
What is the Qualified Medicare beneficiary program (QMB)?
The Qualified Medicare Beneficiary (QMB) program provides Medicare coverage of Part A and Part B premiums and cost sharing to low-income Medicare beneficiaries. In 2017, 7.7 million people (more than one out of eight people with Medicare) were in the QMB program.
How to apply for a Qualified Medicare beneficiary program?
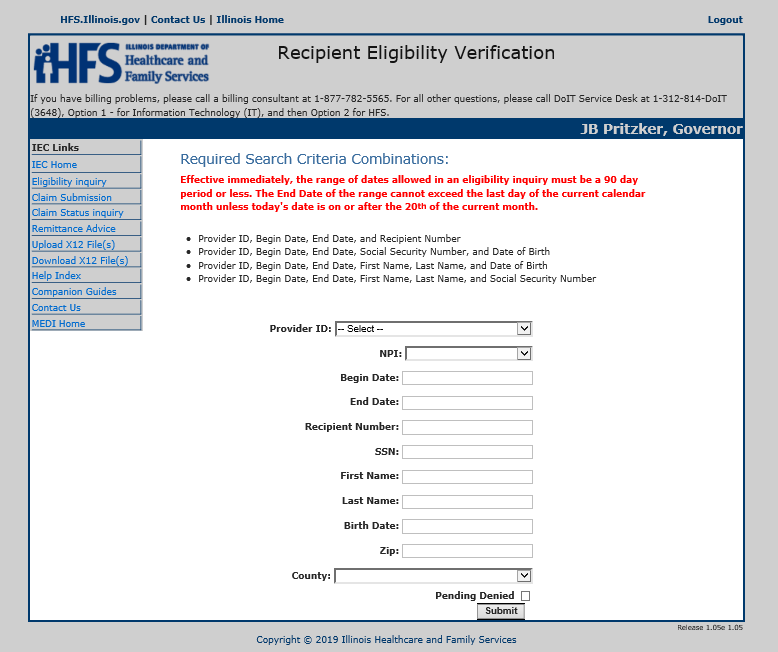
How to Apply for a Qualified Medicare Beneficiary Program. Anyone interested in applying for a QMB program must contact their state’s Medicaid office. If your income is higher than the QMB requirements, you should still reach out to determine eligibility. Each state’s Medicaid program pays the Medicare cost-sharing for QMB program members.
Who is eligible for a Qualified Medicare beneficiary program in 2021?
Who is Eligible for a Qualified Medicare Beneficiary Program in 2021? To be eligible for a QMB program, you must qualify for Part A. Your monthly income must be at or below $1,084 as an individual and $1,457 as a married couple.
What is the income limit for the Qualified Medicare beneficiary program?
The income limit for the Qualified Medicare Beneficiary (QMB) Program is 100 percent of the federal poverty level. The QMB helps pay Medicare Part A premiums, Medicare Part B premiums, Medicare deductibles, coinsurance, and co-payments.
Is QMB the same as Medicare?
The Qualified Medicare Beneficiary (QMB) Program is one of the four Medicare Savings Programs that allows you to get help from your state to pay your Medicare premiums. This Program helps pay for Part A premiums, Part B premiums, and deductibles, coinsurance, and copayments.
What does QMB mean on Medicare?
Qualified Medicare BeneficiarySPOTLIGHT & RELEASES. The Qualified Medicare Beneficiary (QMB) program provides Medicare coverage of Part A and Part B premiums and cost sharing to low-income Medicare beneficiaries.
What does QMB without Medicare dollars mean?
This means that if you have QMB, Medicare providers should not bill you for any Medicare-covered services you receive.
What does QMB stand for?
Qualified Medicare Beneficiary (QMB)Threshold in FPL6 person household, monthlyQMB300% FPL$9,297QMB Plus100% FPL$3,099
How does Medicaid QMB work?
In addition to covering Medicare premiums for eligible QMB recipients, one of the benefits of the QMB program is having protection from improper billing. Improper billing refers to when health care providers inappropriately bill a beneficiary for deductibles, copayments or coinsurance.
Who is eligible for QMB?
You must be eligible for both Medicare and Medicaid to be eligible for QMB benefits. While Medicare’s eligibility requirements are federally mandated, each state may set its own qualifying restrictions for Medicaid.
What are other Medicare and Medicaid assistance programs?
QMB is not the only program available to dual-eligible beneficiaries. Others include:
What does QMB mean for medicaid?
What Does Medicaid QMB Cover? Medicaid QMB, which stands for Qualified Medicare Beneficiary , is a program designed specifically for individuals that qualify for both Medicare and Medicaid coverage and that are financially unstable.
What is qualified Medicare Beneficiary?
The Qualified Medicare Beneficiary program works to help cover Medicare Part A and Part B premiums, as well as the costs of coinsurance, copayments, and deductibles. All of these costs can add up quickly, especially if you require a variety of different medical services. This program is able to provide full payment of both ...
