All three of Aetna’s plans include a zero deductible and minimal copay for tier 1 generic drugs from a preferred pharmacy (Walmart, Costco, King Soopers, Safeway, and CVS). Initial coverage limits and annual out-of-pocket threshold amounts are the same for all three plans.
Full Answer
What medications are covered by Aetna?
prescription drugs and over-the-counter drugs and items are covered by Aetna Better Health Premier Plan. The Drug List also tells you if there are any special rules or restrictions on any drugs covered by Aetna Better Health Premier Plan. Key terms and their definitions appear in the last chapter of the .
What is the preferred pharmacy for Aetna?
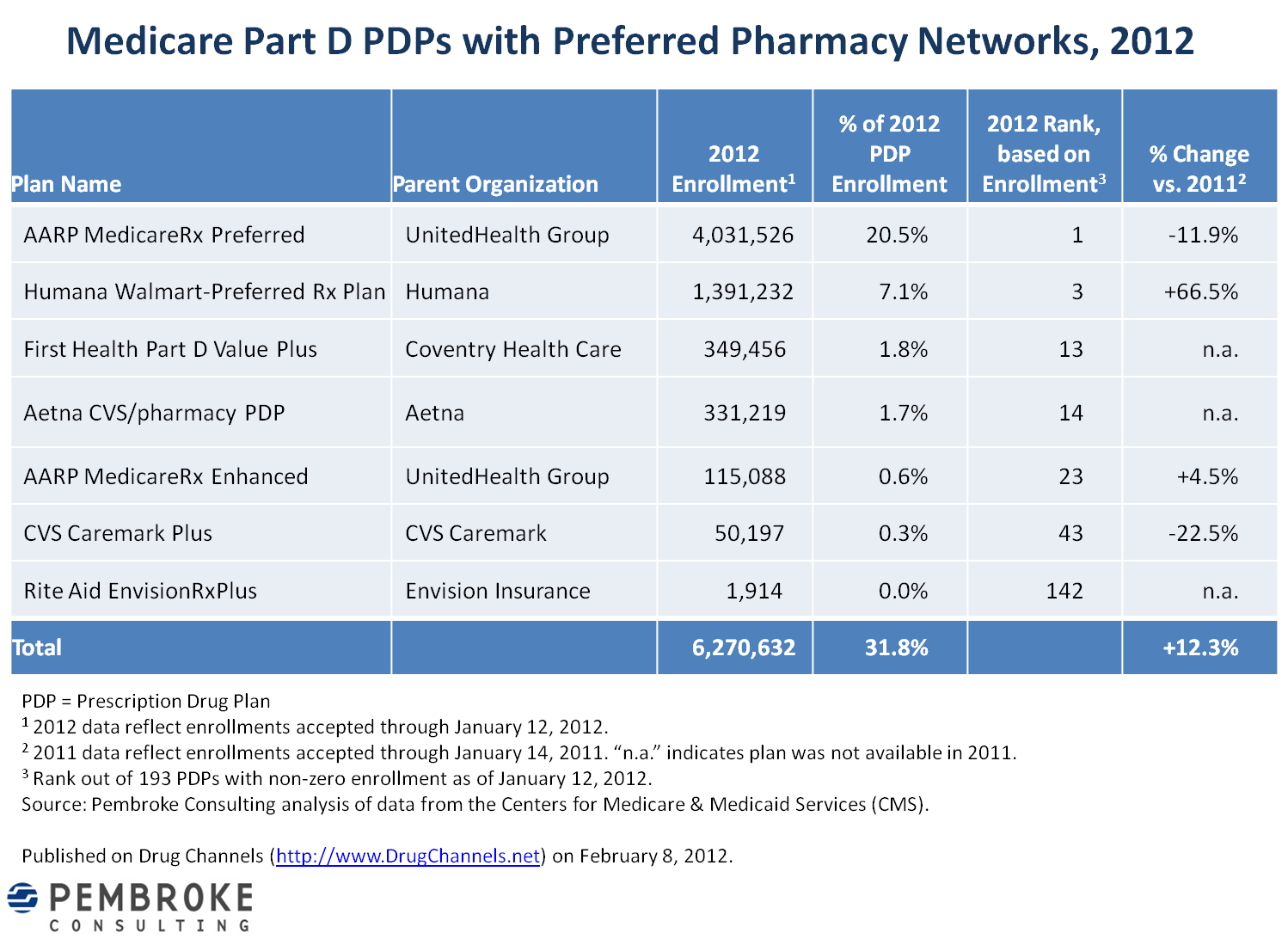
The plan’s preferred pharmacy network comprises 4,200 Walmart, 580 Sam’s Club and 7,500 CVS/pharmacy locations. In addition to the preferred pharmacy network, members also can use any of the 52,700 pharmacies in the Aetna Medicare network.
