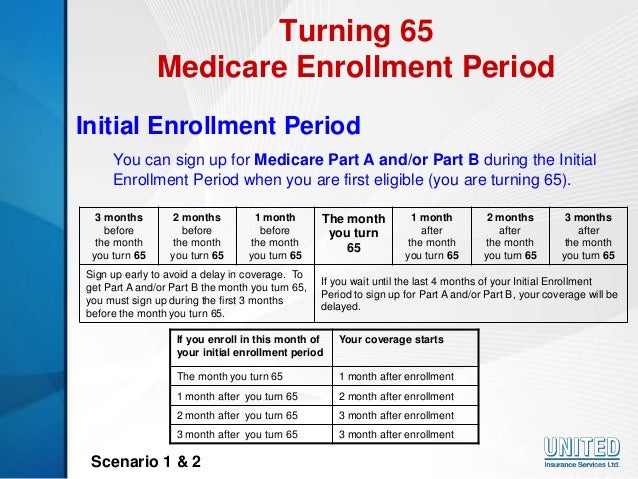
- Your Medicare Initial Enrollment Period (IEP): You can enroll in a Part D plan in the 3 months you turn 65, the month of your 65th birthday or 3 months ...
- The Medicare Annual Enrollment Period (AEP): This runs from Oct. ...
- The Medicare Advantage Open Enrollment Period (OEP): This lasts from Jan. ...
What is the Medicare Part D initial enrollment period (IEP)?
Your Medicare Part D Initial Enrollment Period (IEP) is a seven (7) month window of time that starts three months before your Medicare eligibility month (or 65th birthday month), plus the month of your Medicare-eligibility month (65th birthday month), and continues for three months after your birthday or Medicare eligibility month.
What does IEP stand for in Medicare?
IEP stands for the Initial Enrollment Period. What is the difference between Medicare IEP and ICEP? The difference between IEP and ICEP is the IEP is for enrolling in Part A, Part B, and Part D. The ICEP is for joining in Part C. Can you enroll in Medicare Early? You sign up for Medicare 3-months before you turn 65. Was this article helpful ?
What is the difference between the IEP and ICEP periods?
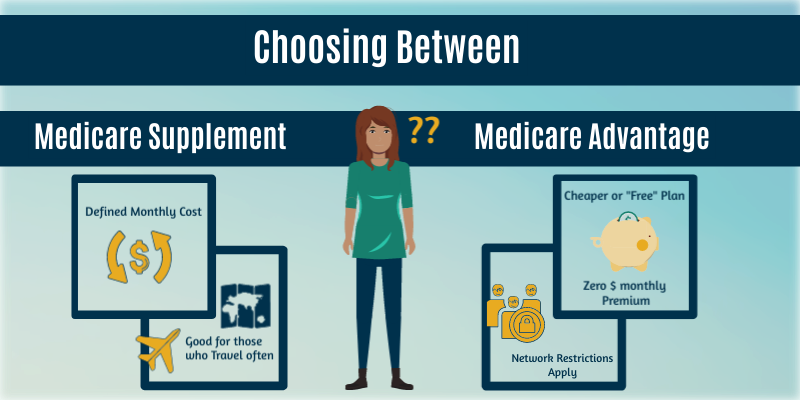
The IEP and ICEP are both one-time Medicare enrollment periods. For many beneficiaries, these periods happen at the same time. The Medicare Initial Enrollment Period (IEP) is your first opportunity to enroll in Original Medicare, which consists of Part A and Part B and is administered by the federal government.
When does my IEP start and end?
Your IEP starts 3 months before your 65th birthday and ends 3 months after your birthday month. The second chance to enroll in Part D coverage is during the Medicare Fall Open Enrollment Period. Medicare has times you may enroll in or make changes to your Part D coverage.
What is a Medicare IEP?
The Medicare Initial Enrollment Period (IEP) It's called your Initial Enrollment Period – or IEP for short. Your IEP includes your 65th birthday month, the 3 months before and the 3 months after. Example: You turn 65 on June 7. Your IEP is March 1 – September 30.
What is the difference between Medicare IEP and Icep?
If you enroll in Medicare Part A and Part B when you turn 65, your ICEP will run concurrently with your IEP. Your IEP is an enrollment period that begins three months before you turn 65, includes the month of your birthday and continues on for three more months, for a total of seven months.
Can I add Part D to my Medicare at any time?
Keep in mind, you can enroll only during certain times: Initial enrollment period, the seven-month period that begins on the first day of the month three months before the month you turn 65 and lasts for three months after the birthday month.
What are the four stages of Medicare Part D?
The Four Coverage Stages of Medicare's Part D ProgramStage 1. Annual Deductible.Stage 2. Initial Coverage.Stage 3. Coverage Gap.Stage 4. Catastrophic Coverage.
Do IEP and Icep occur at the same time?
During the ICEP, your clients can enroll in a Medicare Advantage health plan with or without prescription drug coverage. The ICEP occurs simultaneously with the IEP for Part B and Part D. The ICEP begins 3 months before the month of entitlement to Medicare (e.g., the person's 65th birthday).
What does Icep mean?