What is the difference between Medicare and Medicaid?
Original Medicare is available to individuals 65 years of age or older and individuals with certain disabilities. Medicaid insurance caters to individuals with low income and provides an affordable, government-funded healthcare option for this demographic. The QMB program has specific income requirements that must be met, ...
How many people were in the QMB in 2016?
The amounts of the QMB requirements and the poverty line generally coincide, but it is good to be aware of both. In 2016, there were approximately 7.5 million individuals that are a part of the QMB program. In fact, nearly one out of every eight Medicare recipients was a member of this program.
What is the income limit for 2019?
In 2019, the monthly income limits for individuals is $1,060 and the monthly income limit for a married couple is $1,430. There is also a limit on resources, which is set at $7,730 for individuals and $11,600 for married couples. Additionally, you must also be at or below the annual federal poverty level. The amounts of the QMB requirements and the ...
Is Medigap covered by QMB?
It is important to note that if you are currently using a Medigap plan, the premiums associated with it are not covered by the QMB program. In addition, you should also be aware that states can impose laws specific to Medicaid, Medicare, and QMB programs.
Do you have to accept Medicare and QMB?
They must accept Medicare and QMB payment for their services and recognize this payment as being the full amount of the cost of service . Improper billing protections prevent individuals using the QMB program from being responsible for any cost-sharing expenses, no matter their origin.
What is QMB for Medicare?
For those that qualify, the QMB is a valuable costs savings program for Medicare participants. It holds a potential to save significant amounts and particularly for those that use a moderate to heavy amount of services.
How much does QMB pay for Medicare?
It can pay deductibles that can total more than $1,400 per year for Part A and more than $190 for Part B. The QMB can also pay copays that apply to services used by participants. The overall amount of these payments depends on upon the services used.
What is the deductible for qualified Medicare?
The annual Medicare cycle includes a deductible which was approximately $1,408.00 in 2020. Coinsurance and copays can build into the thousands very easily given even a short hospital stay and outpatient follow-up.
What is QMB program?
The QMB Program is the Qualified Medicare Beneficiary program; Medicaid pays premiums for Part A and for Part B. It pays deductibles, coinsurance, and copays for Part B. The program accepts applicants with incomes as high as 100 percent of the federal poverty guideline. The QDWI Program is the qualified disabled and working individuals program;
What is a QMB?
The QMB is a Medicare Savings Program for low-income individuals and families that can save a lot of money. It is one of four Medicare Savings Programs.
What is QMB eligibility?
Eligibility for QMB. The keys are participation in Medicare Part A and income in the range of the federal poverty guideline. Applicants must be Medicare beneficiaries. The income must be in the range of the federal poverty guideline as adjusted by the review standards.
What percentage of Medicare Part B is covered by QMB?
In Medicare Part B, there is a common relationship of 80 percent coverage by Medicare and 20 percent by the client. The QMB program can pay part of the prescription drug costs for participants in a Medicare Part D: Prescription Drugs plan.
What is QMB program?
Since the QMB program aims to help individuals with low income, it places limits on the monthly income and financial resources available to you. If you exceed these limits, you may not be eligible for the program. Generally, participation is limited to individuals who meet the federal poverty level.
What is QMB insurance?
The QMB program is just one way to get help paying your premiums, deductibles, and other costs. You must fall below income and asset limits to participate in the QMB program. If you think you make or own too much, try applying anyway. Many assets and income sources aren’t included when calculating your eligibility.
How to enroll in QMB?
To enroll in the QMB program, you first need to be enrolled in Medicare Part A. The next step is to review your income and assets to see if you fall below the limits set by Medicare. But remember there are exceptions to those limits, and you’re encouraged to apply even if your income or assets exceed them.
How long does it take to get a QMB denial?
Once you submit your application, you should receive a confirmation or denial within about 45 days. If you’re denied, you can request an appeal. Enrollment in any of the MSPs must be renewed each year. Even when your QMB is active, you may at times be wrongfully billed for items or services that it covers.
What is the poverty level in 2021?
For 2021, the federal poverty level is $12,880 per year for individuals in Washington, D.C., and 48 states. Limits are higher in Alaska ($16,090) and Hawaii ($14,820). Specific financial requirements for the QMB for individuals are: a monthly income limit of $1,094. an asset limit of $7,970.
Does Medicare cover out of pocket costs?
The takeaway. Medicare is meant to provide affordable healthcare coverage for older adults and other individuals in need. Even so, out-of-pocket costs can add up . A number of programs can help you pay for your share of Medicare costs.
Do you have to be a resident to qualify for QMB?
You must be a resident of the state in which you’re applying for the QMB program, and you must already be enrolled in Medicare Part A. Assets that aren’t counted when you apply for the QMB program include: your primary home.
What is QMB in Medicare?
