
SNPs typically cover the following:
- Care and services from providers in the SNP network. In most SNPs, you’ll choose a primary care doctor who will coordinate your care and give you referrals to specialists when ...
- Prescription drugs. ...
- Additional items not covered by Original Medicare. ...
Who can join a Medicare SNP?
Medicare SNPs are a type of Medicare Advantage Plan (like an HMO or PPO). Medicare SNPs limit membership to people with specific diseases or characteristics. Medicare SNPs tailor their benefits, provider choices, and drug formularies to best meet the specific needs of …
Does anyone have a Medicare SNP plan?
Medicare SNPs cover the same Medicare services that all Medicare Advantage plans must cover. Medicare SNPs may also cover extra services tailored to the special groups they serve, like extra days in the hospital. Contact your plan to learn …
What is SNP Health Plan?
A Special Needs Plan (SNP) is a type of Medicare Advantage coordinated care plan. SNPs tailor the benefits, provider choices and drug formularies they offer to best serve the specific needs of beneficiaries. For example, a private health insurance company might offer …
Which Medicare plan is best?
Oct 28, 2021 · A Special Needs Plan (SNP) is a type of Medicare Advantage plan that’s available to beneficiaries with specific financial, health, or institutional needs. SNPs are regional, not available in all areas, and open to qualifying beneficiaries only. Key Takeaways There are three types of Special Needs Plans: D-SNP ( dual-eligible
What does PPO SNP mean?
Preferred Provider OrganizationYour Medicare SNP may be a Health Maintenance Organization (HMO) or a Preferred Provider Organization (PPO). Depending on your plan, you may need to see in-network providers to receive coverage, or have the option of going out of network.
What is the difference between SNP and D SNP?
Institutional SNP (I-SNP): For those who live in an institution such as a nursing home or require nursing care at home. Dual-Eligible SNP (D-SNP): For those with both Medicare and Medicaid.
What does HMO C SNP mean?
C-SNPs are SNPs that restrict enrollment to special needs individuals with specific severe or disabling chronic conditions, defined in 42 CFR 422.2.Dec 1, 2021
What is SNP model of care?
SNP Model of Care is the overall plan for SNP structure, processes, resources, and requirements. SNP MOCs must identify and describe the target population, including health and social factors, and unique characteristics of each SNP type.
Is SNP a Medicare Advantage Plan?
Medicare SNPs are a type of Medicare Advantage Plan (like an HMO or PPO). Medicare SNPs limit membership to people with specific diseases or characteristics. Medicare SNPs tailor their benefits, provider choices, and drug formularies to best meet the specific needs of the groups they serve.
What is a D-SNP look alike plan?
D-SNP “look-alike” plans (sometimes called “mirror” plans) are Medicare Advantage plans that plan sponsors have designed specifcally to attract dual eligible benefciaries.
How do SNP plans work?
When you join a Medicare SNP, you get all your Medicare hospital, medical health care services, and prescription drug coverage through that plan. Because they offer all health care services through a single plan, Medicare SNPs can help you manage your different services and providers.
Does diabetes qualify for C SNP?
Chronic Condition Special Needs (C-SNP) plans are a type of Medicare Advantage (MA) plan designed to meet the unique needs of people with one or more chronic conditions, including diabetes, end-stage renal disease (ESRD), lung conditions or heart disease.
Are SNP plans network based?
SNP networks vary in size and the populations they serve. Two types of networks include: Networks covering a specified area. For example, one network may cover an entire state, while another network covers one county.Dec 1, 2021
Does CMS require NCQA accreditation?
CMS approved NCQA for deeming of Special Needs Plans (SNPs) Model of Care (MOC) requirements. NCQA evaluates plans against a set of standards for MOCs. Organizations that meet NCQA SNP deeming module requirements are deemed for Medicare requirements for SNP MOC.
What is SNP in healthcare?
A SNP may be any type of MA CCP, including either a local or regional preferred provider organization (i.e., LPPO or RPPO) plan, a health maintenance organization (HMO) plan, or an HMO Point-of-Service (HMO-POS) ...
When did the SNP program end?
Most recently, section 206 of the Medicare Access and CHIP Reauthorization Act of 2015 (MACRA) extended the SNP program through December 31, 2018.
Why do SNPs need to provide Part D coverage?
All SNPs must provide Part D prescription drug coverage because special needs individuals must have access to prescription drugs to manage and control their special health care needs. SNPs should assume that, if no modification is contained in guidance, existing Part C and D rules apply.
