Best Medicare Supplemental Insurance Companies
- Cigna. In addition to offering some of the most popular Medigap policy options, Cigna (NYSE: CI) also offers policyholders access to a 24/7 advice line staffed by trained nurses.
- Humana. Humana is a rock-solid supplemental insurance provider that offers plans throughout the country. ...
- Aetna. ...
- Mutual Of Omaha. ...
- CoverRight. ...
Full Answer
How to deal with Medicare as a secondary insurance?
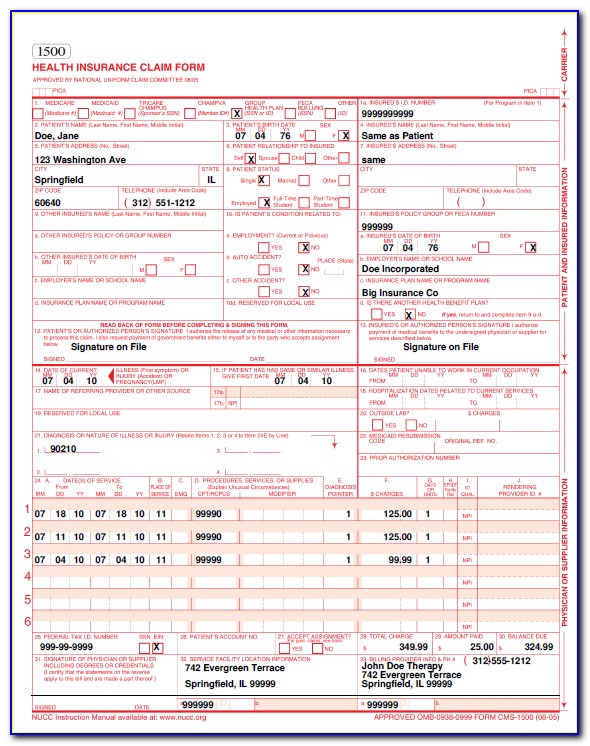
Oct 07, 2021 · Medigap is not the only type of insurance that can be secondary to Medicare. For example, those with TRICARE For Life have TFL as their secondary plan. A series of rules known as the coordination of benefits decides the order of payment in each case. Sometimes, although rarely, there can be up to three payers.
Will my secondary insurance be compatible with Medicare?
Feb 22, 2022 · Best Medicare Supplement Insurance Companies of 2022. Best Overall: Mutual of Omaha. Best User Experience: Humana. Best Set Pricing: AARP. Best Medigap Coverage Information: Aetna. Best Discounts ...
Is Medicare ever used as a secondary insurance carrier?
Jul 01, 2021 · What's the best secondary insurance for seniors? Our 2021 pick for the best Medicare supplement plan for new enrollees is Plan G. However, this comprehensive plan has a high monthly premium. The full list of the best Medicare supplement plans also recommends Plan K for seniors on a budget. However, some seniors with this plan could end up with high …
What is the best supplemental insurance to have with Medicare?
Mar 24, 2022 · Medicare Supplement Insurance helps you pay for the gaps in Medicare coverage. Once Medicare pays its share of the services you are receiving, Medigap will help you pay the rest. If your Part B policy says it covers 80% of a doctor’s visit, Medicare will pay that. Medigap kicks in for the other 20%.
What insurance goes best with Medicare?
| Provider | Forbes Health Ratings | Coverage area |
|---|---|---|
| Blue Cross Blue Shield | 5.0 | Offers plans in 48 states |
| Cigna | 4.5 | Offers plans in 26 states and Washington, D.C. |
| United Healthcare | 4.0 | Offers plans in all 50 states |
| Aetna | 3.5 | Offers plans in 44 states |
What are the top 3 most popular Medicare supplement plans in 2021?
What is the most comprehensive Medicare supplement plan?
What is the most widely accepted Medicare Advantage plan?
What is the deductible for Plan G in 2022?
What is the average cost of supplemental insurance for Medicare?
What is the difference between Medicare Plan G and Plan F?
What's the difference between Plan G and Plan N?
Why is Plan F being discontinued?
What are 4 types of Medicare Advantage plans?
- Health Maintenance Organization (HMO) Plans.
- Preferred Provider Organization (PPO) Plans.
- Private Fee-for-Service (PFFS) Plans.
- Special Needs Plans (SNPs)
What Medicare plans cover dental?
Do Medicare patients get treated differently?
What is secondary coverage for health insurance?
Secondary health insurance policies can fill in any coverage gaps, such as vision coverage, and available policies can also reduce the cost of heal...
Can you have two health insurance plans at the same time?
Yes, it's common to have multiple health insurance policies, and dual coverage can help cover more of your medical costs so that you pay less out o...
Which insurance companies offer secondary health insurance?
