When should I apply for Medicare Part B?
Additionally, HI 00805.275(G) states that lapses in Part B and/or GHP coverage from current employer do not disqualify me for a special enrollment period, as long as I did not have a lapse in coverage for more than 8 consecutive: The SEP provisions permit an 8-month period after the month GHP/LGHP coverage based on current
Should I terminate Part B of Medicare?
Mar 07, 2020 · The Medicare Part B SEP allows you to delay taking Part B if you have coverage through your own or a spouse’s current job. You usually have 8 months from when employment ends to enroll in Part B. Coverage that isn’t through a current job – such as COBRA benefits, retiree or individual-market coverage – won’t help you qualify for this SEP, but the ...
When to enroll in Medicare Part B?
Jun 07, 2021 · Special Enrollment Period (SEP) If you are age 65 or older, you or your spouse are still working and you are covered under a group health plan based on that current employment, you may not need to apply for Medicare medical insurance (Part B) at age 65. You may qualify for a "Special Enrollment Period" (SEP) that will let you sign up for Part B:
Should you decline Medicare Part B?
Special Enrollment Periods (SEPs) are periods of time outside normal enrollment periods when you can enroll in health insurance. They are typically triggered by specific circumstances. The Part B SEP starts when you have coverage from current work (job-based insurance) and you are in your first month of eligibility for Part B. It ends eight months after you lose

Can I drop Part B and add it later?
You can drop Medicare Part B coverage and re-enroll in it when you need it.Dec 18, 2021
Is Medicare Part B coverage retroactive?
If you are granted Social Security disability retroactively Social Security also offers you Part B coverage retroactively if you want it—while making it clear that, if you accept, you must pay backdated Part B premiums for the time period in question, which can amount to hundreds or even thousands of dollars.Oct 5, 2009
Which of the following is a qualifying life event for a Medicare Advantage Special Enrollment Period?
You qualify for a Special Enrollment Period if you've had certain life events, including losing health coverage, moving, getting married, having a baby, or adopting a child, or if your household income is below a certain amount.
How long is SEP for Medicare?
Your chance to join lasts for 2 full months after you drop your Medicare Cost Plan.
Are you automatically enrolled in Medicare if you are on Social Security?
Yes. If you are receiving benefits, the Social Security Administration will automatically sign you up at age 65 for parts A and B of Medicare. (Medicare is operated by the federal Centers for Medicare & Medicaid Services, but Social Security handles enrollment.)
Can you drop Medicare Part B anytime?
You can voluntarily terminate your Medicare Part B (medical insurance). However, since this is a serious decision, you may need to have a personal interview. A Social Security representative will help you complete Form CMS 1763.Nov 24, 2021
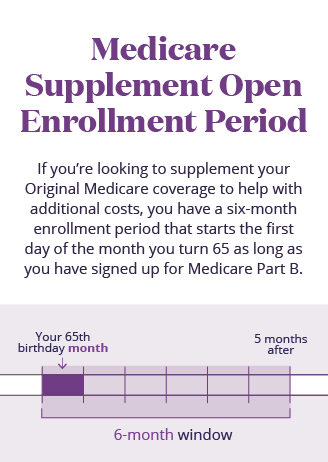
Can I change Medicare supplement plans anytime?
You can change your Medicare Supplement Plan anytime, just be aware that you might have to answer medical questions if your outside your Open Enrollment Period.
What is the initial enrollment period for Medicare?
7 monthsGenerally, when you turn 65. This is called your Initial Enrollment Period. It lasts for 7 months, starting 3 months before you turn 65, and ending 3 months after the month you turn 65.
What are the different enrollment periods for Medicare?
Most people qualify for Medicare because of age. If this is you, your first chance to sign up for Medicare is usually your Initial Enrollment Period, goes for seven months. It starts three months before your 65th birthday, includes the month of your 65th birthday, and ends three months later.
Does Medicare coverage start the month you turn 65?
For most people, Medicare coverage starts the first day of the month you turn 65. Some people delay enrollment and remain on an employer plan. Others may take premium-free Part A and delay Part B. If someone is on Social Security Disability for 24 months, they qualify for Medicare.
What is the correct enrollment period window for IEP2?
Initial Enrollment Period 2 (IEP2) Another enrollment period that is also 7-months is the Initial Enrollment Period 2. The IEP2 is for people who were already eligible for Part A and B before they turned 65. During the IEP2, you can sign up for a Medicare Advantage or Part D plan.Oct 25, 2021
What is the Medicare Part B special enrollment period (SEP)?
The Medicare Part B SEP allows you to delay taking Part B if you have coverage through your own or a spouse’s current job. You usually have 8 month...
Do I qualify for the Medicare Part B special enrollment period?
You qualify for the Part B SEP if: you are eligible for Medicare because of your age or because you collect disability benefits. (People who have E...
How do I use the Part B SEP?
To use this SEP you should call the Social Security Administration at 1-800-772-1213 and request two forms: the Part B enrollment request form (CMS...
What if an employer gives me money to buy my own health plan?
A note about individual coverage: you’ll qualify for an SEP if you delayed Part B because you had employer-sponsored coverage through a group healt...
