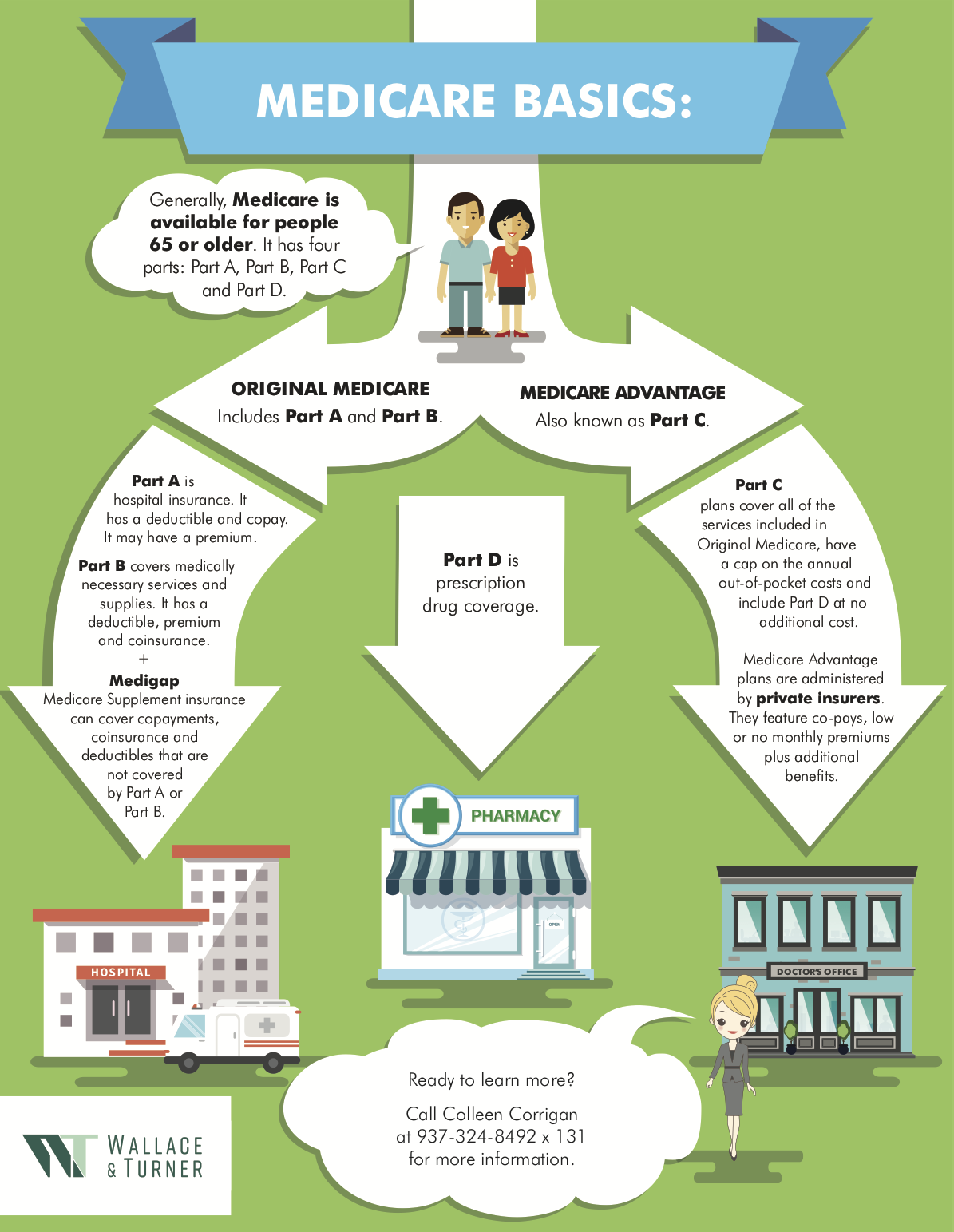
Mental health services, such as individual counseling provided in an outpatient setting, will be covered at 80% of the approved charge with Medicare Part B after the annual deductible ($203 for 2021) is met. You pay the other 20%.
Full Answer
Will Medicare pay for mental health services?
You pay nothing for your yearly depression screening if your doctor or health care provider accepts assignment. After you meet the Part B deductible, you pay 20% of the. Medicare-Approved Amount. In Original Medicare, this is the amount a doctor or supplier that accepts assignment can be paid.