Plans are available from Blue Cross Blue Shield, USAA, AARP, UnitedHealthcare, Aetna, Aflac, Alliance, Humana, Cigna and more.
Is secondary health insurance worth it?
Secondary health insurance can give you financial protection if your main insurance policy has limitations. Most people have some form of secondary...
Why is AARP the best Medicare supplement?
We chose AARP as best for its set pricing for Medicare Supplement coverage because it doesn’t charge more as you grow older. This is especially helpful if you are still covered under your employer's insurance and may require coverage after the age of 65.
When is the best time to buy a Medicare Supplement?
The best time to buy a Medicare Supplement policy is during your Initial Medicare Open Enrollment Period. This is a one-time only, six-month span when federal law allows you to sign up for any Medicare Supplement policy you want that is sold in your state. Preexisting conditions are accepted during this time period, and you can't be denied a Medicare Supplement policy or charged more due to past or present health problems. Make sure you know when your Open Enrollment Period starts. 12
What is a Medicare Supplement Plan?
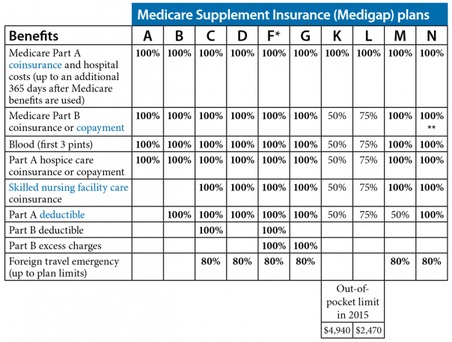
A Medicare Supplement Plan, also called a Medigap plan, is a plan sold by private companies, separate from Medicare. Medicare Supplement plans pay for the costs, or “gaps,” in coverage that are not paid for by Original Medicare. These can include prescriptions, doctor visits, vision and dental care, and more.
How is Medicare Supplement Plan cost determined?
The cost of a Medicare Supplement plan is determined by the individual insurance company that sells it. When researching different companies, be sure to ask how they price their policies. 10 Learning which factors they base their pricing on will help you determine both the costs for you today and what to expect in the future if your health situation changes.
How long do you have to switch back to Medicare Advantage?
If you’re unhappy with your Advantage plan and switch back to a Medicare Original Plan (which you can do within 12 months of enrolling in the Medicare Advantage plan), you then become eligible for Medicare Supplement insurance.
What to do if you have a gap in Medicare?
If you’re experiencing a gap in coverage from Medicare, then you may need to choose supplemental coverage . Explore your options when it comes to finding out what coverage you’re lacking and if things like prescriptions, doctor visits, vision, and dental care are covered or if you need help paying for them. If you’re not fully covered, then consider purchasing supplemental insurance.
Is Medicare Advantage the same as Medigap?
Both Medicare Advantage and Medigap plans are supplements to Original Medicare, but they are different. Medicare Advantage is an alternative Medicare plan. Medicare Advantage has a low or $0 monthly charge and covers most prescription medicine, though the choice of doctors and networks may be limited.
How much does secondary health insurance cost?
Secondary health insurance can cost anywhere from $5 per month to hundreds of dollars per month, depending on the type of coverage and the level of support the plan provides.
What is secondary insurance?
A secondary insurance policy is a plan that you get on top of your main health insurance.
What is Medicare Supplemental Insurance?
Medicare supplemental insurance: Also called Medigap plans, these supplemental plans can help cover services that are not covered by Original Medicare. Plans can also help pay your out-of-pocket costs for deductibles, copayments and coinsurance.
Why combine secondary insurance with cheap insurance?
Combining secondary health insurance with a cheap health insurance plan can help you pay less for broad coverage that would be more expensive if you purchased only one plan.
How much does Medicare supplement cost?
The cost of Medicare supplement plans has the biggest range because of the variety of plans and coverage options. Low-cost plans such as Plan K start at just $62 per month, and other choices such as Plan A or Plan B can cost more than $700 per month.
What happens if you have multiple insurance policies?
If you have multiple insurance policies, there is a clear order in which the plans will pay for health care services.
What is gap insurance?
Gap health insurance: Sometimes called limited benefits plans, these policies usually give you a lump-sum payment for covered illnesses or injuries, and you can use the payments to offset your out-of-pocket costs such as deductibles or copayments.
What is Medicare subsidized by?
In the simplest terms, Medicare is a health insurance plan subsidized by the federal government. It was originally created to help Social Security beneficiaries receive healthcare services, but it’s now been expanded to cover everyone who is:
How much is Medicare Part B deductible?
For 2019, the deductible for Medicare Part B is $185. After the deductible, you’ll pay 20% of most medical expenses.
What is a Medigap plan?
