The 8-minute rule only applies to time-based CPT codes for manual and physical therapy. This falls under Medicare Part B for outpatient therapy. How Does the 8-Minute Rule Work? The 8-minute rule states that to receive Medicare reimbursement, you must provide treatment for at least eight minutes.
What is the 8-minute rule for Medicare Part B billing?
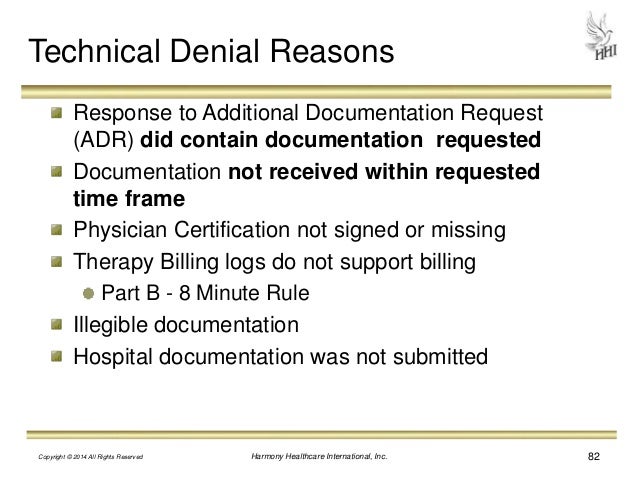
Using CMS’s interpretation of aggregating timed procedure codes (the 8-minute rule) is mandatory when you submit reimbursement claims for Medicare Part B billing. However, some private insurers use the 8-minute rule, the AMA Rule of Eights, or their own proprietary billing rules.
Does Medicare require the 8-minute rule for outpatient services?
Since Medicare requires the 8-minute rule to be followed for these in-person, outpatient services, providers do not have the choice of using another billing method. Lynne visits the hospital where her physical therapist’s office is located. She receives 31 minutes of therapeutic exercise and 14 minutes of manual therapy.
What is the 8 minute rule in nursing?
What is the 8 minute rule? The 8 minute rule is a Medicare guideline for determining how many billable units may be charged in rehabilitation based on time spent with the patient. Billable units are based on 15 minute increments, once the initial 8 minutes have been met, which is how the name “8 minute rule” developed.
How do you calculate the 8 minute rule in medical billing?
Per the 8-Minute Rule, you would first calculate the total treatment time: 30 min + 15 min + 8 min + 30 min = 83 total minutes According to the 8 minute rule chart, you could bill a maximum of 6 units. However, in this case, when adding up your direct time (time-based) codes, it equals 53 minutes.

Does Medicare follow the 8-minute rule?
The 8-minute rule states that to receive Medicare reimbursement, you must provide treatment for at least eight minutes. Using the “rule of eights,” billing units that are normally based on 15-minute increments spent with a patient can be standardized.
What is the 8-minute rule and how is the time billed for two units?
Introduced in December 1999, the 8-minute rule became effective on April 1, 2000. The rule allows practitioners to bill Medicare for one unit of service if its length is at least eight (but fewer than 22) minutes. A billable “unit” of service refers to the time interval for the service.
How many minutes is 8 units?
22 minutesMinutes and Billing Units8 – 22 minutes1 unit23 – 37 minutes2 units38 – 52 minutes3 units53 – 67 minutes4 units68 – 82 minutes5 units1 more row•Sep 13, 2018
What is the rule of 8s?
Enter the 8-Minute Rule If eight or more minutes are left over, you can bill for one more unit; if seven or fewer minutes remain, you cannot bill an additional unit.
Can you bill 3 units in 30 minutes?
According to the chart you can bill 3 units again based on total time. Your bill would need to have 2 units of therapeutic exercises which equals 30 minutes with 2 minutes remainder.
Can a therapist bill Medicare Part B for treating more than one patient at the same time?
Therapists, or therapy assistants, working together as a "team" to treat one or more patients cannot each bill separately for the same or different service provided at the same time to the same patient. CPT codes are used for billing the services of one therapist or therapy assistant.
What is the 8 minute rule in therapy?
A therapist must provide direct one-to-one therapy for at least 8 minutes to receive reimbursement for a time based treatment code. When only one service is provided in a day, you shouldn't bill for services performed for less than 8 minutes.
How do you calculate minute units?
There are 60 minutes in 1 hour. To convert from minutes to hours, divide the number of minutes by 60. For example, 120 minutes equals 2 hours because 120/60=2.
What is the CPT time rule?
