A Medicare program to help people with limited income and resources pay Medicare prescription drug costs, such as premiums, deductibles, and coinsurance. FEDERAL EMPLOYEE HEALTH BENEFITS PLAN (FEHP) The FEHB Program offers health coverage for current and retired federal employees.
Full Answer
What is Medicare in simple terms?
What is Medicare, and who can get it?
- I am 65 years of age or older.
- I am under 65, but I receive disability benefits from the Social Security Administration (SSA) or the Railroad Retirement Board (RRB).
- I have amyotrophic lateral sclerosis (ALS, or Lou Gehrig’s disease).
- I have end-stage renal disease (ESRD), which is permanent kidney failure that requires a transplant or dialysis.
What is the difference between Medicare and medical?
• Medicare is not a dependent upon the needs of an individual whereas Medical is a need based insurance program. • Medicare is a federally funded program whereas Medical is an insurance program started by the State of California with funds shared by state and federal governments.
What is the difference between Medicare and medicade?
Additionally, many beneficiaries are also able to receive Medicaid to help "pay for hospital stays, doctor bills, prescription drugs, and other health costs." Unlike a private retirement account ...
Is Medicare and Medicaid the same thing?
No, these are two separate and distinct programs. Medicare is a federal program designed to assist older persons with healthcare coverage while Medicaid is funded jointly between the Federal and state governments and assists low income individuals and families.

What does the term Medicare mean?
Medicare is the federal health insurance program for: People who are 65 or older. Certain younger people with disabilities. People with End-Stage Renal Disease (permanent kidney failure requiring dialysis or a transplant, sometimes called ESRD)
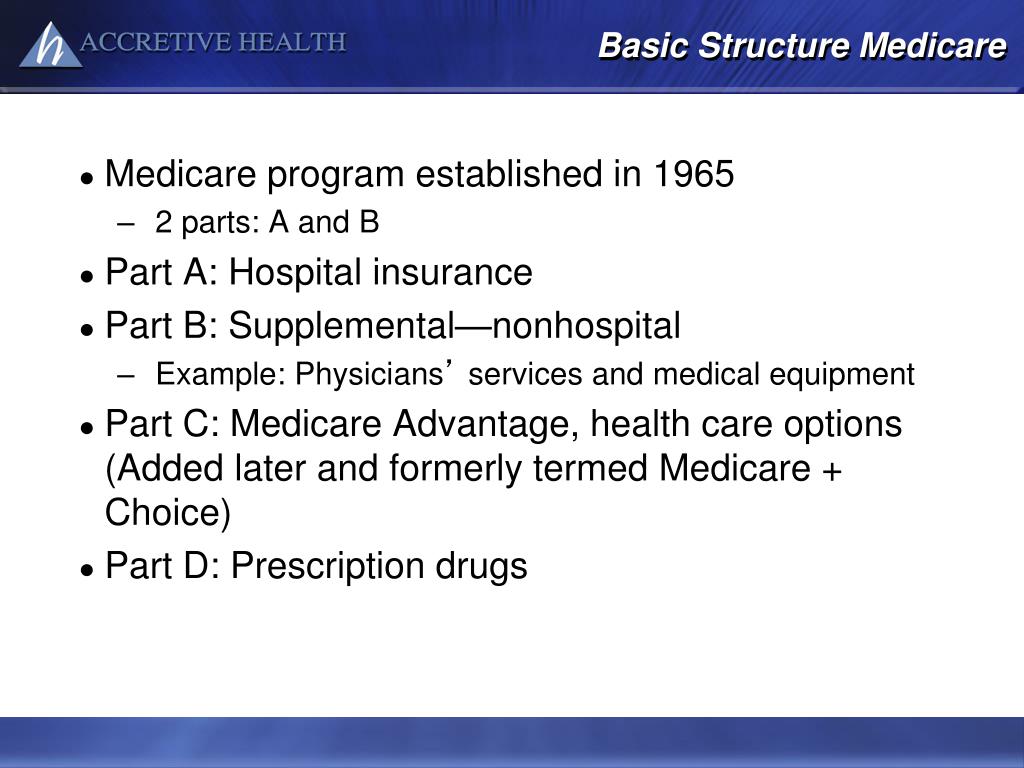
What are the 4 types of Medicare?