When do you have to take Part B?
You have to take Part B once your or your spouse’s employment ends. Medicare becomes your primary insurer once you stop working, even if you’re still covered by the employer-based plan or COBRA. If you don’t enroll in Part B, your insurer will “claw back” the amount it paid for your care when it finds out.
What is a Part B SEP?
The Part B SEP allows beneficiaries to delay enrollment if they have health coverage through their own or a spouse’s current employer. SEP eligibility depends on three factors. Beneficiaries must submit two forms to get approval for the SEP. Coverage an employer helps you buy on your own won’t qualify you for this SEP.
How long can you delay Part B?
You can delay your Part B effective date up to three months if you enroll while you still have employer-sponsored coverage or within one month after that coverage ends. Otherwise, your Part B coverage will begin the month after you enroll.
What is a SEP for Medicare?
What is the Medicare Part B Special Enrollment Period (SEP)? The Medicare Part B SEP allows you to delay taking Part B if you have coverage through your own or a spouse’s current job. You usually have 8 months from when employment ends to enroll in Part B. Coverage that isn’t through a current job – such as COBRA benefits, ...
When does the enrollment period start for a group health plan?
Your initial enrollment period starts three months before the month you attain age 65 and ends three months after the month you turn 65. If your group health plan coverage is based on severance or retirement pay and the job your coverage is based on ended in the last eight months.
What is a SEP in health insurance?
You may qualify for a "Special Enrollment Period" (SEP) that will let you sign up for Part B: During any month you remain covered under the group health plan and your, or your spouse's, current employment continues; or.
How old do you have to be to get Medicare?
If you are age 65 or older, you or your spouse are still working and you are covered under a group health plan based on that current employment, you may not need to apply for Medicare medical insurance (Part B) at age 65. You may qualify for a "Special Enrollment Period" (SEP) that will let you sign up for Part B: 1 During any month you remain covered under the group health plan and your, or your spouse's, current employment continues; or 2 In the eight-month period that begins with the month after your group health plan coverage or the current employment it is based on ends, whichever comes first.#N#Exception: If your group health plan coverage or the employment it is based on ends during your initial enrollment period for Medicare Part B, you do not qualify for a SEP. Your initial enrollment period starts three months before the month you attain age 65 and ends three months after the month you turn 65. 3 If your group health plan coverage is based on severance or retirement pay and the job your coverage is based on ended in the last eight months.
Can I get a SEP if I have Social Security?
If you have that type of coverage, you will not be eligible for a SEP when it ends. To avoid paying a higher premium, make sure you sign up for Medicare when you are first eligible. People who receive Social Security disability benefits and are covered under a group health plan from either their own or a family member's current employment also have ...
What is a special enrollment period?
Special circumstances (Special Enrollment Periods) You can make changes to your Medicare Advantage and Medicare prescription drug coverage when certain events happen in your life, like if you move or you lose other insurance coverage. These chances to make changes are called Special Enrollment Periods (SEPs).
When does Medicare change coverage?
You can’t use this Special Enrollment Period from October–December. However, all people with Medicare can make changes to their coverage from October 15–December 7, and the changes will take effect on January 1.
What can I do with my Medicare Advantage Plan?
What can I do? Join a Medicare Advantage Plan with drug coverage or a Medicare Prescription Drug Plan. Switch from your current plan to another Medicare Advantage Plan with drug coverage or a Medicare Prescription Drug Plan. Drop your Medicare Advantage Plan with drug coverage and return to Original Medicare .
What is the difference between Medicare and Original Medicare?
Original Medicare. Original Medicare is a fee-for-service health plan that has two parts: Part A (Hospital Insurance) and Part B (Medical Insurance). After you pay a deductible, Medicare pays its share of the Medicare-approved amount, and you pay your share (coinsurance and deductibles).
How long does it take to switch plans after moving?
If you tell your plan before you move, your chance to switch plans begins the month before the month you move and continues for 2 full months after you move. If you tell your plan after you move, your chance to switch plans begins the month you tell your plan, plus 2 more full months.
How many times can you use Medicare Special Enrollment?
The month that the person is notified of Part A enrollment. This Medicare Special Enrollment Period can only be used one time during the TRICARE beneficiary’s lifetime.
When do you automatically enroll in Medicare?
Many people are automatically enrolled when they turn 65 or qualify through disability. Read about automatic enrollment and Medicare’s usual enrollment periods. Some people delay enrollment in Original Medicare, Part A and Part B, for a variety of reasons. For example, if you have group health coverage when you’re first eligible for Medicare, ...
How long do you have to enroll in Medicare after your employment ends?
When that employment – or your health coverage – ends, you can typically enroll in Part A and Part B with a Medicare Special Enrollment Period. You have eight months to enroll, beginning the month that employment or employment-based coverage ends – whichever happens first.
What is a SEP in Medicare?
A Medicare Special Enrollment Period (SEP) can let you sign up for Original Medicare Part A and/or Part B outside of regular enrollment periods. If you’re not eligible for an SEP, you’ll have usually to wait until the next General Enrollment Period to sign up for Part A and/or Part B. You might also have to pay a late enrollment penalty ...