The CPT midpoint rule, which says that “a unit of time is attained when the midpoint is passed,” applies to codes that specify a time basis for code selection. Though not accepted by all payers, even Medicare allows the midpoint rule for some services.
How do you bill therapy minutes?
They should add up the total time spent on all short treatments. For example, if the treatments each add up to 5, 6, and 7 Minutes, one unit may be billed for the service that was 7 minutes long. Although the total number of minutes adds up to 18, they still only get to bill for one unit.
What is the difference between Rule of 8?
Divisibility Rule of 8 If the last three digits of a number are divisible by 8, then the number is completely divisible by 8. Example: Take number 24344. Consider the last two digits i.e. 344. As 344 is divisible by 8, the original number 24344 is also divisible by 8.
How many therapy units is 45 minutes?
3 billable unitsTimed Minutes: 45 However, billing is based ultimately on total timed minutes – 45 in this case, and equivalent to 3 billable units. Those 7 minutes spent on therapeutic activity still count toward timed minutes because Therapeutic Activity is a timed code.
What is the 8 minute rule for Medicare?
All federally funded plans—including Medicare, Medicaid, TriCare, and CHAMPUS—require use of the 8-Minute Rule, as do some commercial payers. To determine the requirements for individual payers, it’s best to contact the payer directly.
How long should I bill Medicare?
The answer depends on the billing guidelines you’re using. Per Medicare, as long as the sum of your remainders is at least eight minutes , you should bill for the individual service with the biggest time total, even if that total is less than eight minutes on its own.
How many minutes of therapy should a rehab therapist be on Medicare?
The 8-Minute Rule governs the process by which rehab therapists determine how many units they should bill to Medicare for the outpatient therapy services they provide on a particular date of service (extra emphasis on the word “Medicare” as this rule does not apply to other insurances unless they have specified that they follow Medicare billing guidelines). Basically, a therapist must provide direct, one-on-one therapy for at least eight minutes to receive reimbursement for a time-based treatment code. It might sound simple enough, but things get a little hairy when you bill both time-based and service-based codes for a single patient visit—and therein lies the key to correctly applying this rule.
How long is a CPT code?
According to CPT guidelines, each timed code represents 15 minutes of treatment. But your treatment time for these codes won’t always divide into perfect 15-minute blocks. What if you only provide ultrasound for 11 minutes? Or manual therapy for 6 minutes? That’s where the 8-Minute Rule comes in: Per Medicare rules, in order to bill one unit of a timed CPT code, you must perform the associated modality for at least 8 minutes. In other words, Medicare adds up the total minutes of skilled, one-on-one therapy (direct time) and divides the resulting sum by 15. If eight or more minutes are left over, you can bill for an additional unit. But if seven or fewer minutes remain, Medicare will not reimburse you for another full unit, and you must essentially drop the remainder. To give a simple example, if you performed manual therapy for 15 minutes and ultrasound for 8 minutes, you could bill two direct time units.
How long is 15+8+10?
To start, let’s add up the total treatment time: 15+8+8+10 = 41 minutes. According to the chart above, the maximum total codes you can bill for 41 minutes is 3. Now, let’s take the total minutes of constant attendance services: 15+8+8 = 31. Then, divide that number by 15. You get two 15-minute services plus one extra minute.
How many minutes are required for a federally funded program?
Federally funded programs use the 8-Minute Rule. For others, your best bet is to ask. If the insurance company doesn’t have a preference, you may want to calculate your units using both methods to determine which will better serve your practice.
How long does an insurance provider have to charge for a unit of service?
However, it’s important to understand that there are insurers who don’t require providers to adhere to the 8-Minute Rule. As this resource points out, under the Substantial Portion Methodology (SPM), there is no cumulation of minutes or remainders; in order to charge for a unit of service, you must have performed that service for a “substantial portion” of 15 minutes (i.e., at least 8 minutes). That means that if your leftover minutes come from a combination of services, you cannot bill for any of them unless one individual service totals at least eight minutes.
Medicare 8-Minute Rule Explained
The 8-Minute Rule has been in effect since April 1, 2000, and it applies to time-based current procedural codes for outpatient services.
Getting Supplemental Medicare To Cover for You
The 8-Minute Rule can be a bit confusing and strange for beneficiaries who aren’t used to dealing with it. But it benefits Medicare recipients to understand how their coverage is billed for direct contact services like physical therapy.
What is the 8 minute rule for rehab?
