In South Carolina, applicants can qualify for Medicaid
Medicaid
Medicaid in the United States is a federal and state program that helps with medical costs for some people with limited income and resources. Medicaid also offers benefits not normally covered by Medicare, including nursing home care and personal care services. The Health Insurance As…
What is the Medicare savings program in South Carolina?
6 rows · You can also enroll in Medicare Advantage Plans if you have End-Stage Renal Disease (ESRD) ...
Which states have the highest average Medicare Advantage premiums?
Oct 04, 2020 · Income eligibility: The income limit is $1,063 a month if single and $1,437 a month if married. Asset limits: The asset limit is $7,860 if single and $11,800 if married. These income and asset limits are the same as for the QMB program, meaning QMB enrollees receive full Medicaid benefits in South Carolina.
What is the highest income to qualify for Medicaid in DC?
Nov 16, 2020 · Nationwide, average per beneficiary Original Medicare spending was $10,096 per enrollee, so Medicare spending in South Carolina was lower than the national average. On the ends of the spectrum, Louisiana had the highest average per-beneficiary Original Medicare costs, at $11,932, while Hawaii had the lowest, at just $6,971.
How much does Medicare Part C cost in each state?
Apr 16, 2022 · In 2022, there 96 Medicare Advantage Plans available in South Carolina. 100% of the total Medicare population in South Carolina has access to a Medicare Advantage Plan with a $0 monthly premium in 2022. In 2022, the average monthly premium for a Medicare Advantage Plan in South Carolina is $11.66, a decrease from $12.13 in 2021.
What is the maximum income to qualify for Medicare in South Carolina?
What is the highest income to qualify for Medicare?
Who qualifies for Medicare in SC?
What is the highest income to qualify for Medicaid?
The Federal Poverty Level is determined by the size of a family for the lower 48 states and the District of Columbia. For example, in 2022 it is $13,590 for a single adult person, $27,750 for a family of four and $46,630 for a family of eight.Mar 26, 2022
What income is used to determine Medicare premiums 2021?
Does your income affect how much you pay for Medicare?
What are the 4 types of Medicare?
- Part A provides inpatient/hospital coverage.
- Part B provides outpatient/medical coverage.
- Part C offers an alternate way to receive your Medicare benefits (see below for more information).
- Part D provides prescription drug coverage.
How much does Medicare cost in SC?
| People enrolled in Original Medicare | Average plan cost | Annual state spending per beneficiary |
|---|---|---|
| 733,031 | Plan A: $0 to $499 per month* Plan B: $170.10 per month** | $9,601 |
How do I qualify for dual Medicare and Medicaid?
How are Medicare premiums calculated?
How much money can you have in the bank on Medicaid?
What is the monthly income to qualify for Medi-Cal?
Does South Carolina help with my Medicare premiums?
Many Medicare beneficiaries who struggle to afford the cost of Medicare coverage are eligible for help through a Medicare Savings Program (MSP). In...
Who's eligible for Medicaid for the aged, blind and disabled in South Carolina?
Medicare covers a great number services – including hospitalization, physician services, and prescription drugs – but Original Medicare doesn’t cov...
Where can Medicare beneficiaries get help in South Carolina?
Insurance Counseling Assistance and Referrals for Elders (I-Care) You can receive free Medicare counseling by contacting the Insurance Counseling A...
Where can I apply for Medicaid in South Carolina?
South Carolina’s Medicaid program is overseen South Carolina Department of Health and Human Services (SCDHHS). You can apply for Medicaid ABD or an...
What is Medicare Savings Program in South Carolina?
Many Medicare beneficiaries who struggle to afford the cost of Medicare coverage are eligible for help through a Medicare Savings Program (MSP). In South Carolina, these programs pay for Medicare Part B premiums, Medicare Part A and B cost-sharing, and – in some cases – Part A premiums. Qualified Medicare Beneficiary (QMB): The income limit is ...
What is the income limit for Medicare?
Qualified Medicare Beneficiary (QMB): The income limit is $1,063 a month if single and $1,437 a month if married. QMB pays for Part A and B cost sharing, Part B premiums, and – if a beneficiary owes them – it also pays their Part A premiums. All QMB enrollees also receive full Medicaid benefits in South Carolina.
What is a ship in Medicare?
The SHIP can help beneficiaries enroll in Medicare, compare and change Medicare Advantage and Part D plans, and answer questions about state Medigap protections. Counselors may also be able to provide referrals for home care agencies or long-term care services. You can also access SHIP services through your Area Agency on Aging (AAA), which you can find by entering your zip code on this website.
