
The Centers for Medicare and Medicaid
Medicaid
Medicaid in the United States is a federal and state program that helps with medical costs for some people with limited income and resources. Medicaid also offers benefits not normally covered by Medicare, including nursing home care and personal care services. The Health Insurance As…
Centers for Medicare and Medicaid Services
The Centers for Medicare & Medicaid Services, previously known as the Health Care Financing Administration, is a federal agency within the United States Department of Health and Human Services that administers the Medicare program and works in partnership with state government…
How to complete required Medicare questionnaire?
It can also include:
- A review of your medical and family history.
- Developing or updating a list of current providers and prescriptions.
- Height, weight, blood pressure, and other routine measurements.
- Detection of any cognitive impairment.
- Personalized health advice.
- A list of risk factors and treatment options for you.
What is Medicare health risk assessment?
in Medicare Advantage, a health risk assessment. Medicare Advantage plans are also required to make a “best effort” to conduct a health assessment annually. Health risk assessments (HRAs) are an objective tool used to collect information on a beneficiary's health status, health risk factors, social determinants of health, and
Is a Medicare wellness exam mandatory?
The Medicare Annual Wellness Visit is not mandatory. It is a medical visit that you can take advantage of voluntarily and free of charge. The wellness visit is intended to keep you in touch with your Medicare doctor and ensure that your doctor can help you with preventive care planning.
What are the components of the Medicare wellness exam?
Required elements for the initial AWV include:
- A self-reported health risk assessment
- Establishment of the beneficiary's medical/family history
- Review of the beneficiary's potential risk factors for mood disorders
- Review of the beneficiary's functional ability and level of safety
- A health assessment within the office
- Establishment of current providers and suppliers of service
Does Medicare require a health assessment every year?
Medicare covers a “Welcome to Medicare” visit and annual “wellness” visits. While both visit types are available to Medicare recipients, recipients aren't required to participate in either visit type to maintain their Medicare Part B coverage.
What does a Medicare wellness check up consist of?
Your visit may include: A review of your medical and family history. A review of your current providers and prescriptions. Height, weight, blood pressure, and other routine measurements.
What is included in a Medicare health risk assessment?
What is included in the Health Risk Assessment? The HRA typically includes a series of questions about health conditions, lifestyle choices, mental health, and family health history. These questions are intended to identify potential risk factors that could be detrimental to the patient's health.
How often will Medicare pay for a physical exam?
En español | Medicare does not pay for the type of comprehensive exam that most people think of as a “physical.” But it does cover a one-time “Welcome to Medicare” checkup during your first year after enrolling in Part B and, later on, an annual wellness visit that is intended to keep track of your health.
What is the difference between a Medicare wellness exam and a physical?
There is a difference between an “annual wellness visit” and an “annual physical exam.” One is focused more on preventing disease and disability, while the other is more focused on checking your current overall health.
What is not included in a wellness visit?
Your insurance for your annual wellness visit does not cover any discussion, treatment or prescription of medications for chronic illnesses or conditions, such as high blood pressure, high cholesterol or diabetes.
Does Medicare require a health risk assessment?
The Affordable Care Act directed the Centers for Medicare & Medicaid Services (CMS) to require that a health risk assessment (HRA) be completed as part of the Medicare AWV.
Is a health risk assessment required?
Some populations may be required to take an HRA based on their care, such as Medicare and Medicaid recipients. Medicare recipients are required to complete an HRA by the Centers for Medicare & Medicaid Services (CMS), as part of the Medicare Annual Wellness Visit (AWV).
What are health risk assessments used for?
A health risk assessment (also known as a health risk appraisal) is an instrument used to collect health information, typically coupled with a process that includes biometric testing to assess an individual's health status, risks, and habits. Alone, an HRA can do little to improve health or cut costs.
What is the difference between an annual physical and a wellness visit?
An annual physical typically involves an exam by a doctor along with bloodwork or other tests. The annual wellness visit generally doesn't include a physical exam, except to check routine measurements such as height, weight and blood pressure.
What is a Medicare wellness exam for a woman?
A Medicare Wellness Visit, also called a wellness exam, is an assessment of your overall health and well-being. The primary purpose is prevention – either to develop or update your personalized prevention plan.
Does Medicare cover routine blood work?
Does Medicare Cover Blood Tests? Medicare covers medically necessary blood tests ordered by a physician based on Medicare guidelines. Medicare Advantage (Part C) plans may cover more tests, depending on the plan. There is no separate fee for blood tests under original Medicare.
How many days does Medicare require SNF to do assessments?
