Average Cost of Medicare Advantage Plans in Each State
| State | Monthly Premium | Prescription Drug Deductible |
| Alabama | $65 | $257 |
| Alaska | N/A | N/A |
| Arizona | $48 | $322 |
| Arkansas | $45 | $323 |
Does Medicare Advantage have deductible?
51 rows · Aug 10, 2021 · The average monthly premium for Medicare Advantage plans ranges from $38 to $105 across the ...
What do you pay in a Medicare Advantage plan?
Feb 15, 2022 · In 2022, the average Part D deductible is $367.80 for the year. 1 Medicare Part D “donut hole” coverage gap costs Medicare Part D prescription drug plans and some Medicare Advantage plans have what is known as a “donut hole” or “coverage gap,” which is a temporary limit on how much a Prescription Drug Plan will pay for prescription drug costs.
How much does Medicare Advantage plan cost?
Many Medicare Advantage Plans have a $0 premium. If you enroll in a plan that does charge a premium, you pay this in addition to the Part B premium (and the Part A premium if you don't have premium-free Part A). ... Whether the plan has a yearly deductible [glossary] or any additional deductibles. How much you pay for each visit or service ...
Is there a copay with Medicare?
Dec 14, 2021 · Medicare Advantage plans that include prescription drug coverage will often have two separate deductibles, one for medical care and another for prescription drug costs. Medicare Part D Deductible. Medicare Part D plans cover prescription medications. Like Medicare Advantage, plans Medicare Part D plans are sold by private insurers and thus there is no …
What is the Medicare standard plan annual deductible for 2021?
$203 inThe standard monthly premium for Medicare Part B enrollees will be $148.50 for 2021, an increase of $3.90 from $144.60 in 2020. The annual deductible for all Medicare Part B beneficiaries is $203 in 2021, an increase of $5 from the annual deductible of $198 in 2020.Nov 6, 2020
Is there a high deductible Medicare Advantage plan?
Medicare MSA Plans combine a high-deductible insurance plan with a medical savings account that you can use to pay for your health care costs. Most Medicare Advantage Plans offer prescription drug coverage.
What is the deductible for plan G in 2021?
$2,370Effective January 1, 2021, the annual deductible amount for these three plans is $2,370. The deductible amount for the high deductible version of plans G, F and J represents the annual out-of-pocket expenses (excluding premiums) that a beneficiary must pay before these policies begin paying benefits.
What is the biggest disadvantage of Medicare Advantage?
The primary advantage is the monthly premium, which is generally lower than Medigap plans. The top disadvantages are that you must use provider networks and the copays can nickel and dime you to death.Dec 12, 2021
How much is Medicare Part A deductible for 2021?
The Part A deductible is $1,484 per benefit period in 2021.
What is the average Medicare premium for 2021?
In 2021, the average monthly premium for Medicare Advantage plans with prescription drug coverage is $33.57 per month. 1. Depending on your location, $0 premium plans may be available in your area. Medicare Part C, also known as Medicare Advantage, is sold by private insurance companies.
What is Medicare Part A?
Medicare Part A is hospital insurance. It covers some of your costs when you are admitted for inpatient care at a hospital, skilled nursing facility and some other types of inpatient facilities. Part A can include a number of costs, including premiums, a deductible and coinsurance.
How much is respite care in 2021?
You might also be charged a 5 percent coinsurance for inpatient respite care costs. Medicare Part A requires a coinsurance payment of $185.50 per day in 2021 for inpatient skilled nursing facility stays longer than 20 days. You are responsible for all costs after day 101 of an inpatient skilled nursing facility stay.
How many different Medigap plans are there?
There are 10 different Medigap plans available in most states. You can use the chart below to compare the costs that each type of Medigap plan may cover. Medigap plans and Medicare Advantage plans are not the same thing. You cannot have a Medigap plan and Medicare Advantage plan at the same time.
How long do you have to work to get Medicare in 2021?
To qualify for premium-free Part A, you or your spouse must have worked and paid Medicare taxes for the equivalent of 10 years (40 quarters).
What is the late enrollment penalty for Medicare?
The Part B late enrollment penalty is as much as 10 percent of the Part B premium for each 12-month period that you were eligible to enroll but did not.
