Remark Code: N522 Duplicate of a claim processed, or to be processed, as a crossover claim Common Reasons for Denial Duplicate claim has already been submitted and processed
Full Answer
What does the remark code N522 mean?
Remark Code: N522: Duplicate of a claim processed, or to be processed, as a crossover claim . Common Reasons for Denial. Duplicate claim has already been submitted and processed; Next Step. A redetermination request may be submitted with all relevant supporting documentation.
What is the EOB code for co A1 5 m2?
NULL CO A1, 5 M2 Data current as of 4/30/2016 EOB Code Description Rejection Code Group Code Reason Code Remark Code 852 Denied. Complex fees not payable in conjunction with single examiner examinations.
What is a remittance advice remark code?
Remittance Advice Remark Codes (RARCs) are used to provide additional explanation for an adjustment already described by a Claim Adjustment Reason Code (CARC) or to convey information about remittance processing. Each RARC identifies a specific message as shown in the Remittance Advice Remark Code List.
What is the remark code for a duplicate claim?
Remark Code: N522 Duplicate of a claim processed, or to be processed, as a crossover claim Common Reasons for Denial Duplicate claim has already been submitted and processed
What is remark code N522?
Duplicate of a claim processedRemark Code: N522. Duplicate of a claim processed, or to be processed, as a crossover claim.
What is a remark code for insurance?
Remittance Advice Remark Codes (RARCs) may be used by plans and issuers to communicate information about claims to providers and facilities, subject to state law.
What are the denial codes?
1 – Denial Code CO 11 – Diagnosis Inconsistent with Procedure. ... 2 – Denial Code CO 27 – Expenses Incurred After the Patient's Coverage was Terminated. ... 3 – Denial Code CO 22 – Coordination of Benefits. ... 4 – Denial Code CO 29 – The Time Limit for Filing Already Expired. ... 5 – Denial Code CO 167 – Diagnosis is Not Covered.
What does N706 remark mean?
N706. 4D. DENIED - DOCUMENTATION DOES NOT JUSTIFY PROC/MODIFIER BILLED.
What is a remark code from an Explanation of Benefits document?
7 Remark Code is a note from the insurance plan that explains more about the costs, charges, and paid amounts for your visit. After you visit your provider, you may receive an Explanations of Benefits (EOB) from your insurer.
How do you read an EOB for dummies?
1:342:35How to Read Your Medical EOB - YouTubeYouTubeStart of suggested clipEnd of suggested clipThe amount you pay for the service this is the amount that you will be billed. Remember the EOB isMoreThe amount you pay for the service this is the amount that you will be billed. Remember the EOB is not a bill it just shows you how the costs are distributed. If you have any questions by your EOB.
What are the 5 denials?
Top 5 List of Denials In Medical Billing You Can Avoid#1. Missing Information.#2. Service Not Covered By Payer.#3. Duplicate Claim or Service.#4. Service Already Adjudicated.#5. Limit For Filing Has Expired.
How do Medicare denials work?
If Your Medicare Carrier Denies a Claim...Examine the Explanation of Benefits (EOB) from the carrier, which should include the reason for a claims denial. ... Have a standardized letter handy asking the insurance carrier to reconsider your claim. ... Consider invoking your right to an appeal an adverse claims decision.
What are reason codes in medical billing?
Reason codes appear on an explanation of benefits (EOB) to communicate why a claim has been adjusted. If there is no adjustment to a claim/line, then there is no adjustment reason code.
What is remark code N174?
N174 This is not a covered service/procedure/ equipment/bed, however patient liability is limited to amounts shown in the adjustments under group "PR".
What is remark code N130?
This service/equipment/drug is not covered under the patient's current benefit plan. Remark Code: N130.