What is a special needs plan?
A special needs plan (SNP) is a Medicare Advantage (MA) coordinated care plan (CCP) specifically designed to provide targeted care and limit enrollment to special needs individuals. A special needs individual could be any one of the following: An institutionalized individual, A dual eligible, or. An individual with a severe or disabling chronic ...
Do SNPs have to submit bids?
SNPs must prepare and submit bids like other MA plans, and are paid in the same manner as other MA plans based on the plan’s enrollment and risk adjustment payment methodology. All SNPs must abide by current CMS guidance on cost sharing requirements.
Do SNPs have to follow Medicare?
SNPs are expected to follow existing MA program rules, including MA regulations at 42 CFR 422, as modified by guidance, with regard to Medicare- covered services and Prescription Drug Benefit program rules. All SNPs must provide Part D prescription drug coverage because special needs individuals must have access to prescription drugs to manage and control their special health care needs. SNPs should assume that, if no modification is contained in guidance, existing Part C and D rules apply.
Did CMS accept SNP applications in 2008?
Accordingly, CMS did not accept SNP applications in 2008 for contract year (CY) 2009. The Medicare Improvements for Patients and Providers Act of 2008 (MIPPA) lifted the Medicare, Medicaid, and SCHIP Extension Act of 2007 moratorium on approving new SNPs.
What is a SNP for Medicare?
Get the right prescriptions to prevent complications. A Medicare SNP for people with both Medicare and Medicaid might use a care coordinator to help members access community resources and coordinate their different Medicare and Medicaid services. expand.
Why do Medicare SNPs use care coordinators?
Some Medicare SNPs use a care coordinator to help you stay healthy and follow your doctor's orders. A care coordinator is someone who helps make sure people get the right care and information. For example, a Medicare SNP for people with diabetes might use a care coordinator to help members do these things:
What happens if you don't have Medicare?
If you don't have both Medicare and Medicaid (or get other help from your state paying your Medicare premiums), your exact costs will vary depending on the plan you choose. In general, you'll pay the basic costs of having a Medicare Advantage plan . expand.
How long is the grace period for Medicare?
The grace period is at least one month long, but plans can choose to have a longer grace period. If you lose eligibility for the plan, you'll have a Special Enrollment Period to make another choice. This Special Enrollment Period starts when your Medicare SNP notifies you that you're no longer eligible for the plan.
Does Medicare cover SNP?
If you have Medicare and Medicaid, most of the costs of joining a Medicare SNP will be covered for you . Contact your Medicaid office for more information and to see if you qualify for Medicaid benefits.
What is a SNP in Medicare?
Each Medicare SNP is designed to offer some unique benefits designed to serve the population for whom that plan is designed. For example, a Medicare SNP for beneficiaries who have a chronic lung disorder may include: A network of providers who specialize in treating lung conditions.
What is a SNP plan?
A Medicare SNP, or Special Needs Plan, is a type of Medicare Advantage plan tailored to the needs of specific health conditions or circumstances. Learn more about what a Medicare Advantage SNP might cover, how these plans typically work and how and when you can enroll in an SNP plan. Medicare Advantage plans called Special Needs Plans (SNP) ...
What is a special needs plan?
A Special Needs Plan is a type of Medicare Advantage plan (also called Medicare Part C) that is designed specifically for someone with a particular disease or financial circumstance. The coverage offered by each SNP is built around providing more narrowly-focused care that better meets the needs of the patient.
What is Medicare Advantage?
Medicare Advantage plans offer an alternative way to receive Original Medicare benefits (Part A and Part B), and many Medicare Advantage plans offer additional benefits that aren't covered by Original Medicare. Medicare Advantage plans come in a variety of types such as HMOs and PPOs. While Original Medicare can be used all over the country, ...
What is Medicare Advantage Special Needs?
Medicare Advantage Special Needs Plans can also cater more specifically to the needs of people with: There also Special Needs Plans that can be available to people who reside in a long-term care facility such as a skilled nursing home.
What is SNP network?
SNP network providers are typically specialists who focus their care on the very type of condition, symptoms and treatment associated with your situation. The right type of care can be hard to find, and Special Needs Plans can help you find the specialized providers you need. Medicare Special Needs Plans also generally feature a list ...
Why are special needs plans beneficial?
