
What is the true Medicare fraud rate?
The Medicare fraud rate shows that the program has the highest improper payment rate among its peers, at nearly 15%. In cash, this amounts to $57.36 billion. Medicare FFS has an improper payment rate of 7.25% ($28.91 billion), Medicare Part B of 7.87% ($16.73 billion), and CHIP of 15.83% ($2.74 billion).
What is the cost of health care fraud?
Although no precise measure of health care fraud exists, those who exploit Federal health care programs can cost taxpayers billions of dollars while putting beneficiaries’ health and welfare at risk. The impact of these losses and risks magnifies as Medicare continues to serve a growing number
What are some examples of healthcare fraud and abuse with Medicare?
The authorities discovered yet another instance of healthcare fraud and abuse with Medicare. Namely, Centers for Medicare and Medicaid Services paid over $160 million on medications for Medicare Advantage. The issue here is that hospices already cover those drugs. 12. In 2018, America spent $3.6 trillion on medical care.
What are some statistics about insurance fraud?
48 states make insurance fraud a specific crime. 8,500 cars were intentionally set on fire in 2018. 12.4% – 20.5% of construction workers were misclassified in 2018. $3.1 billion in false and fraudulent claims in 2020. 21% of insurance plan to invest in AI in the next two years. Most consumers are concerned about insurance fraud.
How much does Medicare fraud cost the US?
Medicare Fraud Costs $65 Billion a Year. You Can Help.
What percent of healthcare expenditures is fraud and abuse?
The National Heath Care Anti-Fraud Association estimates conservatively that health care fraud costs the nation about $68 billion annually — about 3 percent of the nation's $2.26 trillion in health care spending. Other estimates range as high as 10 percent of annual health care expenditure, or $230 billion.
How is Medicare fraud committed?
Beneficiaries commit fraud when they… Let someone use their Medicare card to get medical care, supplies or equipment. Sell their Medicare number to someone who bills Medicare for services not received. Provide their Medicare number in exchange for money or a free gift.
How common is healthcare fraud in the United States?
(July 2021) In fiscal year 2020, there were 330 health care fraud offenders, who accounted for 7.7% of all theft, property destruction, and fraud offenses. The number of health care fraud offenders decreased by 36.2% since fiscal year 2016. The USSC HelpLine assists practitioners in applying the guidelines.
Which is the most common form of health care fraud and abuse?
Fraudulent provider billing, duplicate billing, and billing for services not medically needed accounted for 46 percent of provider fraud cases in 2016. Billing for services not performed is the most common provider fraud activity and defrauds millions from public and commercial insurers alike.
What is the largest area of fraud identified by the insurance industry?
What is the largest area of fraud identified by the insurance industry? A: Medicare fraud is the most costly type of insurance fraud in the US. In 2017, it cost taxpayers $60 billion.
What is a major part of Medicare fraud?
Misusing codes on a claim, such as upcoding or unbundling codes. Upcoding is when a provider assigns an inaccurate billing code to a medical procedure or treatment to increase reimbursement. Medicare abuse can also expose providers to criminal and civil liability.
Why is Medicare fraud an issue?
There are health care consequences due to Medicare fraud. A beneficiary may later receive improper medical treatment from legitimate providers because of inaccurate medical records that may contain false diagnoses or incorrect lab results.
Who commits healthcare fraud?
Health care fraud can be committed by medical providers, patients, and others who intentionally deceive the health care system to receive unlawful benefits or payments. The FBI is the primary agency for investigating health care fraud, for both federal and private insurance programs.
How serious is insurance fraud?
Very serious. Insurance fraud is considered a felony, usually punishable by a large fine, and, in some instances, can lead to imprisonment. It's re...
What is the largest area of fraud identified by the insurance industry?
Medicare fraud is the most costly type of insurance fraud in the US. In 2017, it cost taxpayers $60 billion. Out of every $10 budgeted for the Medi...
