Full Answer
How does Medicare billing work for hospitals?
Medicare billing works differently for Part A (hospital) services and Part B (medical) services. Hospitals receive a set amount of money for each visit from a Medicare beneficiary that is not dependent on the level of care rendered to the individual.
How does Medicare billing work with a superbill?
When billing for traditional Medicare (Parts A and B), billers will follow the same protocol as for private, third-party payers, and input patient information, NPI numbers, procedure codes, diagnosis codes, price, and Place of Service codes. We can get almost all of this information from the superbill, which comes from the medical coder.
What information do I need to bill for Medicare?
When billing for traditional Medicare (Parts A and B), billers will follow the same protocol as for private, third-party payers, and input patient information, NPI numbers, procedure codes, diagnosis codes, price, and Place of Service codes.
How long does it take for Medicare to process a bill?
Billing for Medicare. This process usually takes around 30 days. When billing for traditional Medicare (Parts A and B), billers will follow the same protocol as for private, third-party payers, and input patient information, NPI numbers, procedure codes, diagnosis codes, price, and Place of Service codes.
Is Medicare state or federal?
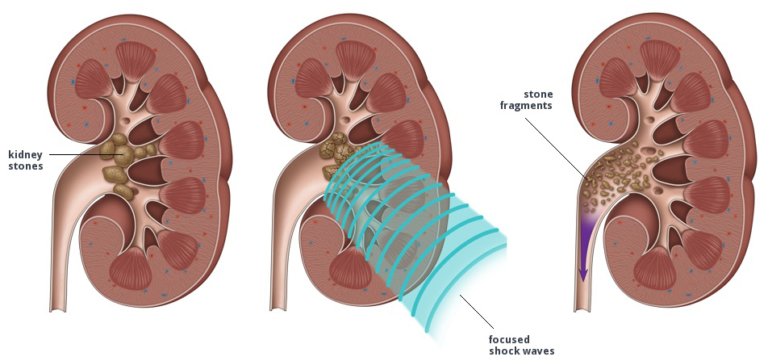
federalMedicare is the federal health insurance program for: People who are 65 or older. Certain younger people with disabilities. People with End-Stage Renal Disease (permanent kidney failure requiring dialysis or a transplant, sometimes called ESRD)
How are Medicare premiums billed?
All Medicare bills are due on the 25th of the month. In most cases, your premium is due the same month that you get the bill. Example of our billing timeline. For your payment to be on time, we must get your payment by the due date on your bill.
Does Medicare cost differ from state to state?
Medicare by State. Original Medicare (Part A and Part B) is a federal program so your coverage, costs and benefits will not be different from state to state. Medicare Advantage, Medicare Part D and Medigap plans are available through private insurers.
What is the Medicare state role?
We often focus on the role of states in administering and financing public programs like Medicaid, but states also serve as purchasers of private insurance for state employees and retirees, and as regulators of private insurance.
Why is my Medicare bill so high?
Medicare Part B covers doctor visits, and other outpatient services, such as lab tests and diagnostic screenings. CMS officials gave three reasons for the historically high premium increase: Rising prices to deliver health care to Medicare enrollees and increased use of the health care system.
How often do you pay Medicare premiums?
When do people pay their Medicare premiums? A person enrolled in original Medicare Part A receives a premium bill every month, and Part B premium bills are due every 3 months. Premium payments are due toward the end of the month.
Does Medicare follow from state to state?
Because it's a federal program, Medicare provides services in every part of the country. It doesn't matter which state you live in — your basic Medicare coverage will stay the same.
Is Medicare specific to the state?
Medicare Part A and Medicare Part B together are known as “original Medicare.” Original Medicare has a set standard for costs and coverage nationwide. That means your coverage will be the same no matter what state you live in, and you can use it in any state you visit.
Does Medicare cover all states?
If you have Original Medicare, you have coverage anywhere in the U.S. and its territories. This includes all 50 states, the District of Columbia, Puerto Rico, the Virgin Islands, Guam, American Samoa, and the Northern Mariana Islands. Most doctors and hospitals take Original Medicare.
Is health state or federal?
Generally, the federal government gives money to the states and territories for health services, as well as providing broad national policies on some health issues.
Does Medicare reimbursement vary by state?
Over the years, program data have indicated that although Medicare has uniform premiums and deductibles, benefits paid out vary significantly by State of residence of the beneficiary. These variations are due in part to the fact that reimbursements are based on local physicians' prices.
Who pays for Medicare Part A?
Most people receive Medicare Part A automatically when they turn age 65 and pay no monthly premiums. If you or your spouse haven't worked at least 40 quarters, you'll pay a monthly premium for Part A.