What is the income limit for a QMB in South Carolina?
Specified Low-Income Medicare Beneficiary (SLMB): The income limit is from QMB levels up to $1,276 a month if single and $1,724 a month if married. SLMB pays for Part B premiums. Qualified Individuals (QI): The income limit is from SLMB levels up to $1,436 a month ...
How much does a spouse need to keep for Medicaid in South Carolina?
Spousal impoverishment rules in South Carolina allow spouses who don’t have Medicaid to keep a Minimum Monthly Maintenance Needs Allowance that is between $2,155 and $3,216 per month. South Carolina requires Medicaid LTSS applicants to have a home equity interest of $595,000 or less.
What assets are not counted in Medicaid?
Certain assets are never counted, including many household effects, family heirlooms, certain prepaid burial arrangements, and one car. Medicaid long-term care enrollees also can’t have more than $595,000 in home equity.
What is the income limit for a single person?
Income limits: The income limit is $2,349 a month if single and $4,698 a month if married (and both spouses are applying).
What percentage of South Carolina residents are on Medicare?
That’s about 21 percent of South Carolina’s population enrolled in Medicare, compared with about 19 percent of the United States population enrolled in Medicare. People become eligible for Medicare either due to their age (turning 65) or due to a disability. In South Carolina, 17 percentof Medicare beneficiaries were eligible due ...
How many people are on medicare in South Carolina?
As of September 2020, there were 1,102,905 people enrolled in Medicare in South Carolina. That’s about 21 percent of South Carolina’s population enrolled in Medicare, compared with about 19 percent of the United States population enrolled in Medicare.
What is the South Carolina Department of Insurance?
The South Carolina Department of Insurance can provide customer service and assistance with a wide range of insurance-related issues. The Department is responsible for regulating and overseeing Medigap insurers, and also licenses the insurers that sell Medicare Advantage and Part D plans in the state (but most regulatory oversight of Advantage and Part D plans is conducted at the federal level, by CMS). The South Carolina Department of Insurance has a resource called “ Making sense of health insurance after retirement, ” which provides some useful information to people with Medicare and people who aren’t yet eligible for Medicare.
What is Medicare Rights Center?
The Medicare Rights Center is a nationwide service that can provide a wide range of information and assistance related to Medicare enrollment, eligibility, and benefits.
How much is Medicare Part D in South Carolina in 2021?
For 2021, there are 29 stand-alone Medicare Part D plan options for sale in South Carolina, with premiums that range from about $7 to $205/month.
How many Medicare Advantage plans are there in South Carolina?
There are Medicare Advantage plans for sale in all 46 countiesin South Carolina in 2020, with plan availability ranging from 29 plans in Darlington County to 66 in Greenville County.
When is Medicare Advantage open enrollment?
People who are already enrolled in Medicare Advantage plans also have access to a Medicare Advantage open enrollment period (January 1 to March 31) during which they can switch to any other Medicare Advantage plan that offers service in their area, or drop their Medicare Advantage plan and enroll in Original Medicare instead.
What are the different types of Medicare Advantage plans in South Carolina?
There are four main plan types in South Carolina’s Medicare Advantage program, including HMOs, PPOs, PFFS plans, and SNPs. Before signing up for a plan, it’s important to find one that has affordable monthly premiums and copays and includes coverage for services you’re most likely to use. Some plans limit you to in-network providers, so if you don’t want to change primary care doctors, you may want to review a plan’s network before enrolling.
What are the rules for Medicare Advantage Plan?
Depending on which Medicare Advantage Plan you select, you may be required to follow certain rules, such as choosing a primary care doctor, getting a referral to see a specialist, or only getting care from in-network providers. Cost-sharing responsibilities, such as premiums, deductibles, copays, and maximum out-of-pocket limits vary. In most cases, your premium will be at least as high as the Original Medicare Part B premium, and it may be higher if you have additional benefits, such as vision or prescription drug coverage.
When is Medicare open enrollment?
Medicare Advantage Open Enrollment Period: This period runs from January 1 through March 31 and is exclusively for Medicare Advantage enrollees. During this time, you can switch to a different Medicare Advantage Plan or back to Original Medicare one time.
When does the enrollment period start for Medicare?
Initial Enrollment Period: This period opens when you first become eligible for Medicare. If you’re newly eligible because you’re turning 65, this period begins three months before your birth month, includes your birth month, and closes three months after.
Does South Carolina have Medicare Advantage?
