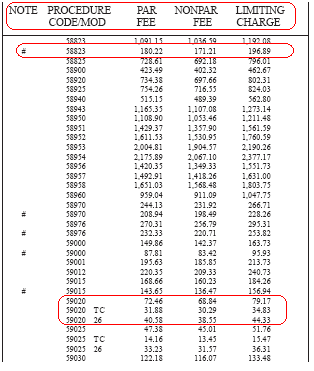
99213 Reimbursement Rates – Medicare 2022: $100.57 (Source) Other Medicare rates for CPT code 99213 are $81.62, in WA in King County, so it depends on the locality.
| 99201 | $35.96 $43.6 |
|---|---|
| 99212 | $37.17 $43.1 |
| 99213 | $58.89 $72.7 |
| 99214 | $88.33 $107.2 |
| 99215 | $118.95 $144.8 |
What is medical billing code 99213?
In Medical billing CPT code 99213 is the most used CPT code . Here i have given the definition and rules for when submitting with other CPT codes such as injection, surgery and vaccination and other CPT codes. CPT CODE – 99213 Established patient, moderate clinic visit.
What does the medical procedure code 99213 mean?
What does CPT code 99213 mean? CPT Code 99213: Office or other outpatient visit for the evaluation and management of an established patient, which requires a medically appropriate history and/or examination and a low level of medical decision making.
What is Procedure Code 99213?
- Low for code 99213
- Moderate for 99214
- High for 99215
What is the Medicare fee schedule?
- Provided a 3.75% increase in MPFS payments for CY 2021
- Suspended the 2% payment adjustment (sequestration) through March 31, 2021
- Reinstated the 1.0 floor on the work Geographic Practice Cost Index through CY 2023
- Delayed implementation of the inherent complexity add-on code for evaluation and management services (G2211) until CY 2024
What Does Medicare pay for a 99213?
A 99213 pays $83.08 in this region ($66.46 from Medicare and $16.62 from the patient). A 99214 pays $121.45 ($97.16 from Medicare and $24.29 from the patient). For new patient visits most doctors will bill 99203 (low complexity) or 99204 (moderate complexity) These codes pay $122.69 and $184.52 respectively.
What is the average reimbursement for a 99213?
99213 Reimbursement Rates: – Medicaid:CPT CodeService TimeRate9921210 minutes$31.369921315 minutes$43.239921425 minutes$66.809921540 minutes$99.95
Is the Medicare 2021 fee schedule available?
The CY 2021 Medicare Physician Fee Schedule Final Rule was placed on display at the Federal Register on December 2, 2020. This final rule updates payment policies, payment rates, and other provisions for services furnished under the Medicare Physician Fee Schedule (PFS) on or after Jan. 1, 2021.
Is the 2020 Medicare fee schedule available?
The Centers for Medicare and Medicaid Services (CMS) has released the 2020 Medicare Physician Fee Schedule final rule addressing Medicare payment and quality provisions for physicians in 2020. Under the proposal, physicians will see a virtually flat conversion factor on Jan. 1, 2020, going from $36.04 to $36.09.
What is the RVU for 99213 in 2021?
0.97 1.3How the E/M code RVU increases could affect family physicians' payCode2020 work RVUs2021 work RVUs992120.480.7992130.971.3992141.51.92992152.12.86 more rows•Jan 18, 2021
Is CPT 99213 covered by Medicare?
For example, a 67-year-old established patient presents for a covered service, such as an office visit for a chronic illness (e.g., 99213)....SERVICE.SERVICECHARGE AMOUNT99213- office visit (covered service)-$130.00Patient billable amount for 99397$71.001 more row
Where can I download Medicare fee schedule?
you may wish to access the Medicare Physician Fee Schedule Database (MPFSDB)/Relative Value File on the CMS website. CMS offers the complete file in several different formats and provides a single code look up. Access the Medicare Physician Fee Schedule Database (MPFSDB)/Relative Value File on the CMS website.
Did Medicare reimbursement go down in 2022?
A law recently passed by Congress wiped out most of a nearly 10% cut in Medicare payments that family physicians would have otherwise incurred in 2022.
