How to manually file a claim with Medicare?
- A copy of the bill
- Your Medicare information
- The doctor’s NPN (call the doctor who treated you and ask them for it)
How can I contact Medicare?
- To check on your eligibility for Medicare benefits.
- To create an account called “my Social Security” so you can go online to verify your earnings, to get an estimate of your future benefits, or to manage your monthly ...
- To get the status of a claim.
- To get a replacement for your Medicare card.
How to fill in Medicare claims?
Few retirees have sufficient financial resources to pay for long-term care.
- The need for assistance. Anyone may need assistance as they age, whether due to dementia, illness, loss of eyesight, or simple frailty.
- Medicare coverage. ...
- Medicaid coverage. ...
- Out-of-pocket costs. ...
- Insurance. ...
- Veterans benefits. ...
- Planning for the future. ...
What is the mailing address for Medicare claims?
Providers can use the addresses provided below to submit the following types of correspondence:
- Enrollment (CMS applications and PECOS Web Certification Statements and supporting documentation)
- Medicare Secondary Payer (MSP)
- Paper Claims
- Redeterminations (All types including overpayments, CERT, RA, SMRC, and UPIC)
- Refunds
- Responses to Noridian requests for additional documentation
- Written Inquiries
What is the fax number for Medicare?
Call 1-800-MEDICARE (1-800-633-4227). TTY users can call 1-877-486-2048. Email us at [email protected]. Send us a fax at 1-844-530-3676.
How do providers submit claims to Medicare?
Contact your doctor or supplier, and ask them to file a claim. If they don't file a claim, call us at 1-800-MEDICARE (1-800-633-4227). TTY: 1-877-486-2048. Ask for the exact time limit for filing a Medicare claim for the service or supply you got.
What form is used to send claims to Medicare?
CMS-1500 claim formThe CMS-1500 claim form is used to submit non-institutional claims for health care services provided by physicians, other providers and suppliers to Medicare.
Can you send paper claims to Medicare?
The Administrative Simplification Compliance Act (ASCA) requires that as of October 16, 2003, all initial Medicare claims be submitted electronically, except in limited situations. Medicare is prohibited from payment of claims submitted on a paper claim form that do not meet the limited exception criteria. web page.
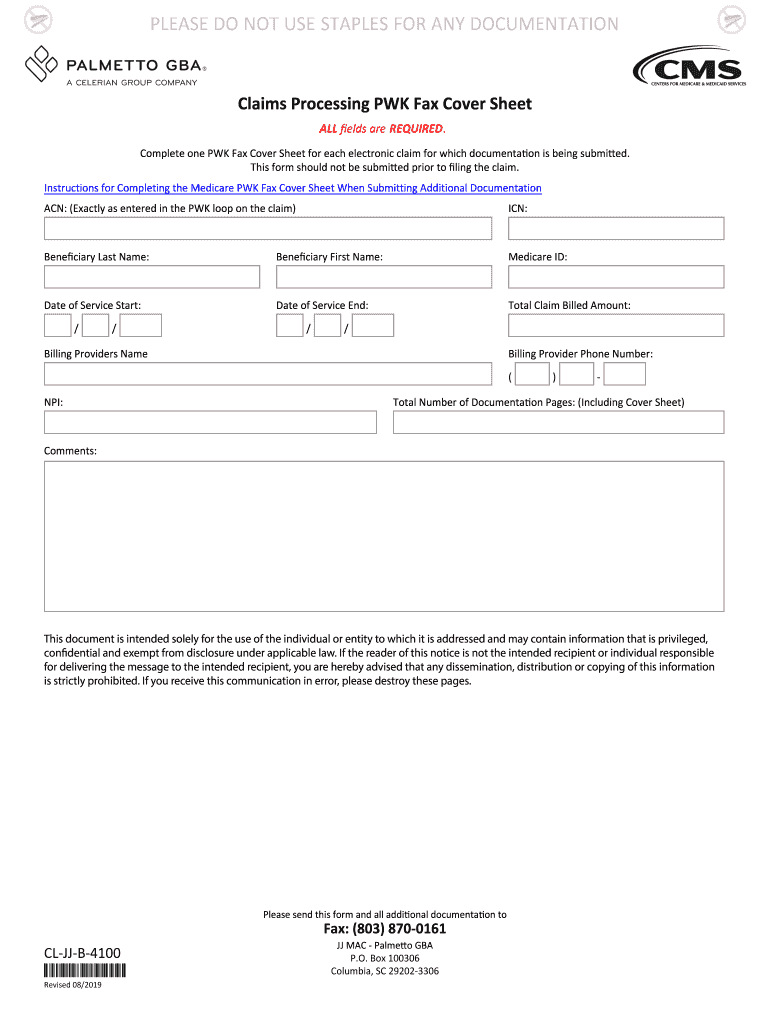
Where do I fax Medicare claims?