The South Carolina Department of Insurance helps you compare and shop for Medicare Advantage Plans by providing you with information regarding your coverage choices, telehealth benefits, when you can sign up for a plan, and whether your policy covers you when you’re traveling . The site offers answers to frequently asked questions about Medicare Supplement Insurance, Medicare Advantage Plans, and prescription drug coverage.
What is Medicare Savings Program?
A Medicare Savings Program (MSP) can help pay deductibles, coinsurance, and other expenses that aren’t ordinarily covered by Medicare. We’re here to help you understand the different types of MSPs. Below, we explain who is eligible for these programs and how to get the assistance you need to pay for your Medicare.
How many types of MSPs are there?
There are four kinds of MSPs. Each type of MSP is tailored to different needs and circumstances. Qualified Medicare Beneficiary (QMB) Programs pay most of your out-of-pocket costs. These costs include deductibles, copays, coinsurance, and Part B premiums. A QMB will also pay the premium for Part A if you haven’t worked 40 quarters.
Do you have to have limited resources to qualify for an MSP?
In addition to the income limits, you must have limited resources to qualify for an MSP.
Does Medicare savers have a penalty?
Also, those that qualify for a Medicare Savings Program may not be subject to a Part D or Part B penalty. Although, this depends on your level of extra help and the state you reside in. Call the number above today to get rate quotes for your area.
What does 0% mean on Medicaid?
If “0%” appears, that means individuals may not qualify for Medicaid in that state based on income alone and must meet other criteria, such as being pregnant or disabled.
How many states do not grant Medicaid?
There are 13 states that do not grant Medicaid access to individuals based on income alone.
How long does it take to get approved for medicaid?
Contact your state Medicaid program in order to apply for Medicaid. Applications are generally reviewed and approved within 90 days and typically are reviewed sooner.
Can you have both Medicare and Medicaid?
If you qualify for both Medicare and Medicaid, you are considered “dual eligible.” In this case, you may qualify for a certain type of Medicare Advantage plan called a Dual Eligible Special Needs Plan (D-SNP). D-SNPs are designed to meet the specific needs of people who have Medicaid and Medicare.
Does each state have its own medicaid program?
Each state runs its own Medicaid programs with its own set of qualifying criteria.
Is Medicaid a federal program?
While Medicaid is a federal program, eligibility requirements can be different in each state.
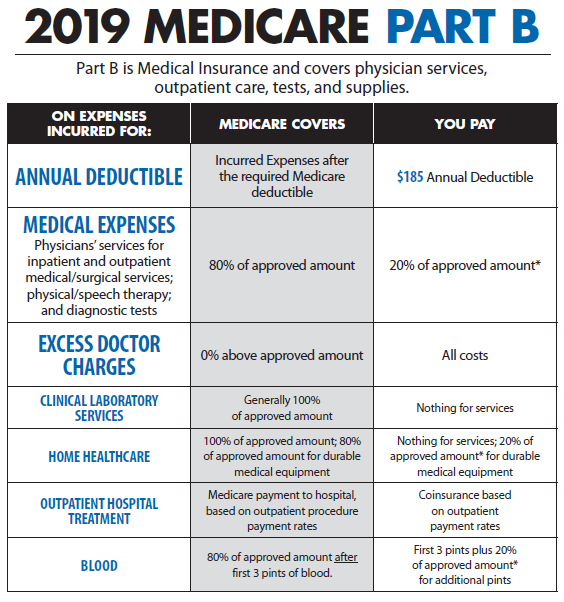
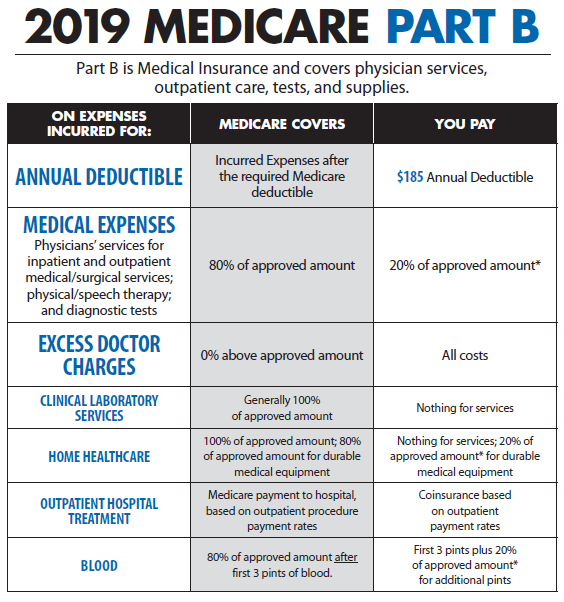
How much does Medicare pay for Part B?
