What is a Tier 2 copay?
What is a Tier 2 prescription drug?
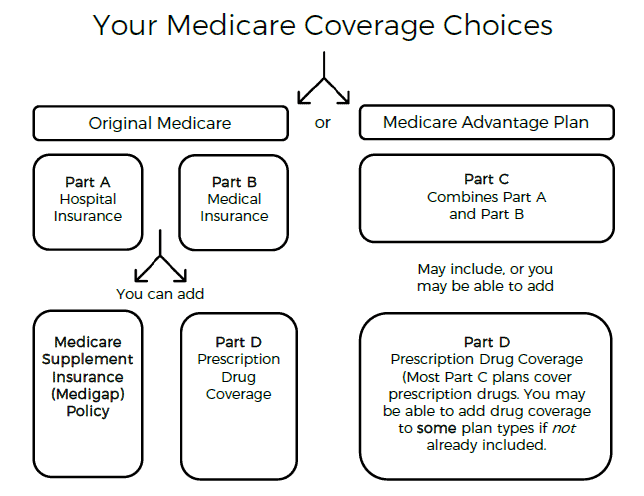
What are the levels of Medicare coverage?
What do Medicare tiers mean?
How do you determine a drug tier?
What is a Tier 3 medication?
What is the difference between Medicare Part C and Part D?
What are Medicare Parts A & B?
Is Medicare Part A free at age 65?
How many tiers are there in Medicare Part D?
What is the most popular Medicare Part D plan?
| Rank | Medicare Part D provider | Medicare star rating for Part D plans |
|---|---|---|
| 1 | Kaiser Permanente | 4.9 |
| 2 | UnitedHealthcare (AARP) | 3.9 |
| 3 | BlueCross BlueShield (Anthem) | 3.9 |
| 4 | Humana | 3.8 |
Do I have Medicare Part D?
What are the tiers of Medicare?
Here's an example of a Medicare drug plan's tiers (your plan’s tiers may be different): Tier 1—lowest. copayment. An amount you may be required to pay as your share of the cost for a medical service or supply, like a doctor's visit, hospital outpatient visit, or prescription drug.
What does Medicare Part D cover?
All plans must cover a wide range of prescription drugs that people with Medicare take, including most drugs in certain protected classes,” like drugs to treat cancer or HIV/AIDS. A plan’s list of covered drugs is called a “formulary,” and each plan has its own formulary.
What is the formulary for Medicare?
Most Medicare drug plans (Medicare drug plans and Medicare Advantage Plans with prescription drug coverage) have their own list of what drugs are covered, called a formulary. Plans include both brand-name prescription drugs and generic drug coverage. The formulary includes at least 2 drugs in the most commonly prescribed categories and classes.
How many drugs does Medicare cover?
All Medicare drug plans generally must cover at least 2 drugs per drug category, but plans can choose which drugs covered by Part D they will offer. The formulary might not include your specific drug. However, in most cases, a similar drug should be available.
Does Medicare save you money?
Also, using generic drugs instead of brand-name drugs may save you money.
When will Medicare start paying for insulin?
Starting January 1, 2021, if you take insulin, you may be able to get Medicare drug coverage that offers savings on your insulin. You could pay no more than $35 for a 30-day supply. Find a plan that offers this savings on insulin in your state. You can join during Open Enrollment (October 15 – December 7, 2020).
What is tiering exception?
A tiering exception is a drug plan's decision to charge a lower amount for a drug that's on its non-preferred drug tier. You or your prescriber must request an exception, and your doctor or other prescriber must provide a supporting statement explaining the medical reason for the exception. .
Is Medicare a secondary payer?
Medicare is the secondary payer if the recipient is: Over the age of 65 and covered by an employment-related group health plan as a current employee or the spouse of a current employee in an organization with more than 20 employees.
What is secondary payer?
A secondary payer assumes coverage of whatever amount remains after the primary payer has satisfied its portion of the benefit, up to any limit established by the policies of the secondary payer coverage terms.
Does Medicare pay conditional payments?
In any situation where a primary payer does not pay the portion of the claim associated with that coverage, Medicare may make a conditional payment to cover the portion of a claim owed by the primary payer. Medicare recipients may be responsible for making sure their primary payer reimburses Medicare for that payment.