What is the Medicare fee schedule?
A fee schedule is a complete listing of fees used by Medicare to pay doctors or other providers/suppliers. This comprehensive listing of fee maximums is used to reimburse a physician and/or other providers on a fee-for-service basis.
What are Medicare premiums for 2021?
The Centers for Medicare & Medicaid Services (CMS) has announced that the standard monthly Part B premium will be $148.50 in 2021, an increase of $3.90 from $144.60 in 2020.
What is a Medicare fee for 2022?
You have Medicare and Medicaid, and Medicaid pays your premiums. (Your state will pay the standard premium amount of $170.10 in 2022.)
What is the 2022 Medicare conversion factor?
$34.6062On Dec. 16, the Centers for Medicare and Medicaid Services (CMS) announced an updated 2022 physician fee schedule conversion factor of $34.6062, according to McDermott+Consulting.
How long does a CPT 99214 take?
Current 99214 CPT Code Description includes the comment note “Typically, 25 minutes are spent face-to-face with the patient and/or family.”. So as per description notes the provider spends approximately 25 minutes face-to-face with the patient for billing CPT 99214.
When did the CPT change?
This change is retroactively effective to July 1, 2016.
What is GPCI in RVU?
2) Geographic Practice Cost Indices (GPCIs) Each of the three RVUs are adjusted to account for geographic variations in the costs of practicing medicine in different areas within the country. These adjustments are called GPCIs, and each kind of RVU component has a corresponding GPCI adjustment.
How to determine the payment rate for a particular service?
To determine the payment rate for a particular service, the sum of the geographically adjusted RVUs is multiplied by a CF in dollars. The statute specifies the formula by which the CF is updated on an annual basis.
How many codes are there in Medicare Part B?
Medicare Part B pays for physician services based on the Medicare PFS, which lists the more than 7,000 unique codes and their payment rates. Physicians’ services include:
When did CMS change the definition of a new patient?
The CPT definition of a new patient underwent subtle changes in 2012. Unfortunately, CMS did not change their definition to stay aligned with these changes. This difference in language has caused great confusion for many qualified healthcare practitioners trying to stay compliant with the complex rules and regulations of E&M.
Can 99214 be used for billing?
CPT Code 99214, if billed correctly, can increase revenue for the practice. By only using CPT code 99212 and CPT Code 99213 many providers are losing thousands of dollars in legitimate revenue yearly. It can be avoided with the correct billing of the 99214 E/M Code.
When will the CPT code 99201 be revised?
On Nov. 1, 2019, CMS finalized revisions to the evaluation and management (E/M) office visit CPT codes 99201-99215. These revisions will go into effect on Jan. 1, 2021. They build on the goals of CMS and providers to reduce administrative burden and put “patients over paperwork” thereby improving the health system.
When will CMS change the physician fee schedule?
CMS has announced changes to the physician fee schedule for 2021. On December 2, 2020, the Centers for Medicare and Medicaid Services (CMS) published its final rules for the Part B fee schedule, referred to as the Physician Fee Schedule (PFS). Substantial changes were made, with some providers benefiting more than others, ...
How much is Medicare reimbursement enhanced?
As a result, depending on physician performance within this program, Medicare reimbursements can be enhanced or penalized by up to 9%, although there is a two-year delay in this application (e.g. provider performance in 2021 will lead to the enhancement or penalty in 2023).
How many categories of requests for additional services are there?
CMS has categorized the request for additional services in three different categories. The explanation of each as well as the additions are as follows:
What is the definition of time in Medicare?
This now represents total physician/qualified health care professional (QHP) time on the date of service. This use of “date-of-service” time aligns with Medicare’s attempt to better recognize work involved with non-face-to-face services like care coordination. These minimum time definitions would only apply when code selection is primarily based on time and not MDM.
When will CMS update the E/M code?
These revisions build on the goals of CMS and the provider community to reduce administrative burden and put “patients over paperwork.” These revisions will be effective Jan. 1, 2021 .
Does CMS use work time?