For Part B-covered services, you usually pay 20% of the Medicare-approved amount after you meet your deductible. This is called your coinsurance. You pay a premium (monthly payment) for Part B. If you choose to join a Medicare drug plan (Part D), you’ll pay that premium separately.
What are the extra benefits that Medicare doesn't cover?
Plans may offer some extra benefits that Original Medicare doesn’t cover—like vision, hearing, and dental services.
What happens if you don't get Medicare?
If you don't get Medicare drug coverage or Medigap when you're first eligible, you may have to pay more to get this coverage later. This could mean you’ll have a lifetime premium penalty for your Medicare drug coverage . Learn more about how Original Medicare works.
What is Medicare Supplement Insurance?
You can get a Medicare Supplement Insurance (Medigap) policy to help pay your remaining out-of-pocket costs (like your 20% coinsurance). Or, you can use coverage from a former employer or union, or Medicaid.
What is Medicare Advantage Plan?
Medicare Advantage Plan (Part C) A type of Medicare health plan offered by a private company that contracts with Medicare. Medicare Advantage Plans provide all of your Part A and Part B benefits, excluding hospice. Medicare Advantage Plans include: Health Maintenance Organizations. Preferred Provider Organizations.
What is the original Medicare?
Original Medicare. Original Medicare is a fee-for-service health plan that has two parts: Part A (Hospital Insurance) and Part B (Medical Insurance). After you pay a deductible, Medicare pays its share of the Medicare-approved amount, and you pay your share (coinsurance and deductibles). (Part A and Part B) or a.
Does Medicare Advantage cover prescriptions?
Most Medicare Advantage Plans offer prescription drug coverage. . Some people need to get additional coverage , like Medicare drug coverage or Medicare Supplement Insurance (Medigap). Use this information to help you compare your coverage options and decide what coverage is right for you.
When did Medicare start providing prescription drugs?
Since January 1, 2006, everyone with Medicare, regardless of income, health status, or prescription drug usage has had access to prescription drug coverage. For more information, you may wish to visit the Prescription Drug Coverage site.
How long do you have to be on disability to receive Social Security?
You have been entitled to Social Security or Railroad Retirement Board disability benefits for 24 months. ( Note: If you have Lou Gehrig's disease, your Medicare benefits begin the first month you get disability benefits.)
What is the second most popular Medicare plan?
Medigap Plan G is, in fact, the second-most popular Medigap plan. 17 percent of all Medigap beneficiaries are enrolled in Plan G. 2. The chart below shows the average monthly premium for Medicare Supplement Insurance Plan G for each state in 2018. 3.
Which states have the lowest Medicare premiums?
Florida, South Carolina, Nevada, Georgia and Arizona had the lowest weighted average monthly premiums, with all five states having weighted average plan premiums of $17 or less per month. The highest average monthly premiums were for Medicare Advantage plans in Massachusetts, North Dakota and South Dakota. *Medicare Advantage plans are not sold in ...
How to contact Medicare Advantage 2021?
New to Medicare? Compare Medicare plan costs in your area. Compare Plans. Or call. 1-800-557-6059. 1-800-557-6059 TTY Users: 711 to speak with a licensed insurance agent.
How often does Medicare cover colorectal cancer screening?
Medicare covers this screening test for colorectal cancer, in certain cases, once every 3 years. See
When will Medicare open enrollment start?
If you have ESRD, you can join a Medicare Advantage Plan during Open Enrollment (October 15–December 7, 2020). Your plan coverage will start January 1, 2021. See page 59.
Does Medicare pay for mental health?
If you have a behavioral health condition (like depression, anxiety, or another mental health condition), Medicare may pay your provider to help manage that condition if they offer the Psychiatric Collaborative Care Model. This model is a set of integrated behavioral health services, including care management support that may include:
Does Medicare cover preventive care?
Medicare covers many preventive services at no cost to you. Ask your doctor or other health care provider which preventive services (like screenings, shots or vaccines, and yearly “Wellness” visits) you need. See pages 30–51 and look for to learn more about which preventive services Medicare covers.
Does Medicare cover cognitive impairment?
Medicare covers a cognitive assessment to help detect the earliest signs of cognitive impairment. Your doctor may perform this assessment during a routine visit. If you show signs of cognitive impairment, Medicare also covers a separate visit with your regular doctor or specialist to do a full review of your cognitive function, establish or confirm a diagnosis like dementia, including Alzheimer’s disease, and develop a care plan. See