There are four parts of Medicare: Part A, Part B, Part C, and Part D.Part A provides inpatient/hospital coverage.Part B provides outpatient/medical coverage.Part C offers an alternate way to receive your Medicare benefits (see below for more information).Part D provides prescription drug coverage.
What are the three types of Medicare?
Different types of Medicare health plansMedicare Advantage Plans. ... Medicare Medical Savings Account (MSA) Plans. ... Medicare health plans (other than MA & MSA) ... Rules for Medicare health plans.
Do I automatically get Medicare when I turn 65?
Yes. If you are receiving benefits, the Social Security Administration will automatically sign you up at age 65 for parts A and B of Medicare. (Medicare is operated by the federal Centers for Medicare & Medicaid Services, but Social Security handles enrollment.)
Who is eligible for Medicare?
Generally, Medicare is available for people age 65 or older, younger people with disabilities and people with End Stage Renal Disease (permanent kidney failure requiring dialysis or transplant). Medicare has two parts, Part A (Hospital Insurance) and Part B (Medicare Insurance).
What part of Medicare is free?
Part APart A covers inpatient hospital stays, care in a skilled nursing facility, hospice care, and some home health care. coverage if you or your spouse paid Medicare taxes for a certain amount of time while working. This is sometimes called "premium-free Part A." Most people get premium-free Part A.
Do you automatically get Medicare with Social Security?
You automatically get Medicare because you're getting benefits from Social Security (or the Railroad Retirement Board). Part B covers certain doctors' services, outpatient care, medical supplies, and preventive services.
Is Medicare and Medicaid the same?
The difference between Medicaid and Medicare is that Medicaid is managed by states and is based on income. Medicare is managed by the federal government and is mainly based on age. But there are special circumstances, like certain disabilities, that may allow younger people to get Medicare.
What is the difference between Medicare A and B?
Medicare Part A and Medicare Part B are two aspects of healthcare coverage the Centers for Medicare & Medicaid Services provide. Part A is hospital coverage, while Part B is more for doctor's visits and other aspects of outpatient medical care.
Can I get Medicare Part B for free?
While Medicare Part A – which covers hospital care – is free for most enrollees, Part B – which covers doctor visits, diagnostics, and preventive care – charges participants a premium. Those premiums are a burden for many seniors, but here's how you can pay less for them.
How much Social Security will I get at the age of 65?
How Your Social Security Benefit Is ReducedIf you start getting benefits at age*And you are the: Wage Earner, the benefit amount you will receive is reduced toAnd you are the: Spouse, the benefit amount you will receive is reduced to6593.345.865 + 1 month93.946.265 + 2 months94.446.565 + 3 months95.046.946 more rows
Do I need to contact Social Security when I turn 65?
Is it automatic when I turn 65? To enroll in Medicare, most people need to contact Social Security directly. Do this before your 65th birthday to avoid a lapse in health coverage.
Does Medicare honor WC cases?
Answer: Medicare will generally honor judicial decisions issued after a hearing on the merits of a WC case by a court of competent jurisdiction. If a court or other adjudicator of the merits specifically designates funds to a portion of a settlement that is not related to medical services
Can you appeal a set aside from Medicare?
Answer: The CMS has no formal appeals process for rejection of a Medicare set-aside arrangement. However, when CMS does not believe that a proposed set-aside adequately protects Medicare’s interests, the parties may provide the RO with additional information/documentation in order to justify their proposal. If the additional information does not convince the RO to approve the set-aside arrangement, and the parties proceed to settle the case despite the ROs objections, then Medicare will not recognize the settlement. Medicare will exclude its payments for the medical expenses related to the injury or illness until such time as WC settlement funds expended for services otherwise reimbursable by Medicare exhaust the entire settlement. At this point, when Medicare denies a particular beneficiary’s claim, the beneficiary may appeal that particular claim denial through Medicare's regular administrative appeals process. Information on applicable appeal rights is provided at the time of each claim denial.