What insurances does Aetna offer?
Most of the U.S. Aetna does offer Life Insurance. However, on their website, Aetna states that the Life insurance coverage that they offer is available through employer-provided plans only. Their life insurance policies are not available to individuals for private sales. Aetna life insurance plans are called group term insurance or group coverage.
Does Aetna have a Medicare Advantage plan?
Depending on where you live, you may be able to enroll in one of the following types of Aetna Medicare Advantage plans: Aetna Medicare Advantage HMO (Health Maintenance Organization) plans may have lower costs than other types of Medicare Advantage plans because they use a contracted provider network to keep health-care expenses low.

Is Walgreens a preferred pharmacy for Medicare?
Walgreens will continue to be a part of preferred pharmacy networks with three national Medicare Part D plan sponsors: Humana. UnitedHealthcare.
What is the difference between standard and preferred pharmacy?
When your pharmacy is a 'Preferred Pharmacy', you get lower pricing and often are allowed to get 90 day supplies of your medications. When your pharmacy is a 'Standard Pharmacy' the pricing will be higher for you on each and every prescription. You also may not be allowed to get 90 day supplies of your medications.
Can I use Aetna at Walmart?
Aetna Medicare members can continue to receive their medicines at Walmart or at any of our 65,000+ network pharmacies nationwide.
What does preferred pharmacy mean?
In the United States, a preferred pharmacy network is a group of pharmacies that involves a prescription drug plan that selects a group of preferred pharmacies, which likely include pharmacies willing to give the plans a larger discount than other pharmacies.
What generic drugs are preferred?
Your preferred drug list, sometimes called a formulary, is a list of brand-name and generic medications that are preferred by your plan. These medications are selected because they can safely and effectively treat most medical conditions while helping to contain costs for you and your plan.
What is an example of a non preferred pharmacy?
"Standard" (non-preferred) retail pharmacies, "Preferred" mail-order pharmacies, and. "Standard" (non-preferred) mail-order pharmacies.
Can Aetna force you to use CVS?
CVS/Aetna can't force patients to fill prescriptions at CVS pharmacies. CVS must disclose how much in rebates it receives from drug manufacturers and how much of that money it pockets.
What Medicare Part D plans Does Walmart accept?
Like all Medicare Part D plans, the Humana Walmart Value Rx Plan (PDP) is available to people who get benefits through Original Medicare, a Medicare Private Fee-for-Service Plan with no drug benefit, a Medicare Cost Plan or a Medicare Medical Savings Account Plan.
Does Aetna have a separate prescription card?
The Aetna Rx Discount Network Pharmacy Card provides access to discounts on prescription drugs and does not provide prescription drug benefits, nor is it intended to replace prescription drug benefits obtained through participation in insurance plans or an employer or retiree plan.
What is the difference between preferred and standard?
That means the younger and healthier you are, the cheaper your rates will be. Preferred rates are the lowest available and bestowed upon people in the optimum health. Everyone else falls into the “standard' rate category.
Is Costco a preferred pharmacy?
First and foremost, Costco Pharmacy is open to anybody where required by law. In practice, that means in most states. So you don't usually have to be a member to use the Costco pharmacy. In an era of skyrocketing prescription costs, Costco routinely has low prices on medications.
Does Medicare use a specialty pharmacy?
As a Medicare Part D member, with access to our large pharmacy network, you may fill your specialty medication at any pharmacy that is able to obtain the drug. Specialty pharmacies work exclusively with handling and administering complex specialty medications.
Why do we call them network pharmacies?
We call them network pharmacies because we’ve contracted with them to provide prescription drugs to Aetna Medicare plan members. In most cases, your prescriptions are covered under our plan only if they’re filled either: By a network pharmacy. Through our mail‐order pharmacy service. Once you go to a pharmacy, you’re not required to keep using ...
How long does it take to get a prescription from mail order?
You should expect to get your prescription drugs 7 to 14 business days from the time the mail‐order pharmacy receives the order. If you don’t receive your prescription drug (s) within this time frame, please call us at the number on your ID card. You may have the option to sign up for automated mail‐order delivery.
Does preferred cost sharing save money?
Preferred cost sharing may save you money . You can go to any of the pharmacies on this list. However, your costs for some drugs may be lower at pharmacies on this list that offer preferred cost sharing. We have marked these pharmacies with an orange tag.
Can I use the same pharmacy for my prescription?
Once you go to a pharmacy, you’re not required to keep using the same pharmacy to fill your prescriptions. You can switch to any of our other network pharmacies. We’ll fill prescriptions at non-network pharmacies under certain circumstances. See those circumstances in the Evidence of Coverage.
