The AASM continues to recommend scoring hypopneas in adults when there is a ≥ 3% oxygen desaturation from pre-event baseline and/or the event is associated with an arousal. However, it is acceptable for accredited sleep centers to score hypopneas in adults when there is a ≥ 4% oxygen desaturation from pre-event baseline.
What is the definitive reference for sleep scoring?
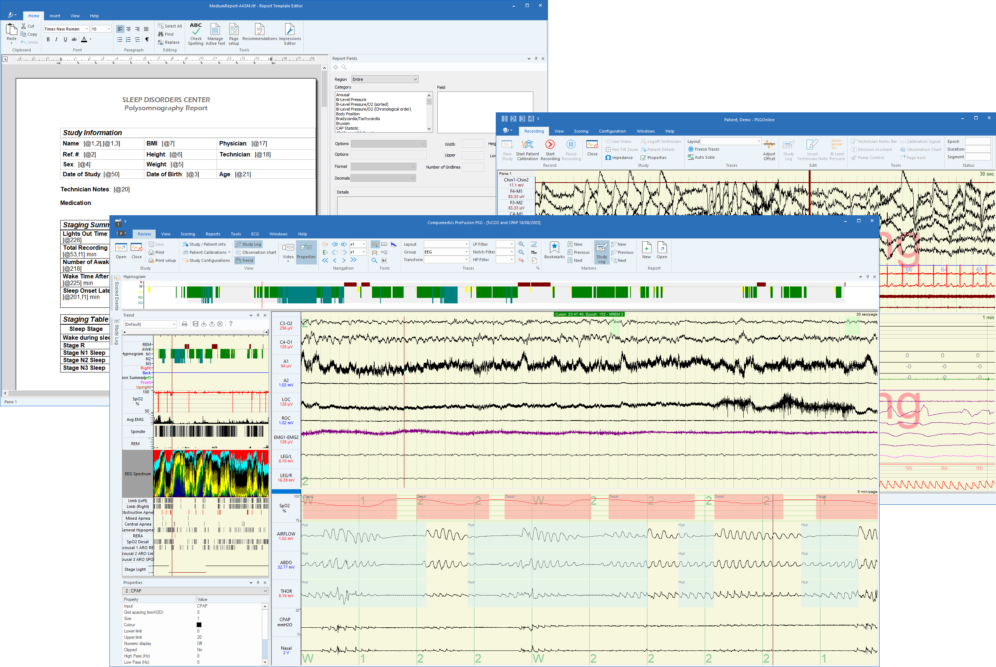
The Definitive Sleep Scoring Resource. The AASM Manual for the Scoring of Sleep and Associated Events: Rules, Terminology and Technical Specifications is the definitive reference for the evaluation of polysomnography (PSG) and a home sleep apnea test (HSAT).
Who can interpret a sleep study for Medicare patients?
Only a sleep boarded or board-eligible physician can interpret sleep studies for Medicare patients. The physician must meet one of the following requirements: Current subspecialty certification in Sleep Medicine – By a member board of the American Board of Medical Specialties (ABMS); or
Do accredited sleep centers need to score hypopneas?
In August members were notified that the AASM has suspended indefinitely the requirement for accredited sleep centers to score hypopneas in adult patients according to the 3 percent oxygen desaturation criterion in the new AASM scoring manual.
What is the Medicare Code for a sleep apnea test?
For home sleep apnea testing, Medicare uses code G0399 (for a type III device) or G0398 (for a type II device). Medicare uses code 95810 for in-center diagnostic polysomnography (PSG) and 95811 for a 50/50 study or full night titration study (learn more about sleep study types and codes, including pediatric sleep codes here.
How do you score a sleep study?
You score the number of the patient's arousals and awakenings in the study and report the arousal index (frequency per hour of sleep and the total number). The higher this index, the more tired the patient will most likely feel depending on their sleep disruption tolerance level.
How is sleep apnea test scored?
An AHI of 30 or higher is consistent with severe sleep apnea. Additional testing is usually required to determine the accurate level of severity and to narrow down treatment options.
How many sleep studies will Medicare pay for in a year?
four levelsAll four levels of sleep studies (Type I, Type II, Type III and Type IV) are covered by Medicare. But a Type I study, which requires you to sleep overnight in a sleep lab facility under the supervision of a sleep specialist, must be specifically ordered by a doctor before Medicare will cover it.
What is the cutoff for sleep apnea?
Most sleep centers use a cutoff of 5-10 episodes per hour. The severity of OSA is arbitrarily defined and differs widely between centers. Recommendations for cutoff levels on AHI include 5-15 episodes per hour for mild, 15-30 episodes per hour for moderate, and more than 30 episodes per hour for severe.
What is a good CPAP score?
Normal: Fewer than 5 breathing events per hour of sleep. Mild sleep apnea: 5 to 14.9 breathing events per hour of sleep. Moderate sleep apnea: 15 to 29.9 breathing events per hour of sleep. Severe sleep apnea: 30 or more breathing events per hour of sleep.