What is Medicare Advantage Plan?
Medicare Advantage Plan (Part C) A type of Medicare health plan offered by a private company that contracts with Medicare. Medicare Advantage Plans provide all of your Part A and Part B benefits, excluding hospice. Medicare Advantage Plans include: Health Maintenance Organizations. Preferred Provider Organizations.
What is Medicare premium?
premium. The periodic payment to Medicare, an insurance company, or a health care plan for health or prescription drug coverage. . Many Medicare Advantage Plans have a $0 premium. If you enroll in a plan that does charge a premium, you pay this in addition to the Part B premium. Whether the plan pays any of your monthly.
What is out of network Medicare?
out-of-network. A benefit that may be provided by your Medicare Advantage plan. Generally, this benefit gives you the choice to get plan services from outside of the plan's network of health care providers. In some cases, your out-of-pocket costs may be higher for an out-of-network benefit. .
What is the difference between Medicare and Original Medicare?
Original Medicare. Original Medicare is a fee-for-service health plan that has two parts: Part A (Hospital Insurance) and Part B (Medical Insurance). After you pay a deductible, Medicare pays its share of the Medicare-approved amount, and you pay your share (coinsurance and deductibles). .
What is a medicaid?
Whether you have. Medicaid. A joint federal and state program that helps with medical costs for some people with limited income and resources. Medicaid programs vary from state to state, but most health care costs are covered if you qualify for both Medicare and Medicaid.
What is covered benefits?
benefits. The health care items or services covered under a health insurance plan. Covered benefits and excluded services are defined in the health insurance plan's coverage documents. and if the plan charges for it. The plan's yearly limit on your out-of-pocket costs for all medical services. Whether you have.
What is a copayment?
A copayment is usually a set amount, rather than a percentage. For example, you might pay $10 or $20 for a doctor's visit or prescription drug. An amount you may be required to pay as your share of the cost for services after you pay any deductibles. Coinsurance is usually a percentage (for example, 20%).
What Is a Deductible?
A deductible is the amount of money that you must pay out of your own pocket for covered care before your plan coverage kicks in.
Medicare Part A Deductible
Medicare Part A covers inpatient care received at a hospital, skilled nursing facility or other inpatient facility.
What Is the Maximum Cost of Medicare Part B?
Medicare Part B does come with a premium cost. The monthly premium prices are set annually and depend on your annual income. Premium costs start at $170.10 per month. The maximum cost of Medicare Part B premiums is $578.30 per month in 2022, and that's for individuals reporting half a million dollars or more in income in 2020.
Medicare Part C (Medicare Advantage) Deductible
Medicare Part C plans, otherwise known as Medicare Advantage plans, are an alternative way to get Original Medicare benefits, often with additional coverage.
Medicare Part D Deductible
Medicare Part D plans cover prescription medications. Like Medicare Advantage, plans Medicare Part D plans are sold by private insurers and thus there is no standard deductible.
Medicare Supplement Deductibles by Plan
There are 10 standardized Medicare Supplement plans (also called Medigap) available in most states, and two of those plans offer a high-deductible option. Medigap Plan F and Plan G have high-deductible options that include an annual deductible of $2,490 in 2022.
What is a deductible for Medicare?
A deductible is the amount you must pay out of pocket for health care before your plan begins to pay. For example, if your deductible is $1,000, you could pay $1,000 out of pocket before you plan begins to cover your health care costs. Some Medicare Advantage plans have $0 annual deductibles.
What is Medicare Advantage Plan Premium?
Medicare Advantage plans out of pocket cost: Premium. A premium is the amount you pay monthly or annually to have the plan, whether or not you receive services. Some Medicare Advantage plans have premiums as low as $0 but you must continue to pay your Medicare Part B premium.
What is Medicare Advantage?
Medicare Advantage plans are another way to get your Medicare Part A and Part B benefits from a private insurance company contracted with Medicare. Medicare Advantage plans must cover everything that Original Medicare (Part A and Part B) cover with the exception of hospice care, which is still covered by Part A.
What factors affect how much you pay out of pocket?
