
What is the Medicare emergency room copay?
What is the Copay for Medicare Emergency Room Coverage? A copay is the fixed amount that you pay for covered health services after your deductible is met. In most cases, a copay is required for doctor’s visits, hospital outpatient visits, doctor’s and hospital outpatients services, and prescription drugs.
Does Medicare pay for outpatient emergency room visits?
Outpatient emergency room visits are covered by Medicare Part B. You usually pay 20 percent of the Medicare-approved cost for doctor and other health care provider's services. You’ll also usually face a copayment from the hospital for each Medicare-covered service you receive, such as X-rays or lab tests.
Do I have to pay copay for emergency department visits?
applies. If your doctor admits you to the same hospital for a related condition within 3 days of your emergency department visit, you don't pay the copayment because your visit is considered part of your inpatient stay. To find out how much your test, item, or service will cost, talk to your doctor or health care provider.
How much does Medicare Part B pay for emergency department visits?
In most cases, if you receive care in a hospital emergency department and are covered by Medicare Part B, you'll also be responsible for: An annual Part B deductible of $233 (in 2022). A coinsurance payment of 20% of the Medicare-approved amount for most doctor’s services and medical equipment.
Does Medicare Part A cover emergencies?
It's an Emergency! Does Medicare Part A Cover Emergency Room Visits? Medicare Part A is sometimes called “hospital insurance,” but it only covers the costs of an emergency room (ER) visit if you're admitted to the hospital to treat the illness or injury that brought you to the ER.
What is the deductible for Medicare Part A hospital stay?
Medicare Part A pays only certain amounts of a hospital bill for any one spell of illness. (And for each spell of illness, you must pay a deductible before Medicare will pay anything. In 2020, the hospital insurance deductible is $1,408.)
Does Medicare Part A cover copays?
Copayments and Medicare Original Medicare comprises parts A and B, but only Part A has a copayment. People enrolled in Medicare Advantage or Medicare Part D prescription drug plans may pay copayments, but the amount will depend on the plan provider's rules.
Does Medicare Part A pay 100% of hospital costs?
Most medically necessary inpatient care is covered by Medicare Part A. If you have a covered hospital stay, hospice stay, or short-term stay in a skilled nursing facility, Medicare Part A pays 100% of allowable charges for the first 60 days after you meet your Part A deductible.
How does the Medicare Part A deductible work?
Part A Deductible: The deductible is an amount paid before Medicare begins to pay its share. The Part A deductible for an inpatient hospital stay is $1,556 in 2022. The Part A deductible is not an annual deductible; it applies for each benefit period.
What services are covered under Medicare Part A?
In general, Part A covers:Inpatient care in a hospital.Skilled nursing facility care.Nursing home care (inpatient care in a skilled nursing facility that's not custodial or long-term care)Hospice care.Home health care.
What is Part A deductible?
Medicare Part A Deductible in 2022 Medicare Part A covers certain hospitalization costs, including inpatient care in a hospital, skilled nursing facility care, hospice and home health care. It does not cover long-term custodial care. For 2022, the Medicare Part A deductible is $1,556 for each benefit period.
Which of the following does Medicare Part A not provide coverage for?
Medicare Part A does not cover 24-hour home care, meals, or homemaker services if they are unrelated to your treatment. It also does not cover personal care services, such as help with bathing and dressing, if this is the only care that you need.
What is Medicare Part A deductible for 2021?
Medicare Part A Premiums/Deductibles The Medicare Part A inpatient hospital deductible that beneficiaries will pay when admitted to the hospital will be $1,484 in 2021, an increase of $76 from $1,408 in 2020.
What will Medicare not pay for?
In general, Original Medicare does not cover: Long-term care (such as extended nursing home stays or custodial care) Hearing aids. Most vision care, notably eyeglasses and contacts. Most dental care, notably dentures.
Who pays for Medicare Part A?
Most people receive Medicare Part A automatically when they turn age 65 and pay no monthly premiums. If you or your spouse haven't worked at least 40 quarters, you'll pay a monthly premium for Part A.
What is a copay for emergency room?
What is the Copay for Medicare Emergency Room Coverage? A copay is the fixed amount that you pay for covered health services after your deductible is met. In most cases, a copay is required for doctor’s visits, hospital outpatient visits, doctor’s and hospital outpatients services, and prescription drugs. Medicare copays differ from coinsurance in ...
How does Medicare pay for outpatient services?
How You Pay For Outpatient Services. In order for your Medicare Part B coverage to kick in, you must pay the yearly Part B deductible. Once your deductible is met, Medicare pays its share and you pay yours in the form of a copay or coinsurance.