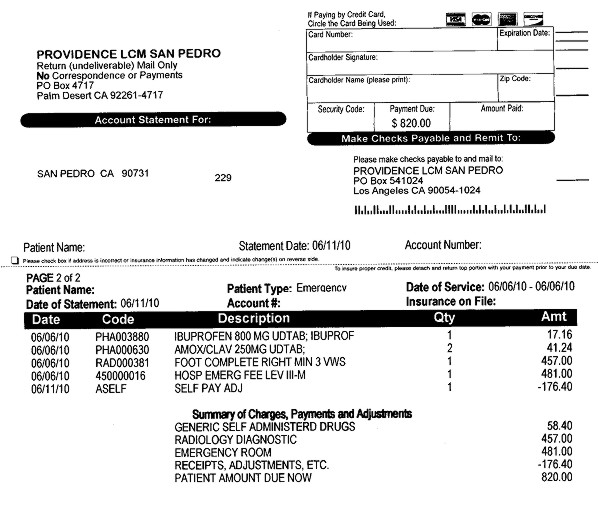
What form do you need to bill Medicare?
If a biller has to use manual forms to bill Medicare, a few complications can arise. For instance, billing for Part A requires a UB-04 form (which is also known as a CMS-1450). Part B, on the other hand, requires a CMS-1500. For the most part, however, billers will enter the proper information into a software program and then use ...
What is a medical biller?
In general, the medical biller creates claims like they would for Part A or B of Medicare or for a private, third-party payer. The claim must contain the proper information about the place of service, the NPI, the procedures performed and the diagnoses listed. The claim must also, of course, list the price of the procedures.
What is 3.06 Medicare?
3.06: Medicare, Medicaid and Billing. Like billing to a private third-party payer, billers must send claims to Medicare and Medicaid. These claims are very similar to the claims you’d send to a private third-party payer, with a few notable exceptions.
How long does it take for Medicare to process a claim?
The MAC evaluates (or adjudicates) each claim sent to Medicare, and processes the claim. This process usually takes around 30 days .
Is it harder to bill for medicaid or Medicare?
Billing for Medicaid. Creating claims for Medicaid can be even more difficult than creating claims for Medicare. Because Medicaid varies state-by-state, so do its regulations and billing requirements. As such, the claim forms and formats the biller must use will change by state. It’s up to the biller to check with their state’s Medicaid program ...
Can you bill Medicare for a patient with Part C?
Because Part C is actually a private insurance plan paid for, in part, by the federal government, billers are not allowed to bill Medicare for services delivered to a patient who has Part C coverage. Only those providers who are licensed to bill for Part D may bill Medicare for vaccines or prescription drugs provided under Part D.
Do you have to go through a clearinghouse for Medicare and Medicaid?
Since these two government programs are high-volume payers, billers send claims directly to Medicare and Medicaid. That means billers do not need to go through a clearinghouse for these claims, and it also means that the onus for “clean” claims is on the biller.
Why do doctors bill Medicare for services that were not rendered?
Because there is no direct oversight of Medicare’s billing system doctors, sometimes in concert with patients, bill Medicare for services that were not rendered in order to get a larger reimbursement.
How does Medicare work?
How Medicare Billing Works. Medicare was designed in 1965 as a single payer health system that is publicly funded. The funds to pay for Medicare services are collected from employers and self-employed individuals. The Federal Insurance Contributions Act taxes employers and employees a total of 2.9% of an individual’s income.
What is single payer health care?
In a single payer health system, providers receive payment for services rendered from a general pool of funds that everyone contributes to through taxes. The Medicare program has established a long list of services they will cover and the fee that Medicare will pay to a provider for a service provided to a beneficiary.
How much does Medicare pay for non-participating providers?
Non-participating Medicare providers will receive 80% of the Medicare determined fee and are allowed to bill 15% or more of the remaining amount to the beneficiary. Medicare billing works differently ...
How much did Medicare cost in 2008?
As of 2008 Medicare cost the American public $386 billion which was roughly 13% of the total federal budget. While Medicare is project to take up only 12.5% of the federal budget in 2010, costs will rise to $452 billion.
How much does the Federal Insurance Contributions Act tax?
The Federal Insurance Contributions Act taxes employers and employees a total of 2.9% of an individual’s income. Employees pay 1.45% and employers pay a matching 1.45% tax. Self employed individuals must pay the entire 2.9% tax themselves to contribute to the Medicare program.
Is Medicare billing wheel chairs fraudulent?
Other fraudulent schemes include billing Medicare for durable medical goods such as wheel chairs multiple times for just one chair, and never even delivering the wheel chair. Medicare billing has become a hot button topic in the United States. A lack of oversight on billing combined with ever increasing costs for medical services is causing ...
When do hospitals report Medicare beneficiaries?
If the beneficiary is a dependent under his/her spouse's group health insurance and the spouse retired prior to the beneficiary's Medicare Part A entitlement date, hospitals report the beneficiary's Medicare entitlement date as his/her retirement date.
What is secondary payer?