Does Medicare cover tests?
Medicare coverage for many tests, items, and services depends on where you live . This list includes tests, items, and services (covered and non-covered) if coverage is the same no matter where you live.
What does Medicare Part B cover?
Part B also covers durable medical equipment, home health care, and some preventive services.
What are the tiers of Medicare Part D?
The Medicare Part D tiers refer to how drugs are organized in a formulary. They include both generic and brand name drugs, covered for different prices. Most commonly there are tiers 1-5, with 1 covering the lowest-cost drugs and 5 covering the most expensive specialty medications.
What are the tiers of a drug?
They include both generic and brand name drugs, covered for different prices. Most commonly there are tiers 1-5, with 1 covering the lowest-cost drugs and 5 covering the most expensive specialty medications.
Does Medicare Part D have a deductible?
Medicare Part D tiers 1 and 2 are often set up to exempt you from paying a deductible, whereas with drugs in the higher tiers you may have to pay the full drug cost until you meet the deductible, then pay a copay/coinsurance.
What is preferred drug?
Preferred drugs means a certain set of types of medications that have been approved by the insurance company to be in this low-cost grouping. Generic refers to non-name brand versions of each type of drug.
What is tier 1 drug?
What it means. Cost. Tier 1. Preferred generic. These are commonly prescribed generic drugs. For most plans, you’ll pay around $1 to $3 for drugs in this tier. Tier 2. Generic. These are also generic drugs, but they cost a little more than drugs in Tier 1.
What is a drug tier?
Drug tiers are how we divide prescription drugs into different levels of cost.
How much does a preferred generic cost?
Preferred generic. These are commonly prescribed generic drugs. For most plans, you’ll pay around $1 to $3 for drugs in this tier. Tier 2. Generic. These are also generic drugs, but they cost a little more than drugs in Tier 1. For most plans, you’ll pay around $7 to $11 for drugs in this tier. Tier 3. Preferred brand.
What is preferred brand?
Preferred brand. These are brand name drugs that don’t have a generic equivalent. They’re the lowest-cost brand name drugs on the drug list. For most plans, you’ll pay around $38 to $42 for drugs in this tier. Tier 4. Nonpreferred drug. These are higher-priced brand name and generic drugs not in a preferred tier.
What is specialty drug?
Specialty drugs are used to treat complex conditions like cancer and multiple sclerosis. They can be generic or brand name. For most plans, you’ll pay 25% to 33% of the retail cost for drugs in this tier. Tier 6.
What is a Part D specialty tier?
Under the final rule, Part D plans may establish a second specialty tier, splitting specialty drugs between a non-preferred specialty tier and a preferred specialty tier, with the preferred tier carrying lower cost-sharing obligations than the non-preferred tier. By allowing plans to apply differential co-insurance obligations to specialty drugs, this dual specialty tier model is designed to give plans flexibility to incentivize beneficiaries to select lower-cost specialty drugs.
Do specialty tiers have tiering exceptions?
Presently, specialty tier medications are not required to have a tiering exception from the specialty tier down to a “lower” non -specialty tier. Plans managing their formularies (every Part D plan) must maintain a benefit design actuarially equivalent to the Defined Standard and allowing a non -specialty tier exception “would likely increase costs elsewhere such as increased cost-sharing on generic drug tiers or increases in premiums.” In the final rule, CMS formally clarified that Part D sponsors may design their exception processes so that Part D drugs on the specialty tier (s) are not eligible for a tiering exception to non- specialty tiers to maintain actuarial equivalence.
When is the final rule for the CY 2022?
With the bids due by June 2021 and the expiration of the 60-day regulatory delay period, the final rule is expected to remain unchanged for CY 2022.
Ways to Save on Eliquis
Here are some ways that may lower the cost of your Eliquis prescription.
Are there any restrictions on coverage?
Most Medicare prescription drug plans have quantity limits to restrict the amount of this drug that can be filled at one time.
What drug tier is Eliquis typically on?
Medicare prescription drug plans typically list Eliquis on Tier 3 of their formulary. Generally, the higher the tier, the more you have to pay for the medication. Most plans have 5 tiers.