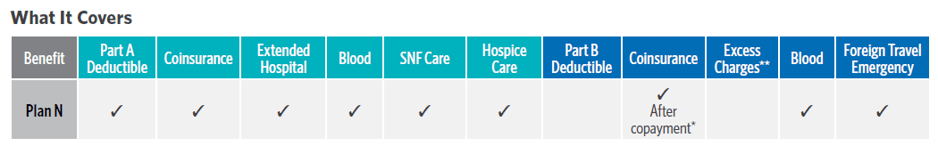
What is a Medigap plan?
Medigap is private health insurance that Medicare beneficiaries can buy to cover costs that Medicare doesn't, including some copays. All Medigap plans cover at least a percentage of your Medicare Part B coinsurance or ER copay costs.
How much is the deductible for Medicare Part B?
In most cases, if you receive care in a hospital emergency department and are covered by Medicare Part B, you'll also be responsible for: An annual Part B deductible of $203 (in 2021). A coinsurance payment of 20% of the Medicare-approved amount for most doctor’s services and medical equipment.
What are the services covered by Medicare?
Most ER services are considered hospital outpatient services, which are covered by Medicare Part B. They include, but are not limited to: 1 Emergency and observation services, including overnight stays in a hospital 2 Diagnostic and laboratory tests 3 X-rays and other radiology services 4 Some medically necessary surgical procedures 5 Medical supplies and equipment, like splints, crutches and casts 6 Preventive and screening services 7 Certain drugs that you wouldn't administer yourself
What is the OPPS payment?
The OPPS pays hospitals a set amount of money (or payment rate) for the services they provide to Medicare beneficiaries. The payment rate varies from hospital to hospital based on the costs associated with providing services in that area, and are adjusted for geographic wage variations.
What are the services of a hospital?
Emergency and observation services, including overnight stays in a hospital. Diagnostic and laboratory tests. X-rays and other radiology services. Some medically necessary surgical procedures. Medical supplies and equipment, like splints, crutches and casts. Preventive and screening services.
What Does Part A of Medicare Cover?
Part A of Medicare covers inpatient care in a hospital. If you have a hospital stay that doesn't involve receiving inpatient care, it will not be covered by Medicare Part A. Part A also covers skilled nursing facility care, hospice care, some in-home health care, and nursing home care.
What Is the Difference Between Inpatient and Outpatient Care?
Understanding the difference between inpatient and outpatient care is important because this often determines which part of Medicare will cover your medical fees. Inpatient care involves receiving medical care overnight and specifically requires the length of your stay to be directly related to your medical care.
Lengthy Outpatient Stays and MOON Forms
If you are staying at an emergency room or hospital setting for over 24 hours but are not receiving inpatient care, then the hospital will be required to give you a Medicare Outpatient Observation Notice, or MOON form.
The Two-Midnight Rule
A general rule that determines inpatient designation is known colloquially as the “two-midnight rule”. If your doctor expects you to stay in the hospital for a time period that crosses two midnights, then you will be admitted as an inpatient.
When Will Part A Cover Emergency Room Visits?
Although Part A doesn’t always cover emergency room visits, there are situations where it will. Specifically, if you are admitted to the same hospital within three days of your initial emergency room visit.
Part B Coverage: Emergency Room Visits With No Hospital Admission
If you go to the emergency room and are treated as an outpatient, then you will receive Medicare coverage under Part B, not Part A. In this scenario, your coverage will function the same way as if you were at your normal doctor’s office.
Medicare Part B: Additional Fees
You will be responsible for a copayment for each visit, as well as 20 percent of the Medicare-approved amount. Your Part B deductible will also apply for outpatient visits to emergency rooms. If you receive a MOON form, that is one way to know that you will be responsible for these fees.
What percentage of Medicare Part B is paid for doctor services?
In addition to these copays, you will pay a coinsurance for doctor services you receive in the ER. Medicare Part B typically pays 80 percent of the Medicare-approved amount for doctor services, and you are responsible for the remaining 20 percent of the cost. The Part B deductible also applies.
What is Medicare Made Clear?
Medicare Made Clear is brought to you by UnitedHealthcare to help make understanding Medicare easier. Click here to take advantage of more helpful tools and resources from Medicare Made Clear including downloadable worksheets and guides.
Do you pay copays for ER visits?
For example, you may pay copays or coinsurance for an ER visit and for services you receive while in the ER. Some plans also have deductibles. It’s important to check each plan’s details for information about coverage for ER visits.
Does Medicare Advantage cover out of network providers?
So, though Medicare Advantage plans typically have provider networks, they must cover emergency care from both network and out-of-network providers. In other words, Medicare Advantage plans cover ER visits anywhere in the U.S. Each Medicare Advantage plan sets its own cost terms for ER visits and other covered services.
Can ER copays change?
If an ER visit results in being you admitted to the hospital, then the visit is considered part of an inpatient stay and ER-related copays would not apply.
Does Medicare cover ER visits?
