Full Answer
What is the average Medicare payment for a DRG?
The average Medicare payment for this DRG was $6,213. Here are the top 20 highest paying DRGs to hospitals (listed by the Average Medicare Payments): $223,532 – Heart transplant or implant of heart assist system with major complication or comorbidity.
What are the highest paying DRGs?
Here are the top 20 highest paying DRGs to hospitals (listed by the Average Medicare Payments): $223,532 – Heart transplant or implant of heart assist system with major complication or comorbidity. $140,536 – Extensive burns or full thickness burns with mechanical ventilation > 96 hours with skin graft.
What is the difference between DRG’s with high relative weight?
DRGs with a relative weight of less than 1.0 are less resource-intensive to treat and are generally less costly to treat. DRG’s with a relative weight of more than 1.0 generally require more resources to treat and are more expensive to treat. The higher the relative weight, the more resources are required to treat a patient with that DRG.
What is DRG weight and why is it important?
DRG’s with a relative weight of more than 1.0 generally require more resources to treat and are more expensive to treat. The higher the relative weight, the more resources are required to treat a patient with that DRG. This is why very serious medical situations, such as organ transplants, have the highest DRG weight.

What are the highest DRG?
The top 10 DRGs overall are: normal newborn, vaginal delivery, heart failure, psychoses, cesarean section, neonate with significant problems, angina pectoris, specific cerebrovascular disorders, pneumonia, and hip/knee replacement. They comprise nearly 30 percent of all hospital discharges.
What are DRG weights?
DRG Weights The CMS assigns a unique weight to each DRG. The weight reflects the average level of. resources for an average Medicare patient in the DRG, relative to the average level of resources. for all Medicare patients.28 The weights are intended to account for cost variations between. different types of treatments ...
What is the highest MS DRG?
Top 10 MS-DRG The ten highest volume Medicare MS-DRGs represent about 30% of total Medicare patients. Each of the 10 highest volume MS-DRG represent from about 2.1% to 4.6% of total Medicare volume.
How are DRG weights determined?
The DRG relative weights are estimates of the relative resource intensity of each DRG. These weights are computed by estimating the average resource intensity per case for each DRG, measured in dollars, and dividing each of those values by the average resource intensity per case for all DRG's, also measured in dollars.
What is a high CMI?
A higher CMI indicates a more complex and resource-intensive case load. Although the MS-DRG weights, provided by the Centers for Medicare & Medicaid Services (CMS), were designed for the Medicare population, they are applied here to all discharges regardless of payer.
What are the 3 DRG options?
There are currently three major versions of the DRG in use: basic DRGs, All Patient DRGs, and All Patient Refined DRGs. The basic DRGs are used by the Centers for Medicare and Medicaid Services (CMS) for hospital payment for Medicare beneficiaries.
What does DRG 999 mean?
• MS-DRG No. 999 - Represents a discharge with invalid data, making it ungroupable.
What is a DRG rate?
Diagnosis-related group reimbursement (DRG) is a reimbursement system for inpatient charges from facilities. This system assigns payment levels to each DRG based on the average cost of treating all TRICARE beneficiaries in a given DRG.
What is a DRG What is difference between a DRG and a MS-DRG?
DRG stands for diagnosis-related group. Medicare's DRG system is called the Medicare severity diagnosis-related group, or MS-DRG, which is used to determine hospital payments under the inpatient prospective payment system (IPPS).
Why do surgical cases tend to have a higher relative weight?
In general, the relative weights assigned to surgical DRGs are higher to reflect the increased resources required for a surgical procedure and the hospital stay.
What is DRG validation?
DRG validation involves review of claim information (including but not limited to all diagnoses, procedure codes, revenue codes) and/or medical record documentation to determine correct coding on a claim submission and in accordance with industry coding standards as outlined by the Official Coding Guidelines, the ...
How many DRGs are there?
Diagnosis-related group (DRG) is a system to classify hospital cases into one of originally 467 groups, with the last group (coded as 470 through v24, 999 thereafter) being "Ungroupable".
What is Medicare DRG?
What exactly is a Medicare DRG? A Medicare DRG (often referred to as a Medicare Severity DRG) is a payment classification system that groups clinically-similar conditions that require similar amounts of inpatient resources. It’s a way for Medicare to easily pay your hospital after an inpatient stay.
What does DRG mean in Medicare?
A DRG dictates how much Medicare pays the hospital if you’re admitted as an inpatient. However, keep in mind that your DRG does not affect what you owe for an inpatient admission when you have Medicare Part A coverage, assuming you receive medically necessary care and that your hospital accepts Medicare.
Why was the DRG system created?
The DRG system was created to standardize hospital reimbursement for Medicare patients while also taking regional factors into account. Another goal was to incentivize hospitals to become more efficient. If your hospital spends less money taking care of you than the DRG payment it receives, it makes a profit.
How is a DRG determined?