How to contact Medicare for Part B?
For more information on Part B enrollment for U.S. citizens living abroad, contact Medicare at 1-800-MEDICARE (1-800-633-4227) . If you’re a TTY user, call 1-877-486-2048. Customer service representatives can be reached 24 hours a day, seven days a week.
How long do you have to be a volunteer to qualify for Medicare?
To qualify for a Medicare Special Enrollment Period, you must: Have volunteered for at least 12 months outside of the United States. Have volunteered for a tax-exempt program. Have had other health coverage for the duration that you served overseas.
Does Cobra count as Medicare?
Keep in mind that COBRA and retiree health insurance don’t count as coverage based on current employment and won’t qualify you for a Medicare Special Enrollment Period when it ends. You also won’t get a Medicare Special Enrollment Period if your group coverage or employment ends during your Medicare Initial Enrollment Period.
When is Medicare enrollment period?
During your Initial Enrollment Period (IEP) when you’re first eligible for Medicare. During the General Enrollment Period (GEP) from January 1 through March 31 of each year. If you’re eligible for a Special Enrollment Period (SEP), like if you’re covered under a group health plan (GHP) based on current employment.
How much is the late enrollment penalty for Part B?
If you sign up after your IEP, you may have to pay a late enrollment penalty (LEP) of 10% for each full 12-month period you don’t have Part B but were eligible to sign up.
How long does an IEP last?
Initial Enrollment Period. Your IEP is the first chance you have to sign up for Part B.It lasts for 7 months. It begins 3 months before the month you reach 65, and it ends 3 months after you reach 65.
What happens if you don't sign up for Part B?
If you don’t sign up for Part B during your IEP, you can sign up during the GEP. The GEP runs from January 1 through March 31 of each year. If you sign up during a GEP, your Part B coverage begins July 1 of that year. You may have to pay a late enrollment penalty if you sign up during the GEP. The cost of your Part B premium will go up 10% for each 12-month period that you could have had Part B but didn’t sign up. You may have to pay this late enrollment penalty aslong as you have Part B coverage.
What is the number to call for Part B?
If you have questions, call Social Security at 1-800-772-1213. TTY users should call 1-800-325-0778.
What is the OMB control number?
The valid OMB control number for this information collection is 0938-1230.
What is a special enrollment period for Medicare?
A Medicare Special Enrollment Period allows you to switch plans or sign up for Medicare outside of the standard Medicare enrollment periods. If you have Medicare: For people who already have Medicare and who experience a qualifying life event, there is a two-month Special Enrollment Period for switching a Medicare Advantage or Part D plan.
What happens if you enroll in Medicare after 2 months?
If you enroll after the two-month mark, you’ll face late enrollment penalties for Part D (regardless of whether you end up with a stand-alone Part D plan or a Medicare Advantage plan that includes drug coverage).
How long does it take to enroll in a 5 star plan?
You want to enroll in a 5-star plan at any time or drop your first Medicare Advantage plan within 12 months of enrolling. You move into or out of a qualified institutional facility, like a nursing home. You are enrolled in or lose eligibility for a qualified State Pharmaceutical Assistance Program.
What is Medicare Made Clear?
Medicare Made Clear is brought to you by UnitedHealthcare to help make understanding Medicare easier. Click here to take advantage of more helpful tools and resources from Medicare Made Clear including downloadable worksheets and guides.
What is a special enrollment period?
A Special Enrollment Period (SEP) is an enrollment period that takes place outside of the annual Medicare enrollment periods, such as the annual Open Enrollment Period. They are granted to people who were prevented from enrolling in Medicare during the regular enrollment period for a number of specific reasons.
When is the open enrollment period for Medicare?
Learn more and use this guide to help you sign up for Medicare. Open Enrollment: The fall Medicare Open Enrollment Period has officially begun and lasts from October 15 to December 7, 2020. You may be able to enroll in ...
How long do you have to disenroll from Medicare Advantage?
If you enrolled in a Medicare Advantage plan when you first became eligible for Medicare, you have 12 months to disenroll from the plan and transition back to Original Medicare.
What happens if you don't enroll in Medicare at 65?
If you did not enroll in Medicare when you turned 65 because you were still employed and were covered by your employer’s health insurance plan, you will be granted a Special Enrollment Period.
How long does Medicare Advantage coverage last?
If you had a Medicare Advantage plan with prescription drug coverage which met Medicare’s standards of “creditable” coverage and you were to lose that coverage through no fault of your own, you may enroll in a new Medicare Advantage plan with creditable drug coverage beginning the month you received notice of your coverage change and lasting for two months after the loss of coverage (or two months after receiving the notice, whichever is later).
How often can you change your Medicare Advantage plan?
If you move into, out of, or currently reside in a facility of special care such as a skilled nursing home or long-term care hospital, you may enroll in, disenroll from, or change a Medicare Advantage plan one time per month.
How long does it take to switch to another Medicare Advantage plan?
If you permanently move out of your Medicare Advantage plan’s coverage area or move to an area with more available plans, you may switch to another Medicare Advantage plan beginning the month before your move and lasting for two months.