Also called Medigap because it covers “gaps” in costs after Medicare Parts A and B pay their share. Medigap Plans C and F, which cover the Medicare Part B deductible, are being discontinued in 2020. Sign up for Medigap during Open Enrollment to lock in the best premium for your plan. Our Approach.
What is covered by Plan A?
Plan A also covers 100% of coinsurances or copayments for hospice care services, 100% of Medicare Part B coinsurances or copayments for medical outpatient services, and 100% of the cost of the first three pints of blood you are administered during a procedure.
How much does Medicare pay for a doctor's visit?
Here’s an example with numbers: if the doctor’s visit had a Medicare-approved cost of $100, Medicare would pay $80, your Medigap would pay $15, and you would only have to pay $5.
What happens if you don't enroll in Medicare?
If you don’t enroll in Part A (inpatient hospital services) when you initially qualify, you may find yourself saddled with a 10% late enrollment penalty on your Part A premium. Says the Medicare website, “You'll have to pay the higher premium for twice the number of years you could have had Part A, but didn't sign up.”
How long do you have to be on Medicare if you have a disability?
If you have a disability and you’re receiving disability benefits from the Social Security Administration, you’ll automatically be enrolled in Parts A and B of Medicare once you’ve been receiving benefits for 24 months.
What is Medicare Secondary Payer?
Medicare Secondary Payer (MSP) is the term generally used when the Medicare program does not have primary payment responsibility - that is, when another entity has the responsibility for paying before Medicare. When Medicare began in 1966, it was the primary payer for all claims except for those covered by Workers' Compensation, ...
What age is Medicare?
Retiree Health Plans. Individual is age 65 or older and has an employer retirement plan: Medicare pays Primary, Retiree coverage pays secondary. 6. No-fault Insurance and Liability Insurance. Individual is entitled to Medicare and was in an accident or other situation where no-fault or liability insurance is involved.
Why is Medicare conditional?
Medicare makes this conditional payment so that the beneficiary won’t have to use his own money to pay the bill. The payment is “conditional” because it must be repaid to Medicare when a settlement, judgment, award or other payment is made. Federal law takes precedence over state laws and private contracts.
How long does ESRD last on Medicare?
Individual has ESRD, is covered by a GHP and is in the first 30 months of eligibility or entitlement to Medicare. GHP pays Primary, Medicare pays secondary during 30-month coordination period for ESRD.
When did Medicare start?
When Medicare began in 1966 , it was the primary payer for all claims except for those covered by Workers' Compensation, Federal Black Lung benefits, and Veteran’s Administration (VA) benefits.
Does GHP pay for Medicare?
GHP pays Primary, Medicare pays secondary. Individual is age 65 or older, is self-employed and covered by a GHP through current employment or spouse’s current employment AND the employer has 20 or more employees (or at least one employer is a multi-employer group that employs 20 or more individuals): GHP pays Primary, Medicare pays secondary.
Does Medicare pay for workers compensation?
Medicare generally will not pay for an injury or illness/disease covered by workers’ compensation. If all or part of a claim is denied by workers’ compensation on the grounds that it is not covered by workers’ compensation, a claim may be filed with Medicare.
What is the difference between primary and secondary insurance?
The insurance that pays first (primary payer) pays up to the limits of its coverage. The one that pays second (secondary payer) only pays if there are costs the primary insurer didn't cover. The secondary payer (which may be Medicare) may not pay all the uncovered costs.
How does Medicare work with other insurance?
When there's more than one payer, "coordination of benefits" rules decide which one pays first. The "primary payer" pays what it owes on your bills first, and then sends the rest to the "secondary payer" (supplemental payer) ...
What is a Medicare company?
The company that acts on behalf of Medicare to collect and manage information on other types of insurance or coverage that a person with Medicare may have, and determine whether the coverage pays before or after Medicare. This company also acts on behalf of Medicare to obtain repayment when Medicare makes a conditional payment, and the other payer is determined to be primary.
How long does it take for Medicare to pay a claim?
If the insurance company doesn't pay the claim promptly (usually within 120 days), your doctor or other provider may bill Medicare. Medicare may make a conditional payment to pay the bill, and then later recover any payments the primary payer should have made. If Medicare makes a. conditional payment.
How many employees does a spouse have to have to be on Medicare?
Your spouse’s employer must have 20 or more employees, unless the employer has less than 20 employees, but is part of a multi-employer plan or multiple employer plan. If the group health plan didn’t pay all of your bill, the doctor or health care provider should send the bill to Medicare for secondary payment.
Which pays first, Medicare or group health insurance?
If you have group health plan coverage through an employer who has 20 or more employees, the group health plan pays first, and Medicare pays second.
What is the phone number for Medicare?
It may include the rules about who pays first. You can also call the Benefits Coordination & Recovery Center (BCRC) at 1-855-798-2627 (TTY: 1-855-797-2627).