Complete all fields and fax to 877- 439-5479 or mail the form to the applicable address/number provided at the bottom of the page. Complete ONE (1) Medicare Fax / Mail Cover Sheet for each electronic claim for which documentation is being submitted. This form should not be submitted prior to filing the claim.
What is the address for Medicare claims?
Medicare claim address, phone numbers, payor id – revised listStateAppeal addressArizonaAZMedicare Part B PO Box 6704 Fargo, ND 58108-6704MontanaMTMedicare Part B PO Box 6735 Fargo, ND 58108-6735North DakotaNDMedicare Part B PO Box 6706 Fargo, ND 58108-6706South DakotaSDMedicare Part B PO Box 6707 Fargo, ND 58108-670719 more rows
What is the first step in submitting Medicare claims?
The first thing you'll need to do when filing your claim is to fill out the Patient's Request for Medical Payment form. ... The next step in filing your own claim is to get an itemized bill for your medical treatment.More items...•
What is the standard format used for submission of electronic claims?
837PThe 837P (Professional) is the standard format health care professionals and suppliers use to send health care claims electronically. The ANSI ASC X12N 837P (Professional) Version 5010A1 is the current electronic claim version.
Which providers submit the CMS 1500 claim form?
The Form CMS-1500 is the standard paper claim form used by health care professionals and suppliers to bill Medicare Carriers or Part A/B and Durable Medical Equipment Medicare Administrative Contractors (A/B MACs and DME MACs).
What is the difference between paper claims and electronic claims?
An “electronic claim" is a paperless patient claim form generated by computer software that is transmitted electronically over the telephone or computer connected to a health insurer or other third-party payer (payer) for processing and payment, while A “manual claim” is a paper claim form that refers to either the ...
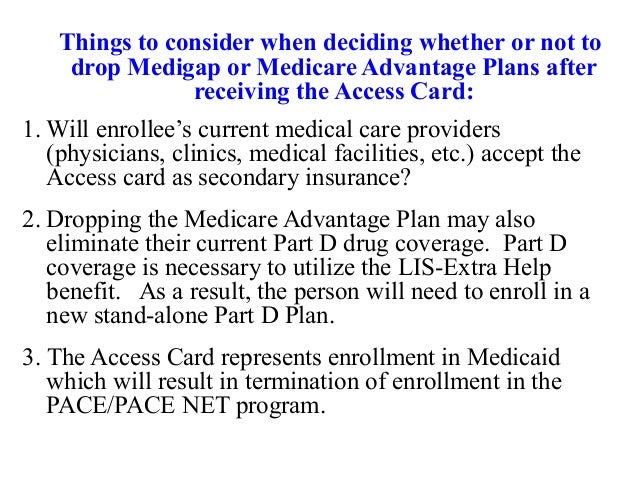
Does Medicare accept secondary paper claims?
Currently, Medicare does not accept electronically filed claims when there is more than one payer primary to Medicare. Claims that involve more than one primary payer to Medicare must be submitted on the 1500 paper claim form, with all appropriate attachments.