Medicare also requires the SNF to record assessments done on days 14, 30, 60, and 90 of your covered stay . The SNF must do this until you're discharged or you've used all 100 days of SNF coverage in your. Benefit Period.
What is the benefit period for Medicare?
Benefit Period. The way that Original Medicare measures your use of hospital and skilled nursing facility (SNF) services. A benefit period begins the day you're admitted as an inpatient in a hospital or SNF. The benefit period ends when you haven't gotten any inpatient hospital care (or skilled care in a SNF) for 60 days in a row.
How to assess a person's mental health?
An assessment includes collecting information about: 1 Your current physical and mental condition 2 Your medical history 3 Medications you're taking 4 How well you can do activities of daily living (like bathing, dressing, eating, getting in and out of bed or a chair, moving around, and using the bathroom) 5 Your speech 6 Your decision-making ability 7 Your physical limitations (like problems with your hearing or vision, paralysis after a stroke, or balance problems)
What is a health goal?
A health goal is the expected result of your treatment, like being able to walk a certain distance or to climb stairs. Your daily assessments and skilled care start the day you arrive at the SNF. Medicare requires that your assessments be recorded periodically.
What is part B of a care plan?
Cognitive assessment & care plan services. Part B covers certain doctors' services, outpatient care, medical supplies, and preventive services. covers a visit with your regular doctor or a specialist to do a full review of your cognitive function, establish or confirm a diagnosis like dementia, including Alzheimer's disease, ...
Does Medicare cover cognitive impairment?
Medicare covers a separate visit to do a more thorough review.
What is the purpose of a Medicare wellness exam?
The purpose of the Medicare annual wellness exam is to develop or update your personalized prevention plan and perform a health risk assessment.
What is Medicare annual wellness exam?
The Medicare annual wellness exam is a free health benefit that includes a personalized prevention plan. Taking advantage of this important benefit can help beneficiaries take proactive steps to stay healthy.
Why do we do wellness exams?
That’s because the wellness exam gives you an opportunity to get personalized health advice. You can talk about any healthcare concerns you may have, ask questions about your medications, talk about changes to your diet or exercise routine and more.
Is the annual wellness exam covered by Medicare?
However, you may still have questions about the purpose of the exam and how it can help you. For instance, it’s important to know that the annual wellness exam is covered in full by Medicare, but it’s not the same as a routine physical exam, which isn’t covered by Medicare. This article answers some of the most common questions about ...
What is the purpose of Medicare health assessment?
The purpose of the Medicare health assessment is to identify heath needs and risk factors so beneficiaries can be directed to appropriate care, ultimately improving outcomes and reducing costs. The Center for Disease Control and Prevention defined the minimum requirements for the health risk assessment in “ Framework for Patient-Centered Health ...
What are the requirements for a health risk assessment?
The Center for Disease Control and Prevention defined the minimum requirements for the health risk assessment in “ Framework for Patient-Centered Health Risk Assessments ,” to include: 1 Demographic data and personal health history 2 Self-assessment of health status 3 Psychosocial risks, such as stress, depression, and pain 4 Behavioral risks, such as tobacco and alcohol use, nutrition, and physical activity 5 Activities of Daily Living (ADLs), including dressing, bathing, and walking 6 Instrumental ADLs, including shopping, housekeeping, managing own medications, and handling finances
What are the risks of self assessment?
Self-assessment of health status. Psychosocial risks, such as stress, depression, and pain. Behavioral risks, such as tobacco and alcohol use, nutrition, and physical activity. Activities of Daily Living (ADLs), including dressing, bathing, and walking.
What is an assessment tool?
Evaluators will use an assessment tool to determine whether the applicant needs long-term care, and at which “level of care” and setting those services should be provided (e.g., in a nursing home or assisted living facility, or community- or home-based care).
Who evaluates Medicaid long term care?
Applicants for Medicaid long-term care coverage have to undergo an assessment by medical doctors, social workers, or other evaluators designated by their state’s Medicaid agency. This evaluation may consider the medical, cognitive, mental health, and functional issues an applicant has. Evaluators will use an assessment tool to determine whether ...
What is level of care in nursing home?
The “level of care” is the setting in which an individual needs medical or long-term care services. In most states, applicants who require a nursing home “level of care” have medical conditions or functional limitations that result in being a danger to oneself.
Does Medicare cover long term care?
Since Medicare does not cover most long-term care needs, many older Americans who need long-term care services (ie, custodial care, as opposed to medical care) find themselves turning to Medicaid, which does cover long-term care for eligible enrollees.
What is Medicare annual wellness visit?
