The Bipartisan Budget Act of 2018 (Public Law No. 115-123) amended section 1852(a) of the Social Security Act to expand the types of supplemental benefits that may be offered by Medicare Advantage (MA) plans to chronically ill enrollees. We refer to these as Special Supplemental Benefits for the Chronically Ill (SSBCI). SSBCI include supplemental benefits that are not primarily health related and may be offered non-uniformly to eligible chronically ill enrollees, as discussed below. We believe the intended purpose of the new category of supplemental benefits is to enable MA plans to better tailor benefit offerings, address gaps in care, and improve health outcomes for the chronically ill population.
What does ssbci stand for?
The CHRONIC Care Act of 2018 gave Medicare Advantage plans new flexibility to offer Special Supplemental Benefits for the Chronically Ill (SSBCI) that are intended to help enrollees with specific chronic conditions. In 2019, MA plans offered a wider array of primarily health-related benefits. And, in 2020, plans began offering Special Supplemental Benefits for the Chronically …
Which health insurance plans offer ssbci?
Apr 24, 2019 · Medicare Advantage (MA) plans to chronically ill enrollees. We refer to these as Special Supplemental Benefits for the Chronically Ill (SSBCI). SSBCI include supplemental benefits that are not primarily health related and may be offered non-uniformly to eligible chronically ill enrollees, as discussed below.
What are special supplemental benefits for the chronically ill (ssbci)?
In simplest terms, SSBCI covers specific benefits designed to improve the health and overall quality of life for chronically ill enrollees. Individual MA plans can choose the benefits themselves since The Centers for Medicare and Medicaid Services (CMS) has given them "broad discretion" to develop their SSBCI programming.
Are ssbci benefits available in 2020?
Medicare Advantage Special Supplemental Benefits for Individuals with Chronic Illness. • Medicare Advantage (MA) plans may provide SSBCI for individuals with multiple chronic conditions. MA plans define benefits and eligibility within federal guidelines. • SSBCI address non-medical needs to help prevent costly emergency department visits, hospital admissions or …
What does Ssbci mean?
Special Supplemental Benefits for the Chronically IllSpecial Supplemental Benefits for the Chronically Ill (SSBCI) and New Primarily Health Related Benefits.
Who qualifies for Ssbci?
For a business to be eligible for the set aside, it must have least 51% of private or public ownership from socially and economically disadvantaged individuals. Like SSBCI 1.0, funds will be sent to states in three tranches.Aug 3, 2021
What are optional supplemental benefits?
Optional supplemental benefits (OSBs) are benefits that are not covered by original Medicare and which Medicare Advantage organizations (MAOs) offer to plan members for an additional premium. If offered, members can elect to purchase OSB coverage from their Medicare Advantage (MA) plans and receive additional benefits.Sep 30, 2021
What is special supplemental benefits for chronically ill Ssbci?
As of 2020, plans can also offer Special Supplemental Benefits for the Chronically Ill (SSBCI) — nonmedical services such as pest control. Goals: To assess the availability of and enrollment in MA plans offering new types of supplemental benefits in 2019 and 2020.Feb 10, 2021
What are some examples of health related benefits non health related benefits?
address enrollee social needs, such as non-fitness club memberships, community or social clubs, park passes, and access to companion care, marital counseling, family counseling, classes for enrollees with primary caregiving responsibilities for a child, or programs or events to address enrollee isolation and improve ...Apr 24, 2019
What is OSB dental?
Oral System Balance, or OSB, is different and focuses on something more basic: the oral structure. That is to say, how the teeth, gums and particularly the tongue are situated in the mouth, naturally affects your eating, speaking and, most importantly, your breathing.
What are OSB plans?
An Optional Supplemental Benefit (OSB) is an added benefit option, available with select plans, that a member may choose to elect in addition to the medical benefits covered by their Medicare Advantage plan.
Who is the largest Medicare Advantage provider?
UnitedHealthcareUnitedHealthcare is the largest provider of Medicare Advantage plans and offers plans in nearly three-quarters of U.S. counties.Dec 21, 2021
What is supplemental benefits for chronically ill?
What are SSBCI? SSBCI are benefits that can be offered to Medicare Advantage members with one or more complex chronic conditions, who are at high risk for hospitalization or adverse health outcomes, and who require intensive care coordination.
What are the added benefits to Medicare?
Medicare Advantage plans sometimes provide extra benefits including things like prescription drug coverage, dental care, routine vision, and routine hearing, among others. Want prescription drug coverage?Oct 1, 2021
What is SSBCI and why does it matter
In simplest terms, SSBCI covers specific benefits designed to improve the health and overall quality of life for chronically ill enrollees. Individual MA plans can choose the benefits themselves since The Centers for Medicare and Medicaid Services (CMS) has given them "broad discretion" to develop their SSBCI programming.