Qualified Medicare Beneficiary (QMB) Program. If you’re a Medicare beneficiary, you know that health care costs can quickly add up. These costs are especially noticeable when you’re on a fixed income. If your monthly income and total assets are under the limit, you might be eligible for a Qualified Medicare Beneficiary program, or QMB.
What is QMB insurance?
The QMB program pays: The Part A monthly premium (if applicable) The Part B monthly premium and annual deductible. Coinsurance and deductibles for health care services through Parts A and B. If you’re in a QMB program, you’re also automatically eligible for the Extra Help program, which helps pay for prescription drugs.
What is a qualified Medicare beneficiary?
The Qualified Medicare Beneficiary program is a type of Medicare Savings Program (MSP). The QMB program allows beneficiaries to receive financial help from their state of residence with the costs of Medicare premiums and more. A Qualified Medicare Beneficiary gets government help to cover health care costs like deductibles, premiums, and copays.
How much money do you need to qualify for QMB?
To be eligible for a QMB program, you must qualify for Part A. Your monthly income must be at or below $1,084 as an individual and $1,457 as a married couple. Your resources (money in checking and/or savings accounts, stocks, and bonds) must not total more than $7,860 as an individual or $11,800 as a married couple.
Can QMB members pay for coinsurance?
Providers can’t bill QMB members for their deductibles , coinsurance, and copayments because the state Medicaid programs cover these costs. There are instances in which states may limit the amount they pay health care providers for Medicare cost-sharing. Even if a state limits the amount they’ll pay a provider, QMB members still don’t have to pay Medicare providers for their health care costs and it’s against the law for a provider to ask them to pay.
Does Medicare Advantage cover dual eligibility?
A Medicare Advantage Special Needs Plan for dual-eligible individuals could be a fantastic option. Generally, there is a premium for the plan, but the Medicaid program will pay that premium. Many people choose this extra coverage because it provides routine dental and vision care, and some come with a gym membership.
Is Medigap coverage necessary for QMB?
Medigap coverage isn’t necessary for anyone on the QMB program. This program helps you avoid the need for a Medigap plan by assisting in coverage for copays, premiums, and deductibles. Those that don’t qualify for the QMB program may find that a Medigap plan helps make their health care costs much more predictable.
What is the income limit for Medicaid in 2021?
In most cases, as of 2021, the individual income limit for institutional Medicaid (nursing home Medicaid) and Home and Community Based Services (HCBS) via a Medicaid Waiver is $2,382 / month. The asset limit is generally $2,000 for a single applicant.
What is Medicare and Medicaid?
Differentiating Medicare and Medicaid. Persons who are eligible for both Medicare and Medicaid are called “dual eligibles”, or sometimes, Medicare-Medicaid enrollees. Since it can be easy to confuse the two terms, Medicare and Medicaid, it is important to differentiate between them. While Medicare is a federal health insurance program ...
How much does Medicare Part B cost?
For Medicare Part B (medical insurance), enrollees pay a monthly premium of $148.50 in addition to an annual deductible of $203. In order to enroll in a Medicare Advantage (MA) plan, one must be enrolled in Medicare Parts A and B. The monthly premium varies by plan, but is approximately $33 / month.
What is dual eligible?
Definition: Dual Eligible. To be considered dually eligible, persons must be enrolled in Medicare Part A, which is hospital insurance, and / or Medicare Part B, which is medical insurance. As an alternative to Original Medicare (Part A and Part B), persons may opt for Medicare Part C, which is also known as Medicare Advantage.
How old do you have to be to qualify for medicare?
Citizens or legal residents residing in the U.S. for a minimum of 5 years immediately preceding application for Medicare. Applicants must also be at least 65 years old. For persons who are disabled or have been diagnosed with end-stage renal disease or Lou Gehrig’s disease (amyotrophic lateral sclerosis), there is no age requirement. Eligibility for Medicare is not income based. Therefore, there are no income and asset limits.
How to apply for medicaid?
How to Apply. To apply for Medicare, contact your local Social Security Administration (SSA) office. To apply for Medicaid, contact your state’s Medicaid agency. Learn about the long-term care Medicaid application process. Prior to applying, one may wish to take a non-binding Medicaid eligibility test.
Does Medicare cover out-of-pocket expenses?
Persons who are enrolled in both Medicaid and Medicare may receive greater healthcare coverage and have lower out-of-pocket costs. For Medicare covered expenses, such as medical and hospitalization, Medicare is always the first payer (primary payer). If Medicare does not cover the full cost, Medicaid (the secondary payer) will cover the remaining cost, given they are Medicaid covered expenses. Medicaid does cover some expenses that Medicare does not, such as personal care assistance in the home and community and long-term skilled nursing home care (Medicare limits nursing home care to 100 days). The one exception, as mentioned above, is that some Medicare Advantage plans cover the cost of some long term care services and supports. Medicaid, via Medicare Savings Programs, also helps to cover the costs of Medicare premiums, deductibles, and co-payments.