What is the Medicare-approved amount?
the Medicare-approved amount if your health care provider accepts assignment. Under Original Medicare, you pay nothing for opioid use disorder treatment services if you get them from an opioid treatment program who’s enrolled in
Is a psychiatric evaluation covered by Medicare?
Nov 25, 2021 · Mental health services, such as individual counseling provided in an outpatient setting, will be covered at 80% of the approved charge with Medicare Part B after the annual deductible ($203 for 2021) is met. You pay the other 20%.
What is included in this Medicare mental health booklet?
Covered Medicare Fee-for-Service Mental Health Services Medicare may cover these services to support behavioral health and wellness: Alcohol misuse screening and counseling for adults who use alcohol but aren’t dependent; if you detect misuse, Medicare covers up to 4 brief face-to-face counseling sessions per year if patient is

What is Part B in psychiatry?
Part B covers partial hospitalization in some cases. Partial hospitalization is a structured program of outpatient psychiatric services provided to patients as an alternative to inpatient psychiatric care. It’s more intense than the care you get in a doctor’s or therapist’s oce. This type of treatment is provided during the day and doesn’t require an overnight stay.
What is an appeal in Medicare?
An appeal is an action you can take if you disagree with a coverage or payment decision by Medicare, your Medicare health plan, or your Medicare drug plan. If you decide to file an appeal, ask your doctor, health care provider, or supplier for any information that may help your case. Keep a copy of everything you send to Medicare or your plan as part of the appeal.
What is coinsurance in insurance?
Coinsurance—An amount you may be required to pay as your share of the cost for services after you pay any deductibles. Coinsurance is usually a percentage (for example, 20%).
Can mental health problems happen to anyone?
Mental health conditions, like depression or anxiety, can happen to anyone at any time. If you think you may have problems that affect your mental health, you can get help. Talk to your doctor or other health care provider if you have:
Does CMS exclude or deny benefits?
The Centers for Medicare & Medicaid Services (CMS) doesn’t exclude, deny benefits to, or otherwise discriminate against any person on the basis of race, color, national origin, disability, sex, or age in admission to, participation in, or receipt of the services and benefits under any of its programs and activities, whether carried out by CMS directly or through a contractor or any other entity with which CMS arranges to carry out its programs and activities.
Can you get help with Medicare if you have limited income?
If you have limited income and resources, you may be able to get help from your state to pay your Medicare costs (like premiums, deductibles, and coinsurance) if you meet certain conditions.
Does Medicare cover alcohol abuse?
Medicare covers one alcohol misuse screening per year for adults with Medicare (including pregnant women) who use alcohol, but don’t meet the medical criteria for alcohol dependency. If your health care provider determines you’re misusing alcohol, you can get up to 4 brief face-to-face counseling sessions per year (if you’re competent and alert during counseling). You must get counseling in a primary care setting (like a doctor’s oce).
What is the CPT code for mental health?
The most used psychiatric and therapeutic codes include 90791, 90792, 90832, 90834, 90837, 90846, 90847, 90853, and 90839.
How long does Medicare cover IPF?
Medicare covers IPF patients for psychiatric conditions in specialty facilities for 90 days per illness with a 60-day lifetime reserve, and for 190 days of care in freestanding psychiatric hospitals (this 190-day limit doesn’t apply to certified psychiatric units). There are no further benefits once a patient uses 190 days of psychiatric hospital care.
What is the IPF medical record?
The IPF medical records must show treatment level and intensity for each patient a physician or NPP admits to the hospital, among other requirements detailed at 42 CFR Section 482.61.
Is CPT copyrighted?
CPT codes, descriptions and other data only are copyright 2020 American Medical Association. All Rights Reserved. Applicable FARS/HHSAR apply. CPT is a registered trademark of the American Medical Association. Applicable FARS/HHSAR Restrictions Apply to Government Use. Fee schedules, relative value units, conversion factors and/or related components are not assigned by the AMA, are not part of CPT, and the AMA is not recommending their use. The AMA does not directly or indirectly practice medicine or dispense medical services. The AMA assumes no liability for data contained or not contained herein.
Does Medicare cover mental health?
In addition to providing all Medicare Part B covered mental health services, Medicare Advantage plans may offer “additional telehealth benefits” (telehealth benefits beyond what Part B pays), as well as supplemental benefits that aren’t covered under Medicare Parts A or B. For example, these mental health supplemental benefits may address areas like coping with life changes, conflict resolution, or grief counseling, all offered as individual or group sessions.
Does Medicare pay for incident to?