Medicare is the Secondary Payer when Beneficiaries are: 1 Treated for a work-related injury or illness. Medicare may pay conditionally for services received for a work-related illness or injury in cases where payment from the state workers’ compensation (WC) insurance is not expected within 120 days. This conditional payment is subject to recovery by Medicare after a WC settlement has been reached. If WC denies a claim or a portion of a claim, the claim can be filed with Medicare for consideration of payment. 2 Treated for an illness or injury caused by an accident, and liability and/or no-fault insurance will cover the medical expenses as the primary payer. 3 Covered under their own employer’s or a spouse’s employer’s group health plan (GHP). 4 Disabled with coverage under a large group health plan (LGHP). 5 Afflicted with permanent kidney failure (End-Stage Renal Disease) and are within the 30-month coordination period. See ESRD link in the Related Links section below for more information. Note: For more information on when Medicare is the Secondary Payer, click the Medicare Secondary Payer link in the Related Links section below.
Does Medicare pay for black lung?
Federal Black Lung Benefits - Medicare does not pay for services covered under the Federal Black Lung Program. However, if a Medicare-eligible patient has an illness or injury not related to black lung, the patient may submit a claim to Medicare. For further information, contact the Federal Black Lung Program at 1-800-638-7072.
Does Medicare pay for the same services as the VA?
Veteran’s Administration (VA) Benefits - Medicare does not pay for the same services covered by VA benefits.
Is Medicare a primary or secondary payer?
Providers must determine if Medicare is the primary or secondary payer; therefore, the beneficiary must be queried about other possible coverage that may be primary to Medicare. Failure to maintain a system of identifying other payers is viewed as a violation of the provider agreement with Medicare.
How much is Medicare reimbursement for 2020?
Reimbursements match similar in-person services, increasing from about $14-$41 to about $60-$137, retroactive to March 1, 2020. In addition, Medicare is temporarily waiving the audio-video requirement for many telehealth services during the COVID-19 public health emergency. Codes that have audio-only waivers during the public health emergency are ...
What is the CPT code for Telehealth?
Medicare increased payments for certain evaluation and management visits provided by phone for the duration of the COVID-19 public health emergency: Telehealth CPT codes 99441 (5-10 minutes), 99442 (11-20 minutes), and 99443 (20-30 minutes)
Does Medicare cover telehealth?
Telehealth codes covered by Medicare. Medicare added over one hundred CPT and HCPCS codes to the telehealth services list for the duration of the COVID-19 public health emergency. Telehealth visits billed to Medicare are paid at the same Medicare Fee-for-Service (FFS) rate as an in-person visit during the COVID-19 public health emergency.
How long can you switch Medicare Advantage plan in Maine?
But, in Maine, you can “try” the Advantage plan for three years, and you have 90 days after dropping the policy to switch to a supplement with Guaranteed Issue ...
How long can you change your Medigap plan?
Some states allow the “Birthday Rule,” which allows a 30-day timeframe for you to change your Medigap plan after your birthday every year. Also, you can change plans without underwriting as long as the policy benefits are equal to or less than your current plan.
How long does it take to switch Medigap plans?
Missouri – If you have a Medigap policy, you can switch plans within 60 days of your enrollment anniversary . New York – You can enroll in a Medigap policy without underwriting throughout the year. Washington – Allows Medigap enrollees to change Medigap plans (except for Plan A) at any point.
Does Medigap cover excess charges?
If you’re looking at purchasing a Medigap policy, you may find that some of the plans cover excess charges. When a doctor doesn’t accept Medicare, excess charges may occur; doctors can only charge 15% above the threshold.
Can you cancel your health insurance in Wisconsin?
In the state of Wisconsin, if the annual premium of your employer plan is over 125% of the Basic Annual Premium for your gender and age, then you may qualify for Guaranteed Issue. No Conditions – You may decide to cancel your group health insurance and make Medicare primary.
Is Medicare primary or secondary?
If your employer’s health care policy is the primary form of insurance, and Medicare is secondary.
Is Medicare open enrollment in 2021?
Updated on July 15, 2021. Even though Medicare is a Federal program, some states have different terms for Open Enrollment, Guaranteed Issue Rights, excess charges, disability, etc. Below, we’ll highlight what states have their own unique rules.
What is the form for Medicare Part B?
Some FOs use Form CMS-18F, "Application for Hospital Insurance" for all Medicare applications and do not stock Form CMS-4040. Form CMS-18F may be used to enroll for Medicare Part B. . Most of the information which is requested on the application can be obtained from local county eligibility records.
What is the agency code for a third party billing action?
Each third party billing action must include an agency code in order to identify the state and the account to which the action applies. The unique assigned three-position agency code identifies: 1) the type of organization; 2) the type of account; and 3) the specific organization itself.
Does Medicare Part D require a premium?
premium, covers most other types of health coverage, including limited prescription drug coverage. Medicare Part D, also optional, requires a premium, and covers outpatient prescription drugs. Medicare Parts A, B, and D all require payment of cost-sharing (e.g., deductibles, coinsurance, and copayments).
Is FFP available for Medicare Part B?
However, states have an interest in ensuring Medicare Part B enrollment for such individuals since FFP is not available for Medicaid costs that Part B could have covered had individuals been had enrolled in it. 42 CFR §431.625(d)(3).