CMS uses a formula to derive the annual physician fee schedules and the “work-time” relative value units have increased significantly for select evaluation and management codes ( e.g. office visits). These now reflect a global period related to office visits, including incremental calls and prescription refill times. In order for this change to be revenue neutral, a known regulatory challenge, CMS had to reduce the “conversion factor” significantly. However, with the signing of the Omnibus and Covid Relief bill, this issue has significantly been reduced while maintaining the other, positive changes made to office visit reimbursement levels.
What is Medicare fee schedule?
The organization that manages the Medicare program, Centers for Medicare & Medicaid Services (CMS), describes the Medicare fee schedule as a comprehensive list of maximum fees used by Medicare to reimburse physicians, other healthcare providers and suppliers.
What is fee for service Medicare?
Medicare fee-for-service payments are for services rendered by doctors, ambulances and clinical laboratories. The schedule, which is developed by CMS, also includes payments for durable medical equipment (DME), prosthetics, orthotics and supplies. Following are two examples of fee schedules.
What percentage of Medicare deductible do you pay when you visit a doctor?
After meeting the Part B deductible, patients will usually pay 20% of the Medicare-approved amount for most services delivered by a physician.
What is AFS in Medicare?
The Ambulance Fee Schedule (AFS) is a national fee schedule for ambulance services provided as part of the Medicare benefits under the provisions of Part B. These services include volunteer, municipal, private, independent and institutional providers as well as skilled nursing facilities.
When is the Medicare Physician Fee Schedule Final Rule?
The Medicare Physician Fee Schedule Final Rule for the calendar year of 2020 has been displayed at the Federal Register since November 1, 2019. It includes payment policies, rates and other elements for services provided under the Medicare Physician Fee Schedule (MPFS).
Does CMS have a regulation change?
CMS sometimes enacts regulatory changes in payment rules as a result of reevaluation to reduce burdensome requirements with regard to supervision, scope and licensing. In response to the President’s Executive Order on “Protecting and Improving Medicare for Our Nation’s Seniors,” EO # 13890, reforms have been proposed, and some have been implemented. For example, physician supervision for services rendered by Physician Assistants has been redefined. This allows therapist assistants to administer therapy under the Medicare benefits for home health care and lowers the minimum oversight required for hospital outpatient therapy.
When is the Medicare Physician Fee Schedule 2020?
This final rule updates payment policies, payment rates, and other provisions for services furnished under the Medicare Physician Fee Schedule (PFS) on or after Jan. 1, 2020.
When will Medicare start charging for PFS 2022?
The CY 2022 Medicare Physician Fee Schedule Proposed Rule with comment period was placed on display at the Federal Register on July 13, 2021. This proposed rule updates payment policies, payment rates, and other provisions for services furnished under the Medicare Physician Fee Schedule (PFS) on or after January 1, 2022.
What is the MPFS conversion factor for 2021?
CMS has recalculated the MPFS payment rates and conversion factor to reflect these changes. The revised MPFS conversion factor for CY 2021 is 34.8931. The revised payment rates are available in the Downloads section of the CY 2021 Physician Fee Schedule final rule (CMS-1734-F) webpage.
What is the calendar year 2021 PFS?
The calendar year (CY) 2021 PFS proposed rule is one of several proposed rules that reflect a broader Administration-wide strategy to create a healthcare system that results in better accessibility, quality, affordability, empowerment, and innovation.
When will CMS issue a correction notice for 2021?
On January 19, 2021, CMS issued a correction notice to the Calendar Year 2021 PFS Final Rule published on December 28, 2020, and a subsequent correcting amendment on February 16, 2021. On March 18, 2021, CMS issued an additional correction notice to the Calendar Year 2021 PFS Final Rule. These notices can be viewed at the following link:
What is the 2020 PFS rule?
The calendar year (CY) 2020 PFS final rule is one of several rules that reflect a broader Administration-wide strategy to create a healthcare system that results in better accessibility, quality, affordability, empowerment, and innovation.
When will Medicare change to MPFS?
On December 27, the Consolidated Appropriations Act, 2021 modified the Calendar Year (CY) 2021 Medicare Physician Fee Schedule (MPFS):