Special Needs Plans can be particularly beneficial because of their focused coverage benefits. Care coordination. Some Special Needs Plans feature care coordination services. These plans may assign a care coordinator to each member who serves as a sort of "quarterback" for your care.
Why is Medicare SNP important?
Because Medicare SNP plans are created with special needs in mind, they generally go beyond providing the same level of coverage as Original Medicare Parts A and B, offering benefits that are specifically tailored to their enrollees’ conditions or circumstances . The targeted services that are offered are formulated to complement the regimens and requirements of the beneficiaries. This both improves treatment and minimizes frustrations and costs that may be encountered in other Medicare Advantage plans that serve a more general patient population.
What are the drawbacks of Medicare SNP?
Though Medicare SNP plans are designed to provide special services to those Medicare beneficiaries that need them, there are some drawbacks to the programs. The SNP plans frequently require their enrollees to see physicians and use providers that are part of pre-established networks, and this may preclude you from remaining with your existing physician. You also may need to get referrals to see specialists. The programs are not widely available, and those who believe they are qualified in the programs must meet specific SNP eligibility criteria. Beneficiaries may be disenrolled when their status changes and they no longer meet the criteria, and will then need to enroll in another plan. Though, if a beneficiary is disenrolled they will have a Special Enrollment Period to join another Medicare Advantage plan.
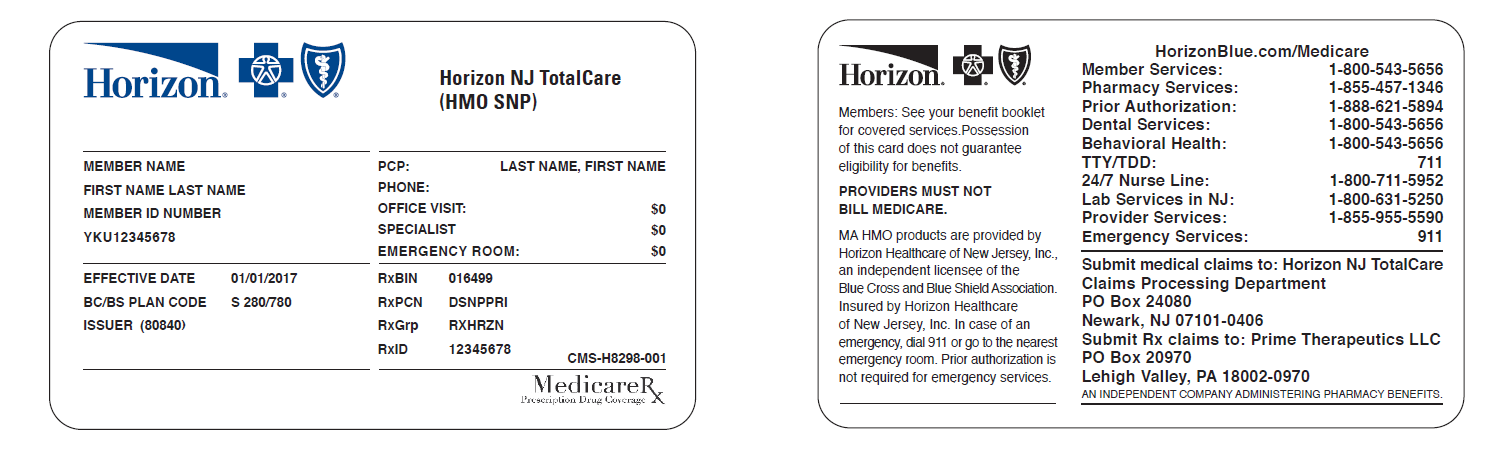
How to qualify for dual SNP?
To qualify for a Dual Eligible Special Needs Plan, you need to provide proof that you have Medicaid. This can be accomplished either by producing a letter from Medicaid or showing your Medicaid identification card. Alternatively, you can complete the enrollment form for the D-SNP and the plan administrator will verify your Medicaid status. It is important to note that if you are enrolled in a Medicare MSP (Medical Savings Plan) at the time that you apply for a Dual Eligible Special Needs Plan, you may find that the specific plan does not accept MSP beneficiaries to enroll. Most D-SNPs include a high level of dental, vision, and hearing care, as well as many other benefits.
How long do you have to live in a nursing home to qualify for SNP?