Initial Coverage Election PeriodIf you plan to enroll in a Medicare Advantage plan (Part C), your first opportunity is your Initial Coverage Election Period (ICEP).
What is the main problem with Medicare Part D?
The real problem with Medicare Part D plans is that they weren't set up with the intent of benefiting seniors. They were set up to benefit: –Pharmacies, by having copays for generic medications that are often far more than the actual cost of most of the medications.
When did Medicare Part D become mandatory?
The MMA also expanded Medicare to include an optional prescription drug benefit, “Part D,” which went into effect in 2006.
Is it worth getting Medicare Part D?
Most people will need Medicare Part D prescription drug coverage. Even if you're fortunate enough to be in good health now, you may need significant prescription drugs in the future. A relatively small Part D payment entitles you to outsized benefits once you need them, just like with a car or home insurance.
What is Stage 2 of Medicare Part D?
Stage 2 – Initial Coverage In Stage 2, you pay your copay and we pay the rest. You stay in Stage 2 until the amount of your year-to-date total drug costs reaches $4,430. Total drug costs include your copay and what we pay.
What is the best Medicare Part D plan?
Best-rated Medicare Part D providersRankMedicare Part D providerMedicare star rating for Part D plans1Kaiser Permanente4.92UnitedHealthcare (AARP)3.93BlueCross BlueShield (Anthem)3.94Humana3.83 more rows•Mar 16, 2022
How many stages do Part D plans have?
four different phasesThere are four different phases—or periods—of Part D coverage: Deductible period: Until you meet your Part D deductible, you will pay the full negotiated price for your covered prescription drugs. Once you have met the deductible, the plan will begin to cover the cost of your drugs.
How many enrollment periods are there for Medicare Part D?
There are three different enrollment periods for Medicare Part D. Each one is unique to you, the beneficiary. It’s important to understand these enrollment periods to avoid late penalties that will stay with you forever.
When does IEP end?
Everyone’s Initial Enrollment Period is different, it’s specific to your 65th birthday month. Your IEP starts 3 months before your 65th birthday and ends 3 months after your birthday month.
What is a special enrollment period?
Life happens for everyone; Special Enrollment Periods are for when certain situations or events happen in life. SEPs give you chances to make changes to your Part D plan or Medicare Advantage plan.
What is an AEP?
AEP is commonly mistaken for the Open Enrollment Period. During AEP, members can openly make changes to their current coverage. This includes enrolling in a Part D drug plan or switching from one Part D plan to another Part D plan that better suits your medical needs.
When is the AEP period?
Each fall the Annual Election Period runs from October 15th through December 7th. AEP is commonly mistaken for the Open Enrollment Period.
When do you turn 65 on an IEP?
Example: You turn 65 on June 7. Your IEP is March 1 – September 30. If, however, your birthday is on the 1st of the month, then your IEP is determined as though you were born the month before. Example: You turn 65 on June 1. Your IEP is February 1 – August 31.
When is Medicare enrollment period?
You will have a chance to review your coverage, and make changes each year during the Medicare Annual Enrollment Period, Oct. 15 – Dec. 7.
What happens if you miss your Medicare enrollment?
If you miss your Initial Enrollment Period, Medicare offers a General Enrollment Period (GEP) for those who did not sign up around their 65th birthday. You could face late enrollment penalties if you wait too long to sign up, and don't qualify for a Special Enrollment Period.
How long does it take to get Medicare if you have a disability?
The Medicare Initial Enrollment Period (IEP) Around your 65th birthday (or 25th disability check), you'll have a 7-month window of time when you can sign up for Medicare. It's called your Initial Enrollment Period – or IEP for short. Your IEP includes your 65th birthday month, the 3 months before and the 3 months after.
What is a dual special needs plan?
Dual Special Needs Plan (DSNPs) are a special kind of Medicare Advantage Plan that combine Parts A, B and D Medicaid, and extra benefits such as dental and vision.
Is dental insurance covered by Medicare?
Dental, vision & other health benefits. Dental, vision, hearing and fitness benefits are not covered by Medicare Parts A, B and D. Only Medicare Advantage plans offer these benefits and others, such as transportation for medical appointments and virtual doctor visits.
Does Medicare notify you of your IEP?
Medicare may not notify you about your eligibility, so be sure to get your Initial Enrollment Period (IEP) dates and put them in your calendar. It's best to sign up for Medicare toward the start of your IEP. That way your coverage will begin as soon as you're eligible.
How to get prescription drug coverage
Find out how to get Medicare drug coverage. Learn about Medicare drug plans (Part D), Medicare Advantage Plans, more. Get the right Medicare drug plan for you.
What Medicare Part D drug plans cover
Overview of what Medicare drug plans cover. Learn about formularies, tiers of coverage, name brand and generic drug coverage. Official Medicare site.
How Part D works with other insurance
Learn about how Medicare Part D (drug coverage) works with other coverage, like employer or union health coverage.
What is the IEP2 enrollment period?