What is a good AHI score?
An AHI less than 5 is considered normal, and some patients with severe sleep apnea may be told by their doctor that they can accept even higher numbers so long as they're feeling more rested each morning, experiencing fewer symptoms and their AHI is progressively decreasing.
Will Medicare pay for a second sleep study?
Medicare will approve additional sleep studies as long as there is a face-to-face evaluation with the patient.
How often does Medicare require a sleep study for CPAP?
Medicare covers CPAP for the treatment of OSA if the beneficiary has an AHI or RDI ≥ 15 events/hour.
How often should a sleep study be repeated?
While there is no set time to repeat a sleep apnea test, many doctors recommend an updated test every 5 years. Returning sleep apnea symptoms, changes in lifestyle, or changes in CPAP therapy are good indicators that a new sleep study test is required.
How many apnea events per hour is normal?
That's because it's considered normal for everyone to have up to four apneas an hour. It's also common if your AHIs vary from night to night. For some CPAP users, even higher AHIs are acceptable, depending on the severity of your sleep apnea.
What is the highest AHI score?
The Apnoea–Hypopnea Index (AHI) is used to classify the severity of the illness: mild AHI 5 to <15; moderate 15 to <30; and severe 30 or more [5]. It is well known that patients with severe OSA have higher morbidity and mortality rates compared to those with mild or moderate levels [6,7].
How many events per hour is considered sleep apnea?
Obstructive sleep apnea is classified by severity: Severe obstructive sleep apnea means that your AHI is greater than 30 (more than 30 episodes per hour) Moderate obstructive sleep apnea means that your AHI is between 15 and 30. Mild obstructive sleep apnea means that your AHI is between 5 and 15.
Sleep Test Scoring and Medicare
Yes.In 2008, the Centers for Medicare and Medicaid Services (CMS) updated the National Coverage Determination for CPAP to include home sleep apnea...
Sleep Study CPT codes list 95806, 95810, 95811, 95807
Medicare will cover two types of home sleep testing devices: 1. Type III home sleep test. This is a four-channel device which measures (1) airflow,...
LCD - Outpatient Sleep Studies (L35050) - CMS
1. Patient must be referred by their attending physician (not a dentist). 2. Sleep must be recorded and staged. 3. Sleep study may be ordered to di...
AASM: 4% Desaturation Criterion is Acceptable for Scoring Hypopneas
From a DME (CPAP) and Part B perspective for ultimate coverage of the PAP device for treatment of sleep apnea, Medicare must see elaboration and ex...
Does Medicare Cover In-Home Sleep Apnea Testing?
Currently, there is no coverage for PAP nap (afternoon nap or short daytime titration studies) sleep studies, regardless of billing codes or modifi...
What Type of Home Sleep Apnea Test Does Medicare Cover?
It depends on the circumstances requiring the new study. There is no lifetime limit for sleep studies. Generally, an initial diagnostic PSG and a f...
What Are The Criteria For Medicare to Cover An In-Home Or In-Center Sleep Study?
Once the sleep study is completed and the data is scored, the report is sent to a sleep specialist for review and interpretation. Only a sleep boar...
Is Snoring Alone Sufficient For Ordering A Sleep Study For A Medicare Patient?
The technician must be credentialed OR certified with one or more of the following: 1. American Academy of Sleep Medicine (AASM) 2. American Board...
Does Medicare Cover Pap naps?
Medicare will pay 80% of the Medicare-approved amount for an in-home (HST) or in-center sleep study after you’ve met your Part B deductible (learn...
How Often Will Medicare Cover A Sleep Study?
For home sleep apnea testing, Medicare uses code G0399 (for a type III device) or G0398 (for a type II device). Medicare uses code 95810 for in-cen...
Who Can Interpret A Sleep Study For A Medicare Patient?
What Type of Certification Must The Sleep Technician Have to Perform Studies For Medicare Patients
How Much Will Medicare Pay For A Sleep Study?
What Codes Are Used to Bill Medicare For A Sleep Study?
How much does Medicare pay for sleep studies?
Medicare will pay 80% of the Medicare-approved amount for an in-home (HST) or in-center sleep study after you’ve met your Part B deductible (learn about this and other insurance terms here ). If you have a secondary insurance, they may pick up the remaining 20% (read our post about how much sleep studies cost here ).
Who can interpret a sleep study for Medicare?
Only a sleep boarded or board-eligible physician can interpret sleep studies for Medicare patients.
What is HST in sleep?
HST is a type of diagnostic polysomnography which is self-administered by the patient in his/her home. It is used to diagnose sleep apnea by recording several channels of information: respiratory effort, pulse, oxygen saturation, nasal flow and snoring.
What type of certification do sleep techs need?
What type of certification must the sleep technician have to perform studies for Medicare patients: The technician must be credentialed OR certified with one or more of the following: American Academy of Sleep Medicine (AASM) American Board of Sleep Medicine (ABSM)-Registered Sleep Technologist (RST)
How long does a sleep study last?