To qualify for an Institutional Special Needs Plan, you must live in long-term care served by the SNP for a minimum of 90 days. To qualify, the facility can be either a nursing home or an intermediate care facility for those with intellectual disabilities. Alternatively, you must have met your state’s guidelines for requiring a nursing home-level of care for a minimum of 90 days whether you live in a community setting such as your home or a group residence or in an institution. Those who have not yet received care for at least 90 days but who are likely to need that level of care for that period of time can also qualify.
Who is Caren Lampitoc?
Caren Lampitoc is an educator and Medicare consultant for Medicare Risk Adjustments and has over 25 years of experience working in the field of Medicine as a surgical coder, educator and consultant.
What are the requirements for SNP?
To be eligible for an SNP, you must have Medicare Parts A and B and meet the specific conditions of the SNP. Depending on the specific plan, benefits may also include coverage for routine dental, vision and hearing care; nonemergency transportation to and from medical care; fitness programs; an over-the-counter medication allowance and more.
What is a special needs plan?
A Special Needs Plan (SNP) is a type of Medicare Advantage plan that combines all the benefits of Original Medicare (Parts A and B) with prescription drug coverage (Part D), but is only available to those beneficiaries who have an additional qualifying condition. For example, those who: 1 Have a specific chronic health condition 2 Are eligible for both Medicare and Medicaid 3 Are a resident of a long-term care facility
What does an I-SNP need to document?
If an I-SNP enrollee changes residence, the I-SNP must document that it is prepared to implement a CMS-approved MOC at the enrollee’s new residence, or in another I-SNP contracted LTC setting that provides an institutional level of care.
What methodology do I-SNPs use?
In states and territories without a specific tool, I-SNPs must use the same LOC determination methodology used in the respective state or territory in which the I-SNP is authorized to enroll eligible individuals.
What is a D-SNP?
What Are D-SNPs? If you are eligible for both Medicare and Medicaid, you can enroll in a Dual Eligible Special Needs Plan (D-SNP). These plans make managing your benefits for both programs easier and allow you to more efficiently manage your health care expenses.
What does it mean to join an I-SNP?
Joining an I-SNP may make institutional care more affordable or offer supplemental benefits that specifically help institutionalized individuals.
What is special needs Medicare?
Special Needs Plans are a type of Medicare Advantage plan that focuses on a specific group of individuals who fit select criteria. Special Needs Plans offer select benefits that may not be available in other plans, therefore you must verify that you fit the selection criteria before attempting to enroll.
What is Medicare Advantage?
Medicare has several different components, one of which is the Medicare Advantage category of health coverage. Advantage plans are offered by private insurance companies that work with the Medicare agency, therefore they have more flexibility in the types of benefits they can offer.
What conditions warrant SNP?
Common conditions that warrant an SNP include cancer, diabetes, dementia, End Stage Renal Disease, and neurologic disorders. An insurance agent can help you discover whether your health status qualifies you for a C-SNP.
Can I be institutionalized for I-SNP?
If you or a person you are caring for has been institutionalized, they may qualify for an I-SNP. In order to enroll in an I-SNP, an individual must be eligible for Medicare Advantage and live in an area where such a plan is available. They must also provide proof that an independent and impartial party has determined they require an institutional ...
What Is A Special Needs Plan?
- A special needs plan (SNP) is a Medicare Advantage (MA) coordinated care plan (CCP) specifically designed to provide targeted care and limit enrollment to special needs individuals. A special needs individual could be any one of the following: 1. An institutionalized individual, 2. A dual eligible, or 3. An individual with a severe or disabling chr...
Statutory and Regulatory History
- The Medicare Modernization Act of 2003 (MMA) established an MA CCP specifically designed to provide targeted care to individuals with special needs. In the MMA, Congress identified “special needs individuals” as: 1) institutionalized individuals; 2) dual eligibles; and/or 3) individuals with severe or disabling chronic conditions, as specified by CMS. MA CCPs established to provide se…
Requirements and Payment Procedures
- SNPs are expected to follow existing MA program rules, including MA regulations at 42 CFR 422, as modified by guidance, with regard to Medicare-covered services and Prescription Drug Benefit program rules. All SNPs must provide Part D prescription drug coverage because special needs individuals must have access to prescription drugs to manage and control their special health c…
Site Overview
- Specific information about each of the three SNP types (C-SNPs, D-SNPs, and I-SNPs), as well as information on the SNP Application and the SNP Model of Care, can be found by clicking the appropriate links on the left-hand side of this page. In addition, there is a link below to the online Medicare Managed Care Manual, which contains Chapter 16b – CMS's current sub-regulatory gu…