Other factors that could affect how much you pay out of pocket are: Whether you go out of network to get care. Whether you need extra benefits. Whether your doctor accepts Medicare assignment if you do go out of network. Whether you have Medicaid or other financial help. What the plan’s yearly out of pocket limit is.
What is coinsurance and copayment?
Coinsurance and copayment is the amount you pay every time you see a doctor or use a service. Coinsurance is usually a percentage and a copayment is a set dollar amount. For example, you could pay a $15 copayment every time you visit the doctor.
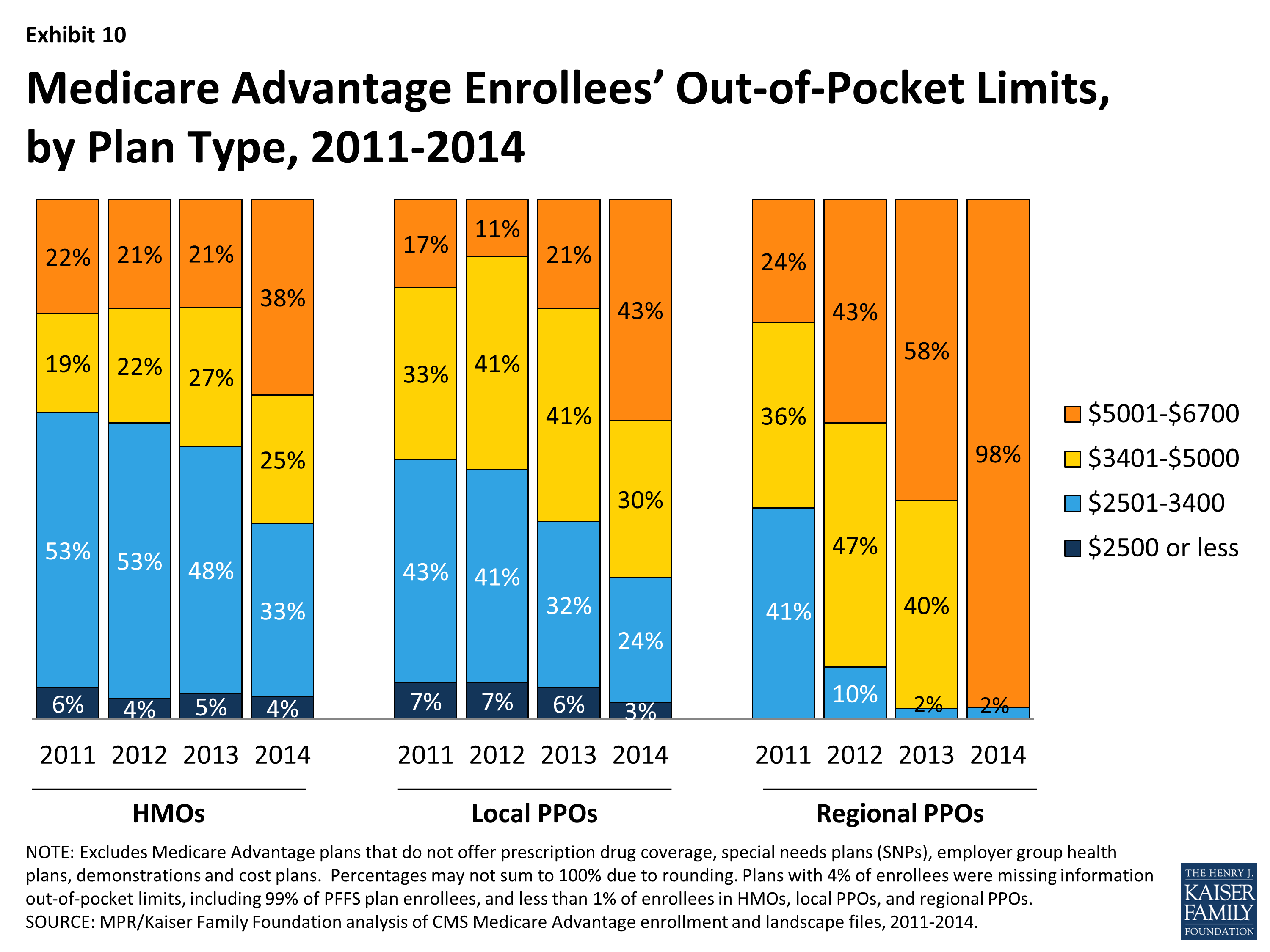
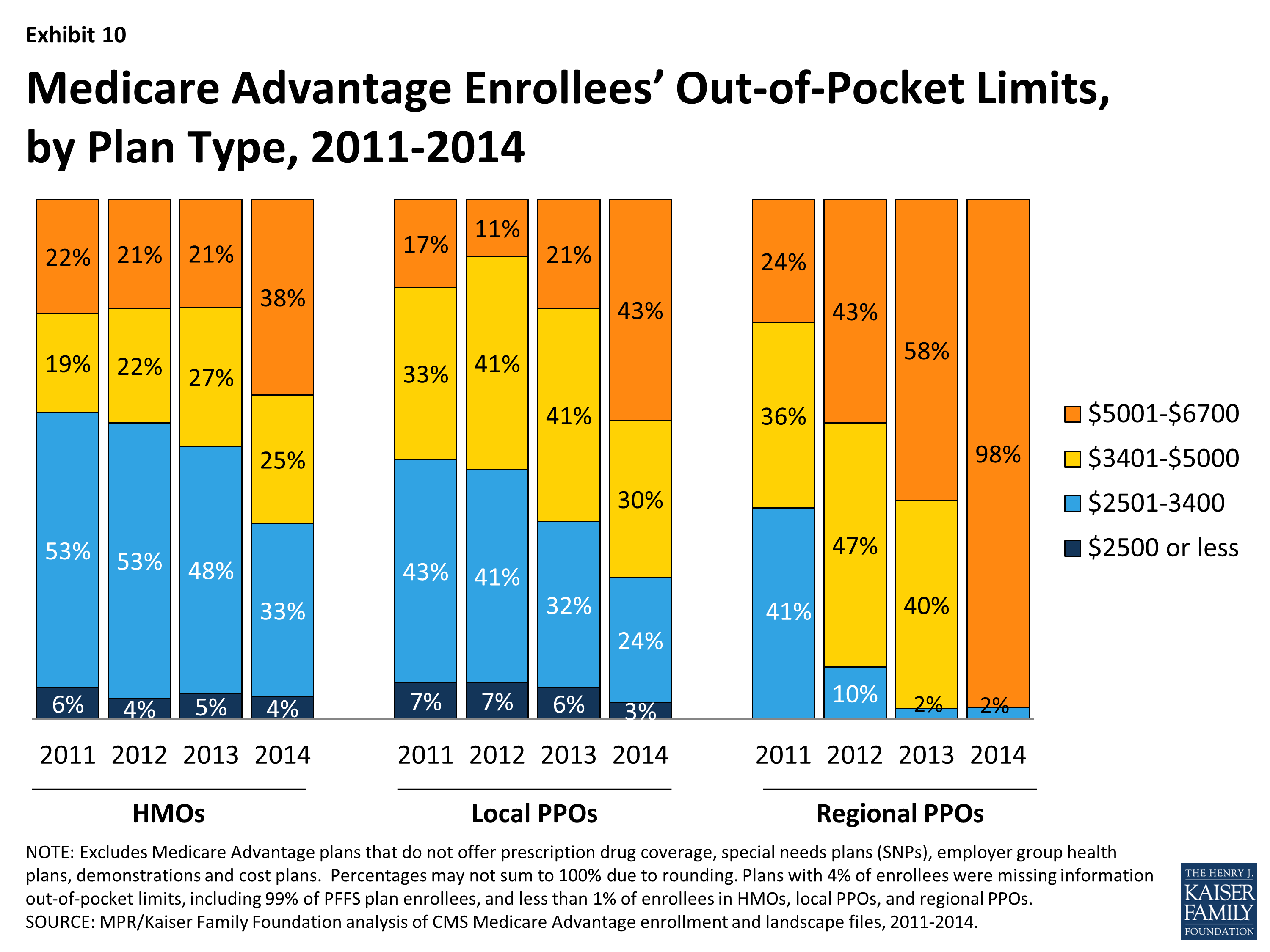
Does Medicare Advantage have out of pocket limits?
