When an ESRD
Chronic Kidney Disease
A condition characterized by a gradual loss of kidney function.
Hewlett-Packard
The Hewlett-Packard Company or Hewlett-Packard was an American multinational information technology company headquartered in Palo Alto, California. It developed and provided a wide variety of hardware components as well as software and related services to consumers, small- and mediu…
When does 30 month coordination period start?
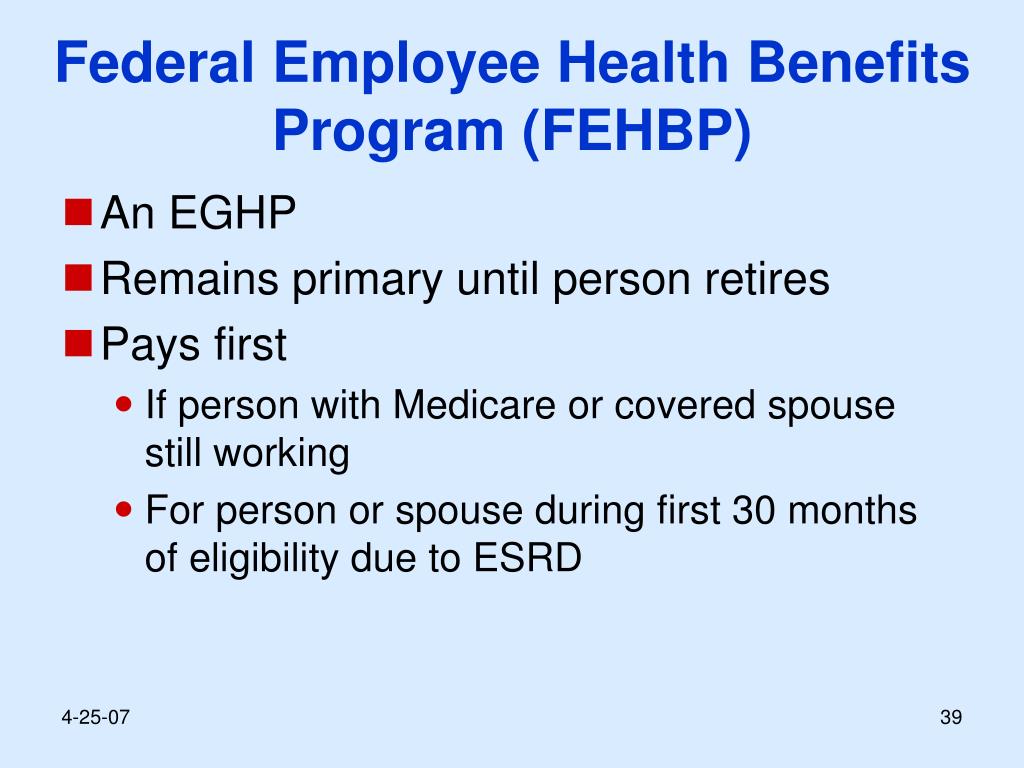
The 30-month coordination period, for people with End-Stage Renal Disease (ESRD), is the period when a group health plan (GHP) pays first and Medicare pays second for health care costs. The coordination period begins when your eligibility for ESRD Medicare begins, even if you haven’t enrolled for ESRD Medicare yet. Even though your GHP pays primary during this period, you …
What happens if I miss the Medicare annual enrollment period?
remain primary for 30 months, beginning the month you first become eligible for ESRD Medicare. This is called the 30-month coordination period. During the 30-month coordination period: You do not have to sign up for ESRD Medicare immediately if you have GHP coverage Your GHP coverage must pay first, and ESRD Medicare may pay second for
What does Medicare mean by benefit period?
The 30-month coordination period when Group Health Plan insurance is primary to Medicare continues uninterrupted. At the end of the 30-month coordination period, Medicare becomes the primary payer of benefits, even if Medicare would otherwise be secondary under the Working Aged or Disability guidelines.
What is the initial enrollment period (IEP) for Medicare?
The COB is a 30-month period in which Medicare is the secondary payer. This begins with the first month the patient is eligible for Medicare due to permanent kidney disease, whether or not the patient applies. In the case of hemodialysis Medicare becomes active on the first day of the 4th month of dialysis, which begins the 30 month COB period.