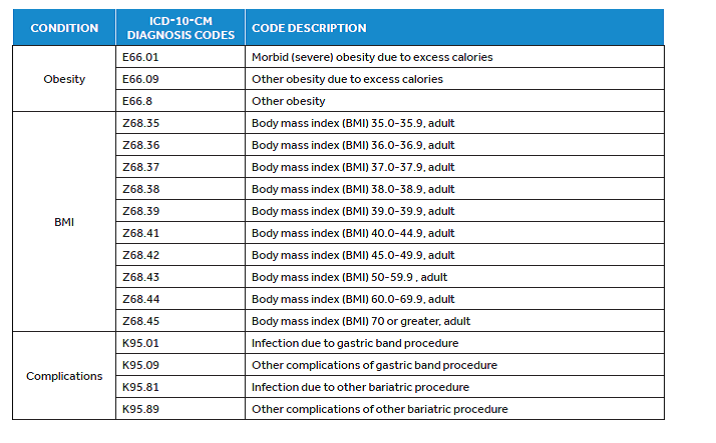
How is a Medicare DRG determined? A Medicare DRG is determined by the diagnosis that caused you to become hospitalized as well as up to 24 secondary diagnoses (otherwise known as complications and comorbidities) you may have. Medical coders assign ICD-10 diagnosis codes to represent each of these conditions.
What is a DRG in 2021?
April 27, 2021. A Medicare diagnosis related group (DRG) affects the pre-determined amount that Medicare pays your hospital after an inpatient admission. Understanding what it means can help you gain insight into the cost of your care. As you probably know, healthcare is filled with acronyms. Although you may be familiar with many ...
How to contact Medicare DRG?
Speak with a licensed insurance agent. 1-800-557-6059 | TTY 711, 24/7. Your Medicare DRG is based on your severity of illness, risk of mortality, prognosis, treatment difficulty and need for intervention as well as the resource intensity necessary to care for you. Here’s how it works:
How long does it take for Medicare to readmit a patient?
However, Medicare has rules in place that penalize hospitals in certain circumstances if a patient is readmitted within 30 days. This deters premature discharges and helps ensure Medicare patients are discharge only when they are truly ready to go home or to another post-discharge care setting.
What is a DRG relative weight?
DRGs with a relative weight of less than 1.0 are less resource-intensive to treat and are generally less costly to treat. DRG’s with a relative weight of more than 1.0 generally require more resources to treat and are more expensive to treat.
What is a DRG in Medicare?
DRG stands for diagnosis-related group. Medicare's DRG system is called the Medicare severity diagnosis-related group, or MS-DRG, which is used to determine hospital payments under the inpatient prospective payment system (IPPS). It's the system used to classify various diagnoses for inpatient hospital stays into groups and subgroups ...
How much did nonprofit hospitals make in 2017?
The largest nonprofit hospitals, however, earned $21 billion in investment income in 2017, 4 and are certainly not struggling financially. The challenge is how to ensure that some hospitals aren't operating in the red under the same payment systems that put other hospitals well into the profitable realm.
When do hospitals assign DRG?
When you've been admitted as an inpatient to a hospital, that hospital assigns a DRG when you're discharged, basing it on the care you needed during your hospital stay. The hospital gets paid a fixed amount for that DRG, regardless of how much money it actually spends treating you.
Which has higher labor costs, Knoxville or Manhattan?
For example, a hospital in Manhattan, New York City probably has higher labor costs, higher costs to maintain its facility, and higher resource costs than a hospital in Knoxville, Tennessee. The Manhattan hospital probably has a higher base payment rate than the Knoxville hospital.
Does a hospital make money on DRG?
If a hospital can effectively treat you for less money than Medicare pays it for your DRG, then the hospital makes money on that hospitalization. If the hospital spends more money caring for you than Medicare gives it for your DRG, then the hospital loses money on that hospitalization. David Sacks/Stone/Getty Images.
Does Medicare increase hospital base rate?
Each of these things tends to increase a hospital’s base payment rate. Each October, Medicare assigns every hospital a new base payment rate. In this way, Medicare can tweak how much it pays any given hospital, based not just on nationwide trends like inflation, but also on regional trends.
What Is MS-DRG?
MS-DRG means Medicare severity-diagnosis-related group. It’s a system of classifying patient hospital stays. Within the system, Medicare classifies groups to facilitate service payments.
The MS-DRG Payment Classification System
The MS-DRG enables the Medicare system to determine hospital payments. This payment system falls under the inpatient prospective payment system (IPPS).
What is a DRG in Medicare?
The diagnoses are listed as DRGs, or “diagnostic-related groups”. These are essentially the reason why the patient was in the hospital: a disease, a condition, or a surgical procedure. Medicare will pay set amount of money to hospitals for each DRG. The Medicare payment per DRG is also affected by the amount of money a given hospital gets ...
How does Medicare affect DRG?
The Medicare payment per DRG is also affected by the amount of money a given hospital gets for being classified as a teaching hospital, by disproportionate share funds, by capital funds, and by outlier funds. Thus an academic medical center that cares for a disproportionate number of Medicaid or uninsured patients will be paid much more ...