What is secondary health insurance?
Secondary health insurance is coverage you can buy separately from a medical plan. It helps cover you for care and services that your primary medical plan may not. This secondary insurance could be a vision plan, dental plan, or an accidental injury plan, to name a few. These are also called voluntary or supplemental insurance plans.
What insurance covers cancer?
These plans may give you a cash payment to apply to costs. Cancer Insurance: Some secondary insurance plans can help cover treatment costs related to certain types of cancer. Medicare Supplement Insurance: Medicare supplement plans help cover things that Original Medicare does not.
What is a supplement plan?
Supplemental health plans like vision , dental , and cancer insurance can provide coverage for care and services not typically covered under your medical plan. Supplemental plans often have a deductible, copay, and coinsurance. When you meet the deductible then your plan starts sharing part of the costs with you.
What is hospital care insurance?
Hospital Care Insurance: Need to stay in the hospital for an unexpected medical problem? Hospital care insurance can vary in terms, but often covers you for certain serious illnesses or conditions, such as stroke or heart attack. These plans may give you a cash payment to apply to costs.
What is gap insurance?
Gap insurance is a type of secondary insurance. It's sometimes called "limited benefits insurance.". Gap insurance offers cash benefits. This means it can help pay health care costs related to your deductible, copay, coinsurance, and other out-of-pocket medical expenses.
Is secondary insurance affordable?
Many secondary insurance plans have affordable monthly premiums. But cost is just one of the factors. Consider the following to find out if this type of coverage is right for you:
Does secondary health insurance cover cosmetic treatments?
Most plans will not cover services or treatment that are experimental or cosmetic. Read the details of any secondary health insurance plan you are considering. There are usually limits on coverage and services. This information is for educational purposes only. It is not medical advice.
Who sells Medicare Supplement Insurance?
Medicare Supplement Insurance plans (also called Medigap) are sold by dozens of private insurance companies all over the U.S. When shopping for coverage, it’s important to find the right plan for your unique needs and also to find the right insurance company. Different companies may sell Medigap plans that have different prices and terms, ...
What is the deductible for Medicare 2021?
1 Plans F and G offer high-deductible plans that each have an annual deductible of $2,370 in 2021. Once the annual deductible is met, the plan pays 100% of covered services for the rest of the year. The high-deductible Plan F is not available to new beneficiaries who became eligible for Medicare on or after January 1, 2020.
What states have Medigap plans?
Their costs and the availability of the types of plans, however, may vary. Medigap plans in Massachusetts, Minnesota and Wisconsin are standardized differently than they are in every other state. Learn more about Medigap plans in your state.
How much does Plan N pay for Part B?
4 Plan N pays 100% of the Part B coinsurance, except for a copayment of up to $20 for some office visits and up to $50 copayment for emergency room visits that don’t result in an inpatient admission .
What is a BCBS?
Blue Cross Blue Shield (BCBS) is among the leading health insurance carriers in the U.S., and BCBS companies were the very first to work in conjunction with Medicare. There are now 36 different locally operated BCBS companies administering coverage in all 50 states.
When will Medicare Supplement Plan F be available?
Medicare Supplement Plan F and Plan C are not available for sale to Medicare beneficiaries who became eligible for Medicare on or after Jan. 1, 2020.
Does Aetna offer Medigap?
Aetna offers a diverse portfolio of insurance products that includes Medigap plans. Over 1 million people trust Aetna for their Medicare Supplement Insurance. 3. Aetna offers several different types of Medigap plans. Plan availability may vary based on your location.
What is secondary insurance?
A separate plan that offers additional benefits is called secondary insurance. Your secondary health insurance can be another medical plan, such as through your spouse. More often, it’s a different type of plan you’ve purchased to extend your coverage. In that case, you may hear it referred to as voluntary or supplemental coverage .
What is hospital indemnity insurance?
Hospital indemnity insurance provides cash payments to help you manage the costs of a hospital stay, from your deductible to everyday expenses like daycare. If an injury or illness prevents you from working, disability insurance provides you with income on a weekly or monthly basis so you can still pay for your day-to-day expenses.
Does primary insurance cover lab tests?
As you probably know , your primary health insurance covers your basic medical expenses like doctors’ visits, lab tests and prescription drugs ― as well as some great perks . But your medical plan can’t cover everything. A separate plan that offers additional benefits is called secondary insurance. Your secondary health insurance can be another ...
Does my medical plan cover everything?
Your medical plan will cover many expenses, but it won't cover everything. So, you may want special policies to help cover those extra costs.
Do different people need different supplemental plans?
Different people need different supplemental plans, depending on their circumstances . Below, you’ll read how Peggy, Cecilia, DeWayne and Kevin use special policies to prepare for the unexpected financial and health challenges life sends their way.