important that you follow the plan’s rules, like getting prior approval for a certain service when needed.
What is a special needs plan?
Special Needs Plan (SNP) provides benefits and services to people with specific diseases, certain health care needs, or limited incomes. SNPs tailor their benefits, provider choices, and list of covered drugs (formularies) to best meet the specific needs of the groups they serve.
Can a provider bill you for PFFS?
The provider shouldn’t provide services to you except in emergencies, and you’ll need to find another provider that will accept the PFFS plan .However, if the provider chooses to treat you, then they can only bill you for plan-allowed cost sharing. They must bill the plan for your covered services. You’re only required to pay the copayment or coinsurance the plan allows for the types of services you get at the time of the service. You may have to pay an additional amount (up to 15% more) if the plan allows providers to “balance bill” (when a provider bills you for the difference between the provider’s charge and the allowed amount).
Do providers have to follow the terms and conditions of a health insurance plan?
The provider must follow the plan’s terms and conditions for payment, and bill the plan for the services they provide for you. However, the provider can decide at every visit whether to accept the plan and agree to treat you.