Unlike Original Medicare, Medicare Advantage plans have out of pocket limits, capping what you spend yearly on covered medical services. Medicare Advantage plans may save you money overall but they also generally come with some out of pocket costs. Medicare Advantage plans out of pocket costs include: premiums, deductibles. coinsurance/copayments.
What is the deductible for Medicare?
Each part of Medicare carries its own deductible. The Part A and Part B deductibles are standard for each beneficiary of Original Medicare. The Part C (Medicare Advantage) and Part D (prescription drug plan) deductibles will vary from plan to plan. Some Part C and Part D plans may have a $0 deductible. Some Medicare Advantage plans also feature $0 ...
How much is Medicare Part B deductible in 2021?
The Medicare Part B deductible in 2021 is $203 per year, and the Part A deductible is $1,484 per benefit period. Learn more about these costs and what you can expect.
How much is Medicare Part A 2021?
The Medicare Part A deductible for 2021 is $1,484 per benefit period . Unlike the deductible for Part B that operates on an annual basis, the Part A deductible starts and stops with each benefit period. A benefit period begins the day you are admitted for inpatient care at a hospital or skilled nursing facility, ...
What is the deductible for Part D?
Medicare defines a deductible as: “The amount you must pay for health care or prescriptions before Original Medicare, your prescription drug plan, or your other insurance begins to pay.”.
What percentage of Medicare coinsurance is 20 percent?
A 20 percent coinsurance means you (the beneficiary) would be responsible for 20 percent of a medical bill, while Medicare would pay the remaining 80 percent. It’s worth noting that the 20 percent you will pay as coinsurance is 20 percent of the Medicare-approved amount.
What is the coinsurance for Medicare Part B?
Coinsurance is the amount of the total bill that you must pay. A 20 percent coinsurance means you (the beneficiary) would be responsible for 20 percent ...
What is Medicare Supplement?
Medicare Supplement Insurance (also called Medigap) is a type of privately-sold insurance plan that is used in conjunction with Medicare Part A and Part B.
What is Medicare Advantage?
The amount you are required to pay for each health care visit or service. Medicare Advantage plans typically include cost-sharing measures such as copayments and coinsurance, and the amounts of these costs can correlate with that of the premium. The type of plan.
What is a Medicare Savings Account?
A Medicare Savings Account (MSA) is a type of Medicare Advantage plan that deposits money into a savings account that can be used to pay for out-of-pocket expenses prior to meeting your deductible.
What to look for when shopping for Medicare Advantage?
When you are shopping for a Medicare Advantage plan, you may consider features such as a plan’s range of benefits and possible network rules. But above all else, perhaps the biggest thing you might consider is the cost of a plan. When it comes to Original Medicare (Medicare Part A and Part B), the cost of premiums is standardized across the board.
How to save money on medicaid?
Saving money with Medicare Advantage 1 If you qualify for Medicaid, your Medicaid benefits can be used to help pay your Medicare Advantage premiums. 2 A Medicare Savings Account (MSA) is a type of Medicare Advantage plan that deposits money into a savings account that can be used to pay for out-of-pocket expenses prior to meeting your deductible. 3 If your Medicare Advantage plan includes a doctor and/or pharmacy network, you can save a considerable amount of money by staying within that network when receiving services. 4 Some Medicare Advantage plans may include extra health perks such as gym memberships. There is even the possibility of Medicare Advantage plans soon covering expenses like the cost of air conditioners, home-delivered meals and transportation.
How much does vision insurance cost?
Vision insurance can typically cost around $20 per month or less. 3. Hearing plans. Unlike dental and vision insurance, hearing insurance plans are not a common insurance product. Some hearing aid companies may offer extended warranties, but the warranties apply only to the hearing aid product itself.
Which state has the lowest Medicare premium?
A closer look at 2021 data also reveals: Nevada has the lowest average monthly premium for Medicare Advantage Prescription Drug (MAPD) plans at $11.58 per month. The highest average MAPD monthly premium is in North Dakota, at $76.33 per month.
Do you have to pay Medicare Part B premium?