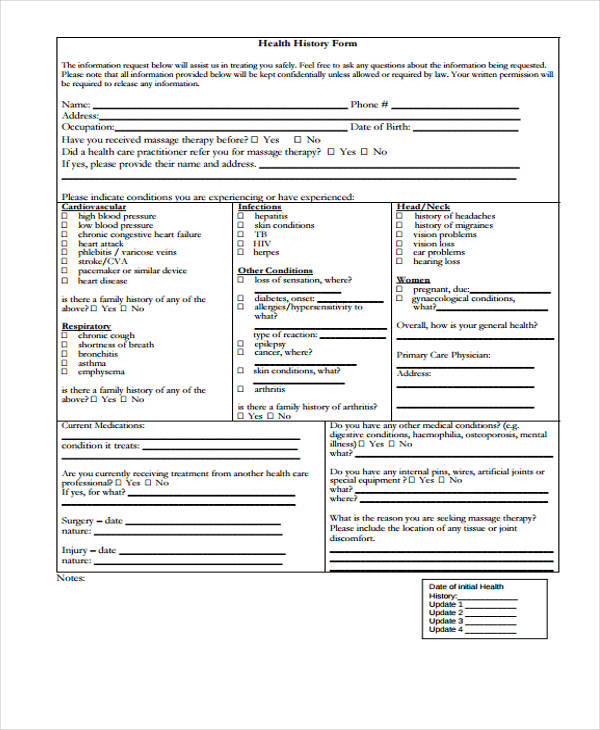
What is the Medicare Annual Wellness Visit? When you attend Medicare annual wellness visit, your physician will have you complete a “Health Risk Assessment”. This is a fancy term for a health questionnaire.
How often is a wellness visit required for Medicare?
This is only once, within your first 12 months of Part B. As discussed above, the Medicare Annual Wellness Visit is an exam that you receive if you’ve been a Medicare recipient for more than 12 months, and this appointment is once per year. The Annual Wellness Visit is a health evaluation, rather than a physical examination.
What is physical exam?
A physical exam can include some of the components of the wellness visit (vitals check, neurological assessment), but not all. These appointments may include abdominal assessments, head and neck exams, lung exams, heart assessments, etc. AWVs are great for Advance Care Planning and Directives, checking one’s level of safety and cognitive function, ...
How long do you have to carry Medicare Part B?
Your annual visit coverage is under your Medicare Part B. You should be aware that you must carry Part B for more than 12 months to qualify for this visit.
Can you get an annual wellness visit with Medicare?
The Annual Wellness Visit is a health evaluation, rather than a physical examination. Furthermore, you can’t receive an AWV during the same calendar year as your Welcome to Medicare preventative visit.
What is Medicare assignment?
Medicare assignment is a fee schedule agreement between Medicare and a doctor. Accepting assignment means your doctor agrees to the payment terms of Medicare. Doctors who accept Medicare are either a participating doctor, non-participating doctor, or they opt-out. When it comes to Medicare’s network, it’s defined in one of three ways.
What does it mean when you sign a contract with Medicare?
Once you sign a contract, it means that you accept the full amount on your own, and Medicare can’t reimburse you. Signing such a contract is giving up your right to use Medicare for your health purposes.
What is assignment of benefits?
The assignment of benefits is when the insured authorizes Medicare to reimburse the provider directly. In return, the provider agrees to accept the Medicare charge as the full charge for services. Non-participating providers can accept assignments on an individual claims basis. On item 27 of the CMS-1500 claim form non participating doctors need ...
How to avoid excess charges on Medicare?
You can avoid excess charges by visiting a provider who accepts Medicare & participates in Medicare assignment. If your provider does not accept Medicare assignment, you can get a Medigap plan that will cover any excess charges. Not all Medigap plans will cover excess charges, but some do.
What happens if a provider refuses to accept Medicare?
However, if a provider is not participating, you could be responsible for an excess charge of 15% Some providers refuse to accept Medicare payment altogether; if this is the situation, you’re responsible for 100% of the costs.
Can you pay 100% of Medicare?
You could pay 100% out of pocket, then wait for Medicare reimbursement. Please keep in mind, there’s no reimbursement guarantee. Then there are doctors who opt out of Medicare charges. This means you pay 100%. Unlike doctors that accept assignment, these doctors don’t set their fees to Medicare standards.
Do doctors accept Medicare Advantage?
Do Most Doctors Accept Medicare Advantage? Unlike a Medicare Supplement, a Medicare Advantage Plan replaces your Original Medicare. Your health coverage is the insurance company and you don’t have the freedom to simply go to any doctor. Advantage plans are subject to plan networks and rules for services.