Rehab therapists use the 8-Minute Rule—or the slightly variant “Rule of Eights”—to determine the number of units they should bill Medicare for the therapy services provided on a particular date of service. Prev.
How many minutes of treatment do you need to be on Medicare?
For time-based codes, you must provide direct treatment for at least eight minutes in order to receive reimbursement from Medicare. Basically, when calculating the number of billable units for a particular date of service, Medicare adds up the total minutes of skilled, one-on-one therapy and divides that total by 15. If eight or more minutes are left over, you can bill for one more unit; if seven or fewer minutes remain, you cannot bill an additional unit.
What is the rule of 8?
The Rule of Eights—which can be found in the CPT code manual and is sometimes referred to as the AMA 8-Minute Rule—is a slight variant of CMS’s 8-Minute Rule . The Rule of Eights still counts billable units in 15-minute increments, but instead of combining the time from multiple units, the rule is applied separately to each unique timed service. Therefore, the math is also applied separately. (Keep in mind that the Rule of Eights only applies to timed codes that have 15 minutes listed as the “usual time” in the operational definition of the code.)
How long do you have to be on Medicare for a treatment?
For time-based codes, you must provide direct treatment for at least eight minutes in order to receive reimbursement from Medicare. Basically, when calculating the number of billable units for a particular date of service, Medicare adds up the total minutes of skilled, one-on-one therapy and divides that total by 15.
How many minutes of 97110 are in a single visit?
For example, say a therapist bills 10 minutes of 97110 and 10 minutes of 98116 in a single visit. Those codes are considered unique services, and are counted separately. Each service lasted longer than eight minutes, so the therapist can bill for two units total: one unit of 97110 and one unit of 98116.
What are the codes for a therapist?
Time-based (or constant attendance) codes, on the other hand, allow for variable billing in 15-minute increments. You would use these codes for performing one-on-one services such as: 1 therapeutic exercise (97110) 2 therapeutic activities (97530) 3 manual therapy (97140) 4 neuromuscular re-education (97112) 5 gait training (97116) 6 ultrasound (97035) 7 iontophoresis (97033) 8 electrical stimulation (manual) (97032)
How long is a manual therapy session?
Let’s say that on a single date of service, you perform 30 minutes of therapeutic exercise (EX), 15 minutes of manual therapy (MT), 8 minutes of ultrasound (US), and 15 minutes of electrical stimulation unattended (ESUN). To correctly calculate the charge in accordance with the 8-Minute Rule, you would add the constant attendance procedures ...
What is the 8 minute rule?
By definition, the 8-minute rule applies to Medicare, Medicaid, TRICARE, and CHAMPUS. Private insurance carriers may choose to operate the same way, but by rule are not required to. Medicare beneficiaries who enroll in private Medicare plans (Medicare Advantage) may also have different billing standards depending on the plan.
How many units of Medicare would you be billed for if you completed 23 minutes of treatment?
However, if you completed 23 minutes of treatment, Medicare would be billed for two units of treatment. The bill would still be for two units regardless of whether you spent 23 or 30 minutes with the patient.
How long do you have to be on Medicare for treatment?
The 8-minute rule states that to receive Medicare reimbursement, you must provide treatment for at least eight minutes. Using the “rule of eights,” billing units that are normally based on 15-minute increments spent with a patient can be standardized.
How long does Medicare bill for physical therapy?
Understanding the Medicare 8-Minute Rule for Physical Therapy Billing. Medicare has certain rules and regulations in place to prevent fraud, waste, and abuse. Here’s one you may not have heard of – the 8-minute rule. Providers must treat patients for at least eight minutes to receive Medicare reimbursement.
How many minutes of manual therapy are there on Medicare?
However, you have two “remaining” minutes from the physical exercise and six “remaining” minutes from the manual therapy. Together, you have eight minutes, which would push you into the next billing unit. Medicare guidelines would allow you to bill for three units in that circumstance.
How many billing units can you bill for 45 minutes?
Technically, you’ve just spent 45 minutes with the patient, which would equate to three billing units. However, those first 25 minutes only counted for one unit because you were not in the room for the whole time, and you were not performing one undivided task. Therefore, you can only bill for two units.
How long do you have to bill for a 15 minute unit?
You only have to spend eight minutes with a patient to be able to bill for one “15-minute” unit. However, if you spend 16 minutes with a patient, you’ll still only be able to bill for one unit. You’d have to spend 23 minutes (15 + 8) with a patient to be able to fall into the two-unit bracket.