Yes, Medicare covers emergency room visits for injuries, sudden illnesses or an illness that gets worse quickly. Specifically, Medicare Part B will cover ER visits. And, since emergencies may occur anytime and anywhere, Medicare coverage for ER visits applies to any ER or hospital in the country. Note though, Medicare only covers emergency services ...
When does Medicare consider a person an inpatient?
Medicare considers a person an inpatient when their stay has extended beyond two midnights. If a doctor admits a person to the hospital, the law requires that they notify the individual that they are an inpatient.
What does Medicare Part A cover?
What does Part A cover? Medicare Part A covers hospital or inpatient care. A person usually visits the ER at a hospital. However, there is a difference between emergency care at a hospital and being a hospital inpatient. Medicare Part A specifically covers care when a person stays as an inpatient at the hospital.
What is the best Medicare plan?
We may use a few terms in this piece that can be helpful to understand when selecting the best insurance plan: 1 Deductible: This is an annual amount that a person must spend out of pocket within a certain time period before an insurer starts to fund their treatments. 2 Coinsurance: This is a percentage of a treatment cost that a person will need to self-fund. For Medicare Part B, this comes to 20%. 3 Copayment: This is a fixed dollar amount that an insured person pays when receiving certain treatments. For Medicare, this usually applies to prescription drugs.
What is Medicare Supplement?
Medicare Supplement Insurance, or Medigap, is a supplemental insurance plan that a person who has Original Medicare may purchase to cover some out-of-pocket expenses, including those for Medicare Part B. Medicare requires that Medigap plans offer the same benefits regardless of the insurance provider.
What is the 20% coinsurance for ambulance?
The out-of-pocket expenses for emergency transportation to an ER include the 20% coinsurance. The Part B deductible applies to this amount. If an ambulance company believes Medicare may not cover their service, they must provide an Advance Beneficiary Notice of Noncoverage.
How much of Medicare deductible is for doctor services?
20% of the Medicare-approved amount for a doctor’s services. the deductible, which applies for doctor’s services. One exception to the ER coverage rules applies when a person returns to a hospital in need of inpatient care within 3 days of their initial visit to the ER.
What is Medicare Advantage?
Medicare Advantage includes benefits from Parts A, B, and sometimes D, which covers prescription drug coverage. It may also offer coverage for services, such as vision, dental, and hearing care.
How much is a hospital visit covered by Medicare?
If Medicare Part A pays for the hospital visit, a person is responsible for a deductible of $1,260. A deductible is a spending total that a person must self-fund on a policy before coverage commences. Once a person spends this amount out of pocket on treatment, Medicare Part A pays 100% of the hospital costs for up to 60 days.
What does Medicare Part A cover?
Medicare Part A provides hospital coverage. If a doctor admits an individual into the hospital for at least 2 midnights, Medicare Part A covers hospital services, such as accommodation costs and testing, while a person stays in the facility.
What is a scenario in Medicare Part B?
The following are some example scenarios: Scenario 1. Scenario: An ambulance brought you to the ER. What pays: Medicare Part B generally covers ambulance transportation to a hospital, skilled nursing facility, or critical access hospital.
How long does it take to go back to the ER?
A person goes to the ER, and the doctor discharges them. The health problem returns, and the individual needs to go back to the ER within 3 days. The doctor admits the person. In this example, Medicare Part A would pay for the hospital stay.
What does Part B pay for?
However, Part B will pay for the doctor’s services while you are in the hospital. SCENARIO 3. Scenario: You are in the ER, and a doctor writes an order to admit you to the hospital. What pays: Part A will pay for your hospital stay and the services that you received when you were an outpatient.
Does Medicare cover emergency care?
Medicare Supplement, or Medigap. Medicare supplement, or Medigap, policies may provide emergency health coverage if a person is traveling outside the United States. Traditional Medicare does not traditionally cover costs for emergency care if a person is traveling outside the country.
Does Medicare cover ER visits?
Medicare Part B usually covers emergency room (ER) visits, unless a doctor admits a person to the hospital for a certain length of time. For inpatient admissions, Medicare Part A may cover the ER visit and subsequent hospital stay if the length of admission into hospital spans at least 2 midnights. In this article, we break down how Medicare ...
Original Medicare Part B (medical insurance) generally covers ER visits
Part B usually covers 80% of ER services when you have an injury, a sudden illness or an illness that gets worse quickly. 1
Other Parts of Medicare can help pay for ER visits, too
ER visits are considered outpatient stays, and Part A does not cover outpatient stays. However, if you’re formally admitted to the hospital with a doctor’s order, Part A will help pay for your inpatient hospital stay. It will also pay for related outpatient services provided during the 3 days before your admission date. 3
Learn more about Medicare
For more helpful information on Medicare, check out these 10 frequently asked questions about Medicare plans.