When enrolled in a Medicare Advantage plan, you must also continue to pay your premium for Medicare Part B. Some Medicare Advantage plans can cover a portion of the Part B premium for you and may account for that by charging a higher premium for the plan. Many Medicare Advantage plans include annual deductibles.
What is an HMO plan?
Health Maintenance Organization (HMO) plan is a type of Medicare Advantage Plan that generally provides health care coverage from doctors, other health care providers, or hospitals in the plan’s network (except emergency care, out-of-area urgent care, or out-of-area dialysis). A network is a group of doctors, hospitals, and medical facilities that contract with a plan to provide services. Most HMOs also require you to get a referral from your primary care doctor for specialist care, so that your care is coordinated.
What happens if you get a health care provider out of network?
If you get health care outside the plan’s network, you may have to pay the full cost. It’s important that you follow the plan’s rules, like getting prior approval for a certain service when needed. In most cases, you need to choose a primary care doctor. Certain services, like yearly screening mammograms, don’t require a referral. If your doctor or other health care provider leaves the plan’s network, your plan will notify you. You may choose another doctor in the plan’s network. HMO Point-of-Service (HMOPOS) plans are HMO plans that may allow you to get some services out-of-network for a higher copayment or coinsurance. It’s important that you follow the plan’s rules, like getting prior approval for a certain service when needed.
What is a special needs plan?
Special Needs Plan (SNP) provides benefits and services to people with specific diseases, certain health care needs, or limited incomes. SNPs tailor their benefits, provider choices, and list of covered drugs (formularies) to best meet the specific needs of the groups they serve.
Do providers have to follow the terms and conditions of a health insurance plan?
The provider must follow the plan’s terms and conditions for payment, and bill the plan for the services they provide for you. However, the provider can decide at every visit whether to accept the plan and agree to treat you.
Can a provider bill you for PFFS?
The provider shouldn’t provide services to you except in emergencies, and you’ll need to find another provider that will accept the PFFS plan .However, if the provider chooses to treat you, then they can only bill you for plan-allowed cost sharing. They must bill the plan for your covered services. You’re only required to pay the copayment or coinsurance the plan allows for the types of services you get at the time of the service. You may have to pay an additional amount (up to 15% more) if the plan allows providers to “balance bill” (when a provider bills you for the difference between the provider’s charge and the allowed amount).
How much is the deductible for Medicare Advantage?
If you are enrolled in a Medicare Advantage plan, there may be a separate deductible for prescription drugs. In 2019, the average prescription drug deductible was $121 in Medicare Advantage plans ...
What are the costs of Medicare Advantage?
Medicare Advantage plans typically cover medically necessary procedures, office visits, hospitalizations and prescription drugs. Sometimes there can be higher deductibles and other costs for services that are not covered by ...
How much will Medicare Advantage cost in 2020?
In fact, more than nine out of 10 beneficiaries (93%) will have access to a Medicare Advantage plan with prescription drug coverage with no monthly premium in 2020. The Medicare Advantage average monthly plan premium is expected to decrease to $21.00, according to the Centers for Medicare and Medicaid Services.
How much is Medicare Part B 2021?
The standard Medicare Part B premium for 2021 is $148.60, but it can be higher, depending on your income level. Be sure to pay your Medicare Part B and Medicare Advantage premiums on time, so you won’t lose coverage. You could use automatic deductions to avoid missing a payment.
How many people will be enrolled in Medicare Advantage in 2020?
Enrollment in Medicare Advantage plans has doubled during the last decade, while monthly premiums have decreased. In 2020, 34% of all Medicare beneficiaries are enrolled in a Medicare Advantage plan. Researchers expect this trend to continue.
What are the costs that do not count toward your out-of-pocket maximum?
Costs that typically do not count toward your plan’s in-network out-of-pocket maximum include: Premiums, Prescription drug costs, Bills from out-of-network providers (those these will count toward an out-of-network limit), and. Services not covered by Medicare.
Does Medicare have an out-of-pocket limit?
Unlike traditional Medicare, all Medicare Advantage plans have an out-of-pocket limit. This is the maximum amount you will pay out of pocket for the year. Once you reach your out-of-pocket limit, your plan will pay in full for all covered medical expenses as long as you pay your premiums.