Check our drug list
Search our formulary for covered drugs and get the information you need. It shows the drugs we cover, the tier a drug is on, any limits or requirements and mail order availability. Generally, the lower the tier, the less you pay. Your Summary of Benefits tells you the drug costs for tiers.
Get our full drug list and more
See a complete list of our covered drugs and other important prescription drug information.
Find a drug by name
Search for a specific drug by name and see if generic equivalents are available. Enter your ZIP code to get started.
What is the Medicare Plan Finder?
The Medicare Plan Finder is a useful comparison tool you can use to plug in the names of prescription drugs and find plans in your area that will cover them. View the Medicare Plan Finder.
How many drugs are on the formulary for Medicare?
Medicare mandates that there be at least two drugs from every therapeutic class in a formulary. But in some instances, you may need a drug that just doesn’t make the list. If that happens, your doctor can contact the insurance company to request what’s called a “formulary exception.”.
How many people over 65 take prescriptions?
Forty percent of those over 65 take five or more medications a day. 1 It’s a staggering number, but it underscores the necessity of prescription drug insurance coverage. That’s why almost 74 percent of people who are on Medicare — or nearly 44 million people 2 — are enrolled in a prescription drug plan. As you figure out the best plan ...
What tier is a drug approved?
Typically, if the drug is approved, it will be provided to you at the cost found in one of the top tiers, such as tier 4 or 5 , which means you will usually be responsible for a higher percentage of the cost than if the medicine was in a lower tier. Transcript: Understanding Drug Payment Stages Infographic.
Does Medicare cover formulary?
Every Medicare prescription drug plan has a list of drugs — also known as a formulary — that it agrees to cover. When you research a plan, check your list of medications against the prescription drugs on your plan’s list. You’ll also be able to see which "tier" it’s been placed into.
Does Medicare Part D cover prescriptions?
Medicare Part D, also known as a prescription drug plan, helps you pay for most of your prescribed medicine. Generally, Original Medicare does not include prescription drug coverage. Learn more here about the different parts of Medicare.
Do you need a pharmacy to take a drug?
Generally, you need to use a pharmacy in your plan’s network for the medication to be covered . Some plans have preferred pharmacies where you could save even more. Whether the drug you take is on the formulary (list of covered drugs). Generally, plans will only cover medications if the drug is on their formulary.
Formularies include both brand name and generic drugs. What are the basic differences between brand name and generic drugs? How can members know which to choose?
McKenna: Think of the brand name drug as the innovator. It’s often the first version of a drug. For a certain period of time, the company that developed the innovative drug is the only one that can make it.
What can members do to save on prescription drug costs?
McKenna: Oftentimes, members experience sticker shock when it comes to what they pay for a drug. So I think it’s important to have a conversation with your pharmacist. Say, ‘This is more than I'm expecting to spend.
What do you think members can do to build a stronger relationship with their pharmacist?
McKenna: I think people should ask their pharmacist any questions they might have about their medications, whether that’s how their medicine works or how much it costs. You should also talk to your pharmacist if you're having problems remembering to take your medicine or are experiencing unexpected side effects.
Secure and safe medicines by mail
It's important to take your prescription medicines regularly. You can receive 90-day supplies of many drugs by mail, saving you trips to the drug store and missed doses. With your secure Caremark account you have access to:
We offer three easy ways to start delivery by mail
1. Ask your doctor to electronically prescribe your medicines to CVS Caremark Mail Service Pharmacy, NPI 1881952851. Your prescription will be delivered immediately.
Disclaimer
The typical number of business days after the mail order pharmacy receives an order for you to receive your shipment is up to 10 days. Enrollees have the option to sign up for automated mail order delivery. If your mail order drugs do not arrive within the estimated time frame, please contact us toll free at 1-866-235-5660, (TTY: 711).
Lower your out-of-pocket costs
Here are some tips to help you get the most from your Part D prescription drug coverage and lower your costs:
Save at preferred pharmacies
Preferred pharmacies generally offer lower costs to you on some medicines. There are thousands of locations nationally in our preferred pharmacy networks. Use the Pharmacy Locator tool on AetnaMedicare.com to find preferred pharmacies near you. You can also call the number on your member ID for help.
Consider lower-priced medicines
Our drug lists include thousands of drugs. In some cases, there may be a less expensive brand or generic drug than the one you currently take for your condition. Generic drugs have the same active ingredients in the same strength as their corresponding brand-name drug. But they can cost a lot less. Discuss your treatment options with your doctor.
FAQs
What should I do if there are no preferred pharmacy locations in my area?
Disclaimer
The typical number of business days after the mail order pharmacy receives an order for you to receive your shipment is up to 10 days. Enrollees have the option to sign up for automated mail order delivery.