Next Step
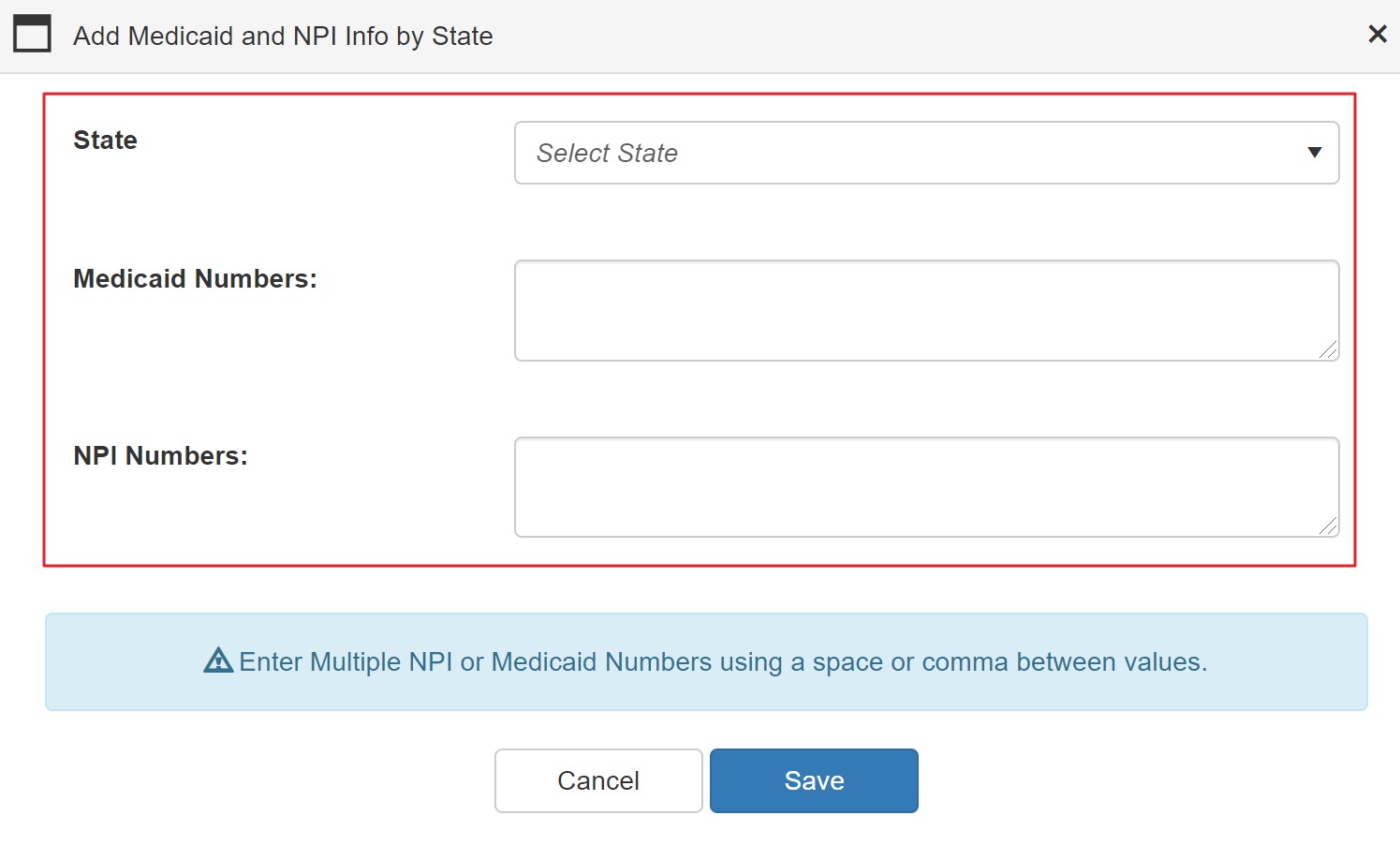
A redetermination request may be submitted with all relevant supporting documentation. Review applicable Local Coverage Determination (LCD), LCD Policy Article, and documentation prior to submitting request. Noridian encourages redeterminations be submitted using the Noridian Medicare Portal
How to Avoid Future Denials
Call Noridian Interactive Voice Response (IVR) System to receive finalized claim processing information. IVR will skip duplicate denial and provide original claim status
What is crossover claim?
Duplicate of a claim processed, or to be processed, as a crossover claim.
Is a patient entitled to benefits for institutional services?
Patient is entitled to benefits for Institutional Services.
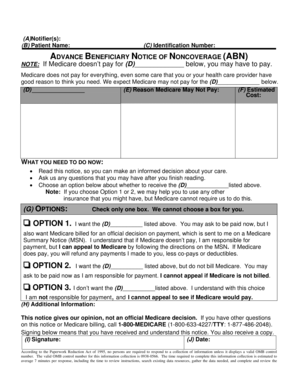
Why is payment denied for less extensive service?
Payment has been (denied for the/made only for a less extensive) service/item because the information furnished does not substantiate the need for the (more extensive) service/item. If you have collected any amount from the patient, you must refund that amount to the patient within 30 days of receiving this notice.
What is the second type of RARC?
The second type of RARC is informational; these RARCs are all prefaced with Alert: and are often referred to as Alerts. Alerts are used to convey information about remittance processing and are never related to a specific adjustment or CARC. Maintenance Request Form. (link is external) 3/1/2021.
When did Obama sequester Medicare?
As required by law, President Obama issued a sequestration order on March 1, 2013, canceling budgetary resources across the Federal Government. As a result, Medicare Fee-For-Service claims, with dates of service or dates of discharge on or after April 1, 2013, incur a two percent reduction in Medicare payment.
What is a CARC code?
New Claim Adjustment Reason Code (CARC) to Identify a Reduction in Payment Due to Sequestration
Does CMS change MAC statement of work?
CMS does not construe this as a change to the MAC statement of Work. The contractor is not obliged to incur costs in excess of the amounts allotted in your contract unless and until specifically authorized by the Contracting Officer.
Is Medicare cut higher than 2 percent?
The Medicare cut will never be higher than 2 percent. • Importantly, the Medicare cuts each year are not cumulative. So, the 2 percent cut this year will not be followed by another 2 percent cut next year, and so forth, producing a cumulative double-digit cut at the end of the sequestration period.