Is third party liability insurance primary to Medicare?
Answer: Third party liability insurance proceeds are also primary to Medicare. To the extent that a liability settlement is made that relieves a WC carrier from any future medical expenses, a CMS approved Medicare set-aside arrangement is appropriate. This set-aside would need sufficient funds to cover future medical expenses incurred once the total third party liability settlement is exhausted. The only exception to establishing a Medicare set-aside arrangement would be if it can be documented that the beneficiary does not require any further WC claim related medical services. A Medicare set-aside arrangement is also unnecessary if the medical portion of the WC claim remains open, and WC continues to be responsible for related services once the liability settlement is exhausted.
Can Medicare be set aside after death?
Answer: Once the RO and the contractor responsible for monitoring the beneficiary's case ensure that all of the beneficiary's claims have been paid, then any amount left over in the beneficiary's Medicare set-aside arrangement may be disbursed pursuant to state law, once Medicare’s interests have been protected. This may involve holding the Medicare set-aside arrangement open for some period after the date of death, as providers, physicians, and other suppliers are permitted to submit their initial bill to Medicare for a period ranging from 15-27 months after the date of service.
What is a script in Medicare?
Informational scripts are designed to respond to beneficiary questions and requests and provide objective information about a plan or the Medicare program. Sales and enrollment scripts are intended to steer a beneficiary towards a plan or limited number of plans, or to enroll a beneficiary into a plan.
What is an educational event for Medicare?
Educational events are designed to inform Medicare beneficiaries about Medicare Advantage, Prescription Drug or other Medicare programs and do not include marketing (i.e., the event sponsor does not steer, or attempt to steer, potential enrollees toward a specific plan or limited number of plans).
What is co-branding in Medicare?
Co-branding is defined as a relationship between two or more separate legal entities, one of which is an organization that sponsors a Medicare plan. Co-branding is when a Plan/Part D Sponsor displays the name(s) or brand(s) of the co-branding entity or entities on its marketing materials to signify a business arrangement. Co-branding arrangements allow a Plan/Part D Sponsor and its co-branding partner(s) to promote enrollment in the plan. Co-branding relationships are entered into independent of the contract that the Plan/Part D Sponsor has with CMS.
What is Medicare marketing guidelines?
The Medicare Marketing Guidelines (MMG) implement the Centers for Medicare & Medicaid Services’ (CMS) marketing requirements and related provisions of the Medicare Advantage (MA, MA-PD ) (also referred to as Plan), Medicare Prescription Drug Plan (PDP) (also referred to as Part D Sponsor), and except where otherwise specified, Section 1876 cost plans (also referred to as Plan) rules, (i.e., Title 42 of the Code of Federal Regulations, Parts 422, 423, and 417). These requirements also apply to Medicare-Medicaid Plans (MMPs), except as modified or clarified in state-specific marketing guidance for each state’s demonstration. State-specific guidance is considered an addendum to the MMG. State-specific marketing guidance for MMPs will be posted to http://www.cms.gov/Medicare-
What is a non-benefit/non-health service provider?
Third parties that provide non-benefit/non-health services (“Non-benefit/non-health service providing third party entities”) are organizations or individuals that supply non-benefit related information to Medicare beneficiaries or a Plan’s/Part D Sponsor’s membership, which is paid for by the Plan/Part D Sponsor or the non-benefit/non-health service-providing third-party entity.
What is the Office of Medicare Hearings and Appeals responsible for?
Please note that the Office of Medicare Hearings and Appeals is responsible only for the Level 3 claims appeals and certain Medicare entitlement appeals and Part B premium appeals. OMHA is not responsible for levels 1, 2, 4, and 5 of the appeals process.
What is Medicare level 1 appeal?
At Level 1, your appeal is called a request for reconsideration. You may request reconsideration by your Medicare Advantage plan within 60 days of being notified by your Medicare Advantage plan of its initial decision to not pay for, not allow, or stop a service ("organization determination").