The Fundamentals of the 8-Minute Rule
The 8-Minute rule controls how rehab therapists decide how many units they should charge to Medicare for outpatient therapy services provided on a specific date. To be reimbursed for a time-based treatment code, a therapist must perform direct, one-on-one therapy for at least eight minutes.
What Exactly Is the 8-Minute Rule?
Medicare’s 8-minute rule states that you can bill Medicare for one entire unit if a service takes between 8 and 22 minutes. As a result, this can only apply to CPT codes that are time-based. The 8-minute guideline, however, does not apply to all time-based CPT codes or all situations.
What Is a Timed Code?
In the AMA CPT codebook, time-based codes are described as services provided one-on-one in 15-minute blocks of time, e.g., To 1 unit = 15 minutes. When assessing the number of units billed for a visit, the 8-minute rule comes into play.
What Are CPT Time-Based Codes?
Variable billing in 15-minute increments is possible using time-based codes. These codes provide one-on-one services such as:
What Is an Untimed Code?
Untimed codes, also known as service-based CPT codes, have no time restriction in their definition and are usually given to a patient once per day. Physical Therapy Evaluation (97161), Mechanical Traction (97012), or Electrical Stim, unsupervised are examples of these codes (97014).
Bottom Line
We hope that the following information clears up any misunderstandings you may have about the 8-minute rule. There is nothing that you should be afraid of when it comes to Medicare’s 8-minute rule. You can avoid overbilling or underbilling by having explicit knowledge of what the rule implies.
What is the 8 minute rule?
The 8 minute rule is a Medicare guideline for determining how many billable units may be charged in rehabilitation based on time spent with the patient. Billable units are based on 15 minute increments, once the initial 8 minutes have been met, which is how the name “8 minute rule” developed.
How long is a 15 minute block?
Within a 15-minute block of time, you cross the half-way point at 8 minutes…well, technically, 7 minutes and 30 seconds. Think of 8 minutes as the tipping point. Once you’ve crossed 8 minutes, the 15 minute block counts as a unit! By spending at least 8 minutes with your patient, you’ll “satisfy” the majority of the 15-minute block ...
How long is a CPT unit?
According to the CMS (Centers for Medicare and Medicaid Services), billable units are 15 minutes long. That means Medicare will reimburse a treatment based on how many of these 15-minute increments or billable units it entailed. “For any single timed CPT code in the same day measured in 15-minute units, providers bill a single 15-minute unit ...
Why do 7 minutes count as timed minutes?
Those 7 minutes spent on therapeutic activity still count toward timed minutes because Therapeutic Activity is a timed code. Therefore, the therapist can ethically bill 2 units of neuromuscular re-ed because neuro re-ed was a larger focus of the treatment in terms of minutes spent.
How long is a 15 minute treatment?
CMS qualifies the 15-minute rule as any treatment “ greater than or equal to 8 minutes through and including 22 minutes.”. So if your treatment was 20 minutes, you only have one unit to bill. This works incrementally as you accumulate units:
Is 8 minutes a timed CPT?
Remember: the 8-minute rule only counts for “timed” minutes, regardless of the total treatment time (which may include “untimed” minutes such as hot/cold packs). So which CPT codes are “timed” and which are “untimed”?

The Basics
Time-Based vs. Service-Based
Minutes and Billing Units
What Are Mixed Reminders?
What About Non-Medicare Insurances?
to Bill Or Not to Bill?
The 8-Minute Rule in WebPT
8-Minute Rule FAQ
- What is the 8-Minute Rule?
Put simply, to receive payment from Medicare for a time-based (or constant attendance) CPT code, a therapist must provide direct treatment for at least eight minutes. To calculate the number of billable units for a date of service, providers must add up the total minutes of skilled, one-on-o… - What are time-based CPT codes?
Time-based (or constant attendance) codes allow for variable billing in 15-minute increments. These differ from service-based (or untimed) codes, which providers can only bill once regardless of how long they spend providing a particular treatment.
Introduction
- The 8-Minute Rule applies to services where the beneficiary and the healthcare provider have direct contact. This means it must be an in-person visit. Medicare will be billed based on the total number of minutes timed per regulation but won’t be billed if the individual service is less than 8 minutes. Services are billed in 15-minute increments. If...
What Are Service-Based Cpt Codes?
What Are Time-Based Cpt Codes?
What’s The Deal with Mixed Remainders?
So What Is The Rule of Eights?
Does Assessment and Management Time Count Toward The 8-Minute Rule?
What’s The Best Way to Avoid 8-Minute Rule Mistakes?