Initial Enrollment Period 2 (IEP2) Another enrollment period that is also 7-months is the Initial Enrollment Period 2. The IEP2 is for people who were already eligible for Part A and B before they turned 65. During the IEP2, you can sign up for a Medicare Advantage or Part D plan. The IEP2 runs for the same seven-month period as the IEP.
What is a SEP in Medicare?
A SEP is when you can make changes to your Medicare Advantage and Prescription Drug coverage when certain events happen in your life. Events include situations such as if you move or lose other insurance coverage. An example is losing health insurance ...
What is the ICEP period?
The ICEP is your first opportunity to choose a Medicare Advantage plan instead of Original Medicare. During the ICEP, you can also sign up for prescription drug coverage. If you enroll in Part B when you turn 65, your ICEP is the same as your IEP.
Why is Medicare enrollment confusing?
Medicare Enrollment Periods can be confusing because different enrollment periods have different dates for various purposes. There are many enrollment periods for people signing up for benefits for the first time. If you’re receiving Social Security or Railroad Retirement benefits when you turn 65, you’ll automatically be enrolled in Medicare.
What is open enrollment for Medicare 2021?
These enrollment periods fall into two categories. First, open enrollment is available to anyone eligible for Medicare. Then, Special Enrollment Periods. If you want to change the coverage you currently have, you can do so during one ...
How long does an OEP last?
Your OEP lasts for six months; you’ll be granted Medicare Supplement Guaranteed Issue Rights. During this time, you can sign up for a Medicare Supplement Plan, also known as Medigap. If you didn’t sign up for a Medicare Advantage or a drug plan during your IEP, the AEP is your next chance to make changes.
How many enrollment periods are there for Medicare?
There are three enrollment periods for people signing up for benefits who are already enrolled in Original Medicare. During open enrollment, you can make changes to your Medicare plans and add additional coverage.
What is an IEP and an ICEP?
What are IEP and ICEP? The IEP and ICEP are both one-time Medicare enrollment periods. For many beneficiaries, these periods happen at the same time. The Medicare Initial Enrollment Period (IEP) is your first opportunity to enroll in Original Medicare, which consists of Part A and Part B and is administered by the federal government.
When does IEP end?
Your IEP begins three months before your birthday month, on May 1. It continues for your birthday month and three months after, ending on November 30. If you enroll in both Original Medicare Part A and Part B during this period, your ICEP also runs from May 1 to November 30, and you can enroll in a Medicare Advantage plan.
How to qualify for ICEP?
How Do I qualify for an ICEP? To trigger an ICEP and join a Medicare Advantage plan, you must have both Medicare Part A and Medicare Part B coverage . Also, your permanent residence must be within the service area of your chosen Medicare Advantage plan. If you don’t enroll in Part B during the IEP, you cannot enroll in a Medicare Advantage plan ...
How long does an IEP last?
Your IEP lasts for seven months, beginning three months before your 65th birthday. If you enroll in Medicare parts A and B during the IEP, then your ICEP runs simultaneously. Some people choose not to enroll in Medicare Part B during their IEP.
What is Medicare OEP?
What is the Medicare OEP? 1 The Medicare Advantage Open Enrollment Period (MAOEP) runs from January 1 through March 31. It allows people currently enrolled in a Medicare Advantage plan to make a one-time change. For example, you could switch to a different Medicare Advantage plan or disenroll from your Medicare Advantage plan and return to Original Medicare. You cannot change from one Part D plan to another. 2 There is also the fall Medicare Open Enrollment Period (OEP) mentioned earlier, which runs from October 15 through December 7 each year. During the OEP, you can join, switch or leave a plan, with changes to coverage beginning on January 1 of the following year.
What is Medicare Advantage?
Private insurance companies sell Medicare Advantage plans that replace your Original Medicare coverage. These options provide at least the same healthcare coverage as Original Medicare. Many people prefer them because they often offer additional benefits, such as prescription drug coverage and wellness benefits.
How long does it take for ICEP to start?
If you enroll in Part B at a later date rather than during the IEP, your ICEP begins three months before your Part B coverage is due to start.
What are the special enrollment periods?
When certain events happen in your life, like if you move or lose other insurance coverage, you may be able to make changes to your Medicare health and drug coverage. These chances to make changes are called Special Enrollment Periods. Rules about when you can make changes and the type of changes you can make are different for each Special Enrollment Period.
How many enrollment periods are there for Medicare Advantage?
There are 2 separate enrollment periods each year. See the chart below for specific dates.
What is the late enrollment penalty for Medicare?
The late enrollment penalty is an amount that’s permanently added to your Medicare drug coverage (Part D) premium. You may owe a late enrollment penalty if at any time after your Initial Enrollment Period is over, there’s a period of 63 or more days in a row when you don’t have Medicare drug coverage or other creditable prescription drug coverage. Creditable prescription drug coverage is coverage (for example, from an employer or union) that’s expected to pay, on average, at least as much as Medicare’s standard prescription drug coverage. If you have a penalty, you’ll generally have to pay it for as long as you have Medicare drug coverage. For more information about the late enrollment penalty, visit Medicare.gov, or call 1‑800‑MEDICARE (1‑800‑633‑4227). TTY users can call 1‑877‑486‑2048.