Why is the 30-month coordination period so important?
The 30-month coordination period when Group Health Plan insurance is primary to Medicare continues uninterrupted. At the end of the 30-month coordination period, Medicare becomes the primary payer of benefits, even if Medicare would otherwise be secondary under the Working Aged or Disability guidelines.Oct 4, 2021
When does a patient's 30-month coordination period begin?
The 30-month coordination period begins when eligibility for ESRD Medicare begins, even if you haven't signed up for ESRD Medicare yet. For example, if Mr. X begins dialysis at a facility in September of 2017, he is eligible for Medicare the first day of the fourth month he gets dialysis, which is December 1, 2017.
How long is the coordination period for ESRD?
Your group health plan (GHP) coverage–meaning job-based, retiree, or COBRA coverage– will remain primary for 30 months, beginning the month you first become eligible for ESRD Medicare. This is called the 30-month coordination period.
How many months is the coordination period for beneficiaries who have Medicare based on ESRD with a GHP?
Medicare is the secondary payer to group health plans (GHPs) for individuals entitled to Medicare based on ESRD for a coordination period of 30 months regardless of the number of employees and whether the coverage is based on current employment status.Dec 1, 2021
When is ESRD Medicare primary?
If you have ESRD and need dialysis (also known as 'hemodialysis'), your Medicare coverage starts the first day after the 3rd full month of dialysis in a clinic.
When does Medicare become primary?
Even if you have a group health plan, Medicare is the primary insurer as long as you've been eligible for Medicare for 30 months or more.
How long are providers required to retain Medicare secondary payer records?
10 yearsBased on this regulation, hospitals must document and maintain MSP information for Medicare beneficiaries. Without this documentation, the contractor would have nothing to audit submitted claims against. CMS recommends that providers retain MSP information for 10 years.
Why does Medicare cover end stage renal disease?
Medicare for those with End-Stage Renal Disease (ESRD Medicare) provides you with health coverage if you have permanent kidney failure that requires dialysis or a kidney transplant. ESRD Medicare covers a range of services to treat kidney failure.
Does Medicare coverage start the month you turn 65?
For most people, Medicare coverage starts the first day of the month you turn 65. Some people delay enrollment and remain on an employer plan. Others may take premium-free Part A and delay Part B. If someone is on Social Security Disability for 24 months, they qualify for Medicare.
What is the GFR for end stage renal disease?
ESRD is a terminal illness defined as having a glomerular filtration rate of less than 15 mL/min.
When is Medicare Secondary Payer?
Medicare Secondary Payer (MSP) is the term generally used when the Medicare program does not have primary payment responsibility - that is, when another entity has the responsibility for paying before Medicare.Dec 1, 2021
When does Medicare end after kidney transplant?
When Medicare coverage ends If you're eligible for Medicare only because of permanent kidney failure, your Medicare coverage will end: 12 months after the month you stop dialysis treatments. 36 months after the month you have a kidney transplant.
When does Medicare coverage end?
If the beneficiary has Medicare only because of ESRD, Medicare coverage will end when one of the following conditions is met: 12 months after the month the beneficiary stops dialysis treatments, or. 36 months after the month the beneficiary had a kidney transplant.
When does Medicare start?
2. Medicare coverage can start as early as the first month of dialysis if:
What is the term for a kidney that stops working?
End-Stage Renal Disease (ESRD) End-Stage Renal Disease (ESRD) is a medical condition in which a person's kidneys cease functioning on a permanent basis leading to the need for a regular course of long-term dialysis or a kidney transplant to maintain life.
How long does Medicare cover a transplant?
Medicare coverage can start two months before the month of the transplant if the transplant is delayed more than two months after the beneficiary is admitted to the hospital for that transplant or for health care services that are needed before the transplant.
Is Medicare a secondary plan?
Medicare is secondary to GHP coverage provided through the Consolidated Omnibus Budget Reconciliation Act (COBRA), or a retirement plan. Medicare is secondary during the coordination period even if the employer policy or plan contains a provision stating that its benefits are secondary to Medicare.