Why 2021 should be the year MA plans address SDoH
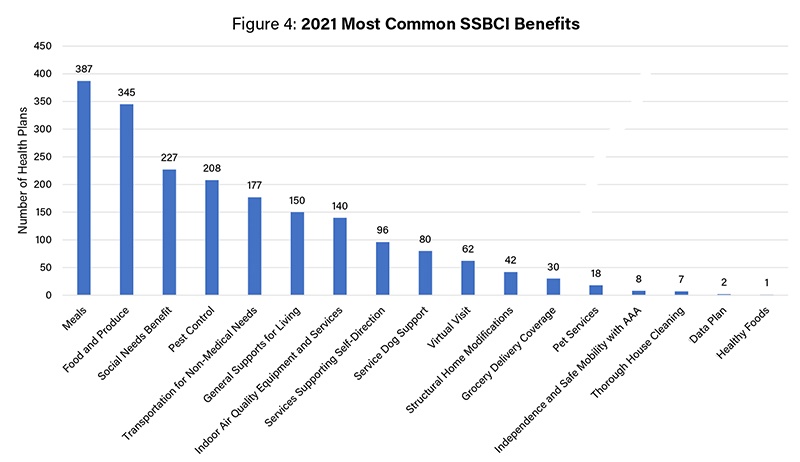
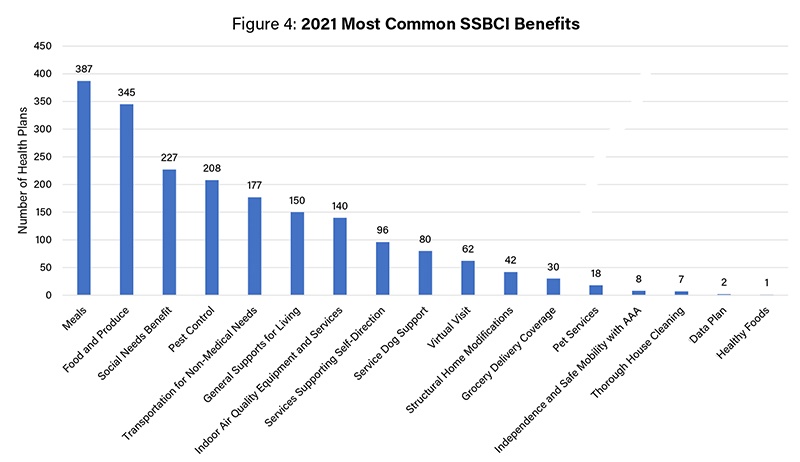
Supplemental benefits are not new, but too few MA plans are leveraging the expanded flexibilities effectively. To date, few MA plans offer the kind of benefits that fall within the SSBCI. Pest control, the most popular supplemental benefit, is offered by just 49 percent of MA plans. Food and produce assistance is offered by only 41 percent.
Your guide to SSBCI benefits
Ready to learn how MA plans can leverage SSBCI to keep costs in line as our population ages? Download our latest resource, Addressing SDoH Using Special Supplemental Benefits for the Chronically Ill.
What is MA plan?
MA plans are seeing increasing numbers of enrollees with complex medical needs and social risk factors. Research shows there is strong evidence that increased investment in selected social services and improved coordination between medical and non-medical services can improve health outcomes and lower health care costs for certain populations, including older adults and people with disabilities. By offering benefits that meet beneficiaries’ broader health-related social needs, MA plans can provide holistic, high-value care to this population. This has been particularly salient during the COVID-19 public health emergency, as MA plans provide services their beneficiaries need to stay safely in the home, such as delivered meals and virtual companionship.
Does Medicare cover social needs?
While traditional Medicare does not cover benefits to address social needs, Medicare Advantage (MA) plans have some flexibility to provide benefits — including food, prescription delivery, and housing supports — to meet the needs of members with complex chronic conditions. To maximize the potential of these new benefits, ...
What is SSBCI in Medicare?
The Bipartisan Budget Act of 2018 introduced new categories of supplemental benefits for the chronically ill. Special supplemental benefits for the chronically ill (“SSBCI”) include benefits that are not primarily health related and may be offered non-uniformly [1] to eligible enrollees. According to the new law, a chronically ill person: (1) has one or more comorbid and medically complex chronic conditions that is life threatening or significantly limits the overall health or function of the enrollee, (2) has a high risk of hospitalization or other adverse health outcomes, and (3) requires intensive care coordination. [2] For 2020, CMS will consider any enrollee with a condition identified as a chronic condition in section 20.1.2 of Chapter 16b of the Medicare Managed Care Manual to meet the statutory criterion (1) above, which would include approximately 73 percent of the Medicare Advantage population. Medicare Advantage plans must document their determinations that enrollees meet all three criterion above before providing SSBCI.
What is a supplemental benefit?
The move redefined “primarily health related” supplemental benefits to include items or services with a primary purpose to “diagnose, prevent, or treat an illness or injury, compensate for physical impairments, act to ameliorate the functional/psychological impact of injuries or health conditions, or reduce avoidable emergency and healthcare utilization.” A supplemental benefit is not primarily health related if it is solely or primarily used for cosmetic, comfort, or general use purposes. This week, while responding to requests for clarification, CMS provided the following examples of supplemental benefits that would qualify as primarily health related:
What is a cooking class?