There is no lifetime limit for sleep studies. Generally, an initial diagnostic PSG and a follow-up titration to evaluate effectiveness should be all that is needed for several months unless their is an extraordinary change in the patient’s well being.
Is sleep study covered by dental insurance?
Patient must be referred by their attending physician (not a dentist). Sleep must be recorded and staged. Other disorders during sleep (parasomnias) including dental/medical/psychiatric disorders and sleep behavior disorders. Sleep studies are not covered for chronic insomnia.
Does CPAP include HST?
Yes. In 2008, the Centers for Medicare and Medicaid Services (CMS) updated the National Coverage Determination for CPAP to include home sleep apnea testing (HST) as a means to qualify patients with obstructive sleep apnea (learn more about OSA here) for CPAP therapy (learn more about CPAP here ). HST is a type of diagnostic polysomnography which is ...
note
To find out how much your test, item, or service will cost, talk to your doctor or health care provider. The specific amount you’ll owe may depend on several things, like:
note
Your doctor or other health care provider may recommend you get services more often than Medicare covers. Or, they may recommend services that Medicare doesn’t cover. If this happens, you may have to pay some or all of the costs.
Document Information
CPT codes, descriptions and other data only are copyright 2020 American Medical Association. All Rights Reserved. Applicable FARS/HHSARS apply.
CMS National Coverage Policy
This LCD supplements but does not replace, modify or supersede existing Medicare applicable National Coverage Determinations (NCDs) or payment policy rules and regulations for outpatient sleep services. Federal statute and subsequent Medicare regulations regarding provision and payment for medical services are lengthy.
Coverage Guidance
Compliance with the provisions in this LCD may be monitored and addressed through post payment data analysis and subsequent medical review audits. History/Background and/or General Information Sleep complaints and disorders are widespread.
General Information
Medicare is a single-payer, national insurance program administered by the U.S. federal government for people age 65 or older, people under age 65 with certain disabilities, and people of all ages with end-stage renal disease.
National Coverage Determinations
Continuous Positive Airway Pressure (CPAP) Therapy for Obstructive Sleep Apnea (OSA) (240.4) Effective Date: March 13, 2008
DME – Local Coverage Determinations
The following chart lists all of the LCDs and Local Coverage Articles for Positive Airway Pressure (PAP) devices and Oral Appliances for the treatment of OSA.
DME MAC– Dear Physician Letters
DME MACs have developed Dear Physician Letters, to highlight requirements for sleep study scoring.
What are the goals of the respiratory scoring task force?
The goals of the task force were: (1) to clarify and simplify the respiratory scoring rules, (2) to review evidence for new monitoring technologies relevant to the scoring rules, and (3) to strive for greater concordance between adult and pediatric rules.
When was the AASM scoring manual published?
In 2007 the American Academy of Sleep Medicine (AASM) published rules for scoring respiratory events in the AASM Manual for the Scoring of Sleep and Associated Events, 1sted.1(hereafter referred to as the 2007 scoring manual). Widespread use of the rules has resulted in questions about rule interpretation and application.
What is the minimum duration of hypopnea?
This is very similar to the current recommendation of the task force for the hypopnea definition for adults except that the minimum duration is 2 breaths.
Can apnea be scored?
An apnea cannot be scored using the apnea rule in the 2007 scoring manual as 24 seconds (the duration of the ≥ 90% drop in oronasal flow) is not 90% of the event duration. A hypopnea cannot be scored based on the drop in nasal pressure, as there is no associated desaturation or arousal.
How to contact AASM for sleep facilities?
To request participation in the AASM Expedited Accreditation Program at the reduced fee, or for more information, sleep facilities can contact the AASM Accreditation Department at 630-737-9700 or [email protected].
How long does it take for an AASM to approve a facility?
Depending on a facility’s responsiveness and the thoroughness of its application, the AASM may be able to issue an accreditation decision 2 to 4 weeks after application submission.
Can a sleep facility be accredited?
To demonstrate that a sleep center is certified by the AASM, a sleep facility may apply for and achieve AASM Sleep Facility Accreditation. Facilities seeking sleep center accreditation to meet this medical policy article requirement can take advantage of the AASM Expedited Accreditation program, which was originally created for sleep facilities ...
The Definitive Sleep Scoring Resource
The AASM Manual for the Scoring of Sleep and Associated Events: Rules, Terminology and Technical Specifications is the definitive reference for the evaluation of polysomnography (PSG) and a home sleep apnea test (HSAT).
The Scoring Manual Subscription
The AASM Scoring Manual is an online and app-based resource offering you digital access from your desktop, tablet and mobile device. An annual subscription ensures that you always have immediate access to the current version of the manual, and it enables you to remain compliant with AASM accreditation standards.
Questions?
Along with your online subscription, subscribers now have access to a list of frequently asked questions about the AASM Scoring Manual with responses.
Summary of Updates
The following are summaries of the revisions made for each major update of the AASM Scoring Manual including the dates when these new versions were released.