What happens if my Medicare Advantage plan does not meet the response deadline?
If your Medicare Advantage plan fails to meet the established deadlines, it is required to forward your appeal to an independent outside entity for a Level 2 review. Your plan does not decide in your favor.
Can you appeal a Medicare Advantage plan?
If you are in a Medicare Advantage plan, you can appeal the plan's decision to not pay for, not allow, or stop a service that you think should be covered or provided . You may contact your plan or consult your plan materials for detailed information about requesting an appeal and your appeal rights.
Does Medicare Advantage plan decide in your favor?
Your plan does not decide in your favor. If during your Level 1 appeal ("reconsideration") your Medicare Advantage plan does not decide in your favor, it is required to forward your appeal to an independent outside entity for a Level 2 review.
Can you request an expedited reconsideration with Medicare?
You or your physician may request an expedited reconsideration by your Medicare Advantage plan in situations where the standard reconsideration time frame might jeopardize your health, life, or ability to regain maximum function. If you are receiving services in an inpatient hospital, skilled nursing facility, home health agency or comprehensive ...
Why is Medicare Advantage so popular?
Medicare Advantage is a popular health insurance option because it works like private health insurance for Medicare beneficiaries. In fact, according to the Centers for Medicare & Medicaid Services, more than 60 million Americans enrolled in Medicare in 2019. Of these Medicare enrollees, more than 37 percent were enrolled in a Medicare Advantage ...
When is the open enrollment period for Medicare?
Open enrollment period (October 15–December 7). During this time, you can switch from original Medicare (parts A and B) to Part C (Medicare Advantage), or from Part C back to original Medicare. You can also switch Part C plans or add, remove, or change a Part D plan. General enrollment period (January 1–March 31).
How long does it take to sign up for Medicare?
Initial enrollment period. This is a 7-month window around your 65th birthday when you can sign up for Medicare. It begins 3 months before your birth month, includes the month of your birthday, and then extends 3 months after your birthday. During this time, you can enroll for all parts of Medicare without a penalty.
Does Medicare Advantage have coinsurance?
Most Medicare Advantage plans charge a copayment or coinsurance amount for services rendered. These services could include a doctor’s office visit, specialist’s office visit, or even a prescription drug refill. Specific coinsurance and copayment amounts are set by the plan you’re enrolled in.
Does Medicare Advantage cover hospital services?
This includes any hospital services covered under Medicare Part A and any medical services covered under Medicare Part B. Some Medicare Advantage plans also cover additional healthcare needs, including: However, this coverage varies by plan, and each Medicare Advantage plan can choose what additional coverage to offer.
Does Medicare Advantage cover prescription drugs?
Most Medicare Advantage plans include this coverage, which helps pay for the cost of your medications. Only certain types of prescription drugs are required to be covered under Part D, however — so you’ll want to make sure to check for coverage of your medications before enrolling in an Advantage plan.
Can you charge separate deductibles for Medicare Advantage?
In addition, Advantage plans can charge separate drug and health plan deductibles. Individual healthcare needs play a huge role in how much you may end up paying out of pocket for your Medicare Advantage plan. For example, your plan costs can be affected by: how often you seek services.
When will Medicare reassign to a new plan?
11208) (BLUE Notice) Informs people that their current Medicare drug plan is leaving the Medicare Program and they’ll be reassigned to a new Medicare drug plan effective January 1, 2021, unless they join a new plan on their own by December 31, 2020. • Keep the notice.
When will non-chooser LIS join a new Medicare plan?
Informs non-chooser LIS members that because their current Medicare drug plan premium is increasing above the regional LIS premium subsidy amount, they’ll e reassigned to a new Medicare drug plan effective January 1, 2021, unless they join a new plan on their own by December 31, 2020. LIS Qualifications & Benchmark Articles.
When do you have to join Medicare 2021?
You must join a Medicare drug plan by February 28 if you want Medicare drug coverage for 2021. Daily - ongoing. CMS.