Cooking classes as part of a nutritional/dietary or health education benefit. Fall prevention kits as part of home & bathroom safety devices. Implantable hearing aids, such as middle ear implants as part of a hearing benefit. CMS noted that such primarily health related supplemental benefits should be entered and briefly described in ...
What is a chronically ill person?
According to the new law, a chronically ill person: (1) has one or more comorbid and medically complex chronic conditions that is life threatening or significantly limits the overall health or function of the enrollee, (2) has a high risk of hospitalization or other adverse health outcomes, and (3) requires intensive care coordination. [2] .
Does Medicare Advantage offer supplemental benefits?
Last week, the Centers for Medicare and Medicaid Services (“CMS”) announced increased flexibility for Medicare Advantage health insurance plans to offer supplemental benefits (those benefits not covered under Medicare Parts A or B).
When will Medicare allow ESRD?
The Cures Act amended the Social Security Act (the Act) to allow all Medicare-eligible individuals with ESRD to enroll in MA plans beginning January 1, 2021. CMS is proposing to codify this statutory change in regulation. This proposed rule takes an important step in improving the lives of beneficiaries with ESRD, which is a priority in alignment with the Executive Order on Advancing American Kidney Health. By removing the barrier that beneficiaries with ESRD now face in terms of enrolling in MA plans, we are empowering them to choose the type of Medicare coverage that best meets their needs. This proposed rule also implements related MA and Medicare FFS payment changes made by the Cures Act—FFS coverage of kidney acquisition costs for MA beneficiaries and exclusion of such costs from MA benchmarks.”
What is a beneficiary RTBT?
CMS proposes that each Part D plan implement a beneficiary RTBT that will allow enrollees to view plan-provided, patient-specific, real-time formulary and benefit information by January 1, 2022. Plans would be able to use existing secure patient portals, develop a new portal, or use a computer application to fulfill this requirement. Plans would be required to also make this information available to enrollees who call the plan’s customer service call center. In order to encourage enrollees to use the beneficiary RTBT, we also propose to allow plans to offer rewards and incentives to their enrollees who log onto the beneficiary RTBT or seek to access this information via the plan’s customer service call center.
What are the C and D star ratings?
The Part C and D Star Ratings support CMS efforts to improve the level of accountability for the care provided by health and drug plans, physicians , hospitals, and other Medicare providers. In addition to routine measure updates and technical clarifications to the Star Ratings, CMS proposes to further increase the predictability and stability in the Star Ratings by directly reducing the influence of outliers on cut points. We also propose to further increase measure weights for patient experience/complaints and access measures from 2 to 4, reflecting CMS’s commitment to put patients first and to empower patients to work with their doctors to make healthcare decisions that are best for them.
How does CMS reduce administrative burden?
CMS proposes to reduce the administrative burden for PACE organizations by proposing to allow service delivery requests be approved in full by an interdisciplinary team (IDT) member at the time the request is made. This proposal eliminates the requirement that the IDT conduct a reassessment of the participant for service delivery requests that can be approved. We are also proposing to enhance participant protections by improving the participant appeals process, adding additional participant rights, increasing requirements related to the provision of services, and ensuring PACE organizations appropriately document care in the medical record while maintaining original communications from caregivers and others. CMS is also proposing to bolster CMS’s ability to access records, improve the regulatory framework relating to required services in PACE, and set out appeal processes for PACE organizations following certain enforcement actions.
Will CMS publish a call letter for 2021?
CMS will not publish a Call Letter for 2021. We believe that codifying the policies in regulation provides additional transparency and program stability, and allows MA organizations and Part D plan sponsors to develop more innovative plan designs. In addition, CMS will issue HPMS memoranda to communicate instructions, such as those around bidding, ...
What is the second specialty tier?
Part D sponsors and pharmacy benefit managers have requested a second specialty tier option, suggesting this would encourage the use of more preferred, less expensive agents, reduce enrollee cost sharing, and reduce costs to CMS. In response, with a proposed effective date of January 1, 2021, we propose to: allow Part D sponsors to establish a second, “preferred” specialty tier with lower cost sharing than the current specialty tier; codify the maximum cost sharing for the higher specialty tier; codify the methodology that determines and increases the specialty tier cost threshold; require sponsors to permit tiering exceptions between the two specialty tiers; and permit sponsors to determine which drugs go on either tier subject to the proposed cost threshold. This proposal supports the agency’s commitment to lowering drug prices for the Medicare population.
Do Part D plans have to disclose their performance?
Under the Part D program, plans currently do not have to disclose to CMS the measures they use to evaluate pharmacy performance in their network agreements. The measures used by plans potentially impact pharmacy reimbursements. Therefore, CMS proposes to require Part D plans to disclose such information to enable CMS to track how plans are measuring and applying pharmacy performance measures. CMS will also be able to report this information publicly to increase transparency on the process and to inform industry in their recent efforts to develop a standard set of pharmacy performance measures. CMS is also seeking comment on the Part D pharmacy performance measures more broadly, including recommendations for potential Part D Star Ratings metrics to incentivize the uptake of a standard set of measures.