Medicare pays under the “Incident to” provision when the services and supplies comply with state law and meet all these requirements:
What is the Medicare Part B coverage for a clinical psychologist?
Clinical psychologists diagnose and treat mental, emotional, and behavioral disorders – and are one of the health care providers covered by Medicare Part B. Coverage: Medicare pays 80 percent of the Medicare-approved amount. You pay 20 percent of the Medicare-approved amount, the Part B deductible, and coinsurance costs.
What is Medicare Part B?
Coverage: Medicare Part B helps pay for a psychiatric evaluation. Medicare pays 80 percent of the Medicare-approved amount. You pay 20 percent of the approved amount, the Part B deductible, and coinsurance costs.
What percentage of Medicare does a nurse practitioner pay?
Nurse practitioners. Physician assistants. Coverage: Medicare pays 80 percent of the Medicare-approved amount. You pay 20 percent of the Medicare-approved amount, the Part B deductible, and coinsurance costs.
Does Medicare cover marriage counseling?
Medicare does not cover other types of relationship counseling, such as marriage counseling. You’re only covered for mental health services from a licensed psychiatrist, clinical psychologist, or other health care professional who accepts Medicare assignment.
Does Medicare cover depression screening?
Coverage: A yearly depression screening and preventive visit does not cost anything if your doctor or health care provider accepts assignment.
Does Medicare cover mental health?
Medicare Coverage of Mental Health Services. A person’s mental health refers to their state of psychological, emotional, and social well-being – and it’s important to take care of it at every stage of life , from childhood to late adulthood. Fortunately, Medicare beneficiaries struggling with mental health conditions may be covered ...
When is the 2019 Medicare Physician Fee Schedule released?
These provisions are part of the final rule on the 2019 Medicare Physician Fee Schedule and Quality Payment Program, released by CMS in early November. Highlights of the Final Rule include.
What is the final rule for Medicare?
Final Rule on 2019 Medicare Physician Fee Schedule and Quality Payment Program. For 2019, the Centers for Medicare and Medicaid Services (CMS) has reduced administrative burdens on physicians associated with documentation and preserved separate payments for each of the existing levels of evaluation and management ...
What is the AMA RUC?
The American Medical Association (AMA) and its CPT Editorial Panel and Relative Value Scale (RVS) Update Committee (RUC) have paid an important role in this process as it has evolved. The AMA CPT Editorial Panel has established a process where CPT coding proposals are reviewed and if approved referred to the AMA RUC.
Does Medicare update fee schedules?
Back to Medicare. Medicare maintains and updates fee schedules for all health care related costs including physicians, ambulance services, clinical labs, and durable medical equipment. The Medicare Physician Fee Schedule is updated on an annual basis through the rule-making process.
What is Medicare approved amount?
The Medicare-approved amount is the amount that Medicare pays your provider for your medical services. Since Medicare Part A has its own pricing structure in place, this approved amount generally refers to most Medicare Part B services. In this article, we’ll explore what the Medicare-approved amount means and it factors into what you’ll pay ...
What are the services covered by Medicare?
No matter what type of Medicare plan you enroll in, you can use Medicare’s coverage tool to find out if your plan covers a specific service, test, or item. Here are some of the most common Medicare-approved services: 1 mammograms 2 chemotherapy 3 cardiovascular screenings 4 bariatric surgery 5 physical therapy 6 durable medical equipment
What is a non-participating provider?
Nonparticipating provider. A nonparticipating provider accepts assignment for some Medicare services but not all. Nonparticipating providers may not offer discounts on services the way participating providers do. Even if the provider bills Medicare later for your covered services, you may still owe the full amount upfront.
How much is Medicare Part A deductible?
If you have original Medicare, you will owe the Medicare Part A deductible of $1,484 per benefit period and the Medicare Part B deductible of $203 per year. If you have Medicare Advantage (Part C), you may have an in-network deductible, out-of-network deductible, and drug plan deductible, depending on your plan.
What percentage of Medicare deductible is paid?
After you have met your Part B deductible, Medicare will pay its portion of the approved amount. However, under Part B, you still owe 20 percent of the Medicare-approved amount for all covered items and services.
What happens if a provider accepts assignment?
If they are a nonparticipating provider, they may still accept assignment for certain services. However, they can charge you up to an additional 15 percent of the Medicare-approved amount for these services.
What is Medicare Advantage?
Medicare Part B covers you for outpatient medical services. Medicare Advantage covers services provided by Medicare parts A and B, as well as: prescription drugs. dental.