How is insurance fraud detected?
It is a two-step process that starts with identifying suspicious claims either by using statistical analysis or based on tips from public and insur...
What happens if someone commits insurance fraud?
It depends on the severity of the fraud. For example, if it’s just an exaggerated but otherwise legitimate claim, the insurer will negotiate with t...
What happens if you get in trouble for insurance fraud?
Insurance fraud statistics inform us that insurance fraud is considered a felony punishable by fines, probation, or prison time in 48 states. The e...
How much money is wasted on Medicare fraud?
Medicare fraud statistics show that billions of dollars are wasted every year due to scams and corruption. The damage to the entire healthcare system is irreparable, as that money could have been invested in a range of legal medical services. Enormous expenses of fraudulent practices result in Medicare costs escalation.
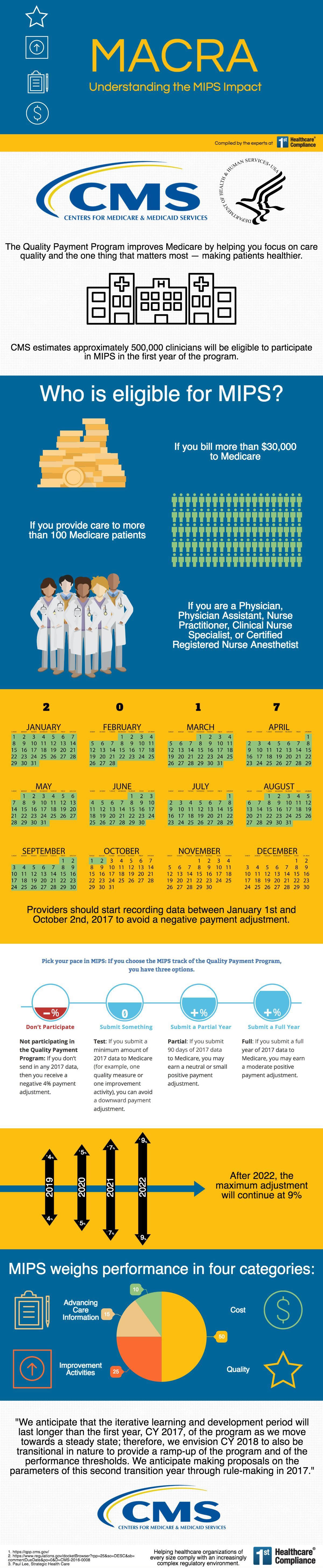
What is Medicare fraud?
Medicare fraud includes intentionally covering up the truth with the aim of obtaining illegitimate benefits. Paired with abuse, which involves practices that don’t adhere to authorized fiscal and medical practices to increase expenses, healthcare scams severely harm both the state and the federal medical system.
How much did Medicare spend on hospice?
Medicare spent $160.8 million on medications covered by hospices. (Source: Health Payer Intelligence) The authorities discovered yet another instance of healthcare fraud and abuse with Medicare. Namely, Centers for Medicare and Medicaid Services paid over $160 million on medications for Medicare Advantage.
How much money did the HHS return to Medicare?
Medical fraud statistics reveal that the Office of Inspector General at HHS and the US Department of Justice managed to return nearly $1.4 billion to Medicare Trust funds via fines, forfeits, and recoveries. These departments actively fight healthcare and insurance frauds and prosecute perpetrators.
How many Medicare claims were filed correctly?
Research showed that out of 300 sample claims, only 116 were filed correctly. Such an error cost the insurer almost $367 million.
What is the improper payment rate for medicaid?
Medicaid has an improper payment rate of 14.90%. Inconsistencies in payments may not necessarily mean fraud or abuse, but do indicate a human error. The Medicare fraud rate shows that the program has the highest improper payment rate among its peers, at nearly 15%. In cash, this amounts to $57.36 billion.
How much of the US population has Medicare?