Does Medicare accept handwritten claims?
Medicare to Reject Handwritten Claims. Providers who wish to continue to submit paper claims may do so as long as they are printed and as long as the only handwriting included in the claim is in a signature field. Software programs are available that will allow providers to print information into a CMS 1500 form.
File a complaint (grievance)
Find out how to file a complaint (also called a "grievance") if you have a concern about the quality of care or other services you get from a Medicare provider. Contact your State Health Insurance Assistance Program (SHIP) for local, personalized Medicare counseling.
File a claim
Get information on how and when to file a claim for your Medicare bills (sometimes called "Medicare billing"). You should only need to file a claim in very rare cases.
Check the status of a claim
Check your claim status with your secure Medicare account, your Medicare Summary Notice (MSN), your Explanation of Benefits (EOB), Medicare's Blue Button, or contact your plan.
File an appeal
How to appeal a coverage or payment decision made by Medicare, your health plan, drug plan or Medicare Medical Savings Account (MSA) Plan.
Your right to a fast appeal
Learn how to get a fast appeal for Medicare-covered services you get that are about to stop.
Authorization to Disclose Personal Health Information
Access a form so that someone who helps you with your Medicare can get information on your behalf.
What is the CRC number?
to 8:00 p.m., Eastern Time, except holidays, at toll-free lines: 1-855-798-2627 (TTY/TDD: 1-855-797-2627 for the hearing and speech impaired).
What is the phone number for BCRC?
to 8:00 p.m., Eastern Time, except holidays, at toll-free lines: 1-855-798-2627 (TTY/TDD: 1-855-797-2627 for the hearing and speech impaired).
What information do you need to release a private health insurance beneficiary?
Prior to releasing any Private Health Information about a beneficiary, you will need the beneficiary's last name and first initial, date of birth, Medicare Number, and gender. If you are unable to provide the correct information, the BCRC cannot release any beneficiary specific information.
When does Medicare use the term "secondary payer"?
Medicare generally uses the term Medicare Secondary Payer or "MSP" when the Medicare program is not responsible for paying a claim first. The BCRC uses a variety of methods and programs to identify situations in which Medicare beneficiaries have other health insurance that is primary to Medicare.
What is BCRC in Medicare?
The Benefits Coordination & Recovery Center (BCRC) consolidates the activities that support the collection, management, and reporting of other insurance coverage for Medicare beneficiaries. The purpose of the COB program is to identify the health benefits available to a Medicare beneficiary and to coordinate the payment process to prevent mistaken Medicare payment. The BCRC does not process claims or claim-specific inquiries. The Medicare Administrative Contractors, (MACs), intermediaries, and carriers are responsible for processing claims submitted for primary or secondary payment and resolving situations where a provider receives a mistaken payment of Medicare benefits.
What is MLN CMS?
The Medicare Learning Network (MLN) is a CMS initiative to ensure Medicare physicians, providers and supplies have immediate access to Medicare coverage and reimbursement rules in a brief, accurate, and easy to understand format. To access MLN Matters articles, click on the MLN Matters link.
Does BCRC release beneficiary information?
You will be advised that the beneficiary's information is protected under the Privacy Act, and the BCRC will not release the information. The BCRC will only provide answers to general COB or MSP questions. For more information on the BCRC, click the Coordination of Benefits link.
Does BCRC process claims?
The BCRC does not process claims or claim-specific inquiries. The Medicare Administrative Contractors, (MACs), intermediaries, and carriers are responsible for processing claims submitted for primary or secondary payment and resolving situations where a provider receives a mistaken payment of Medicare benefits.
Can a Medicare claim be terminated?
Medicare claims paying offices can terminate records on the CWF when the provider has received information that MSP no longer applies (e.g., cessation of employment, exhaustion of benefits). Termination requests should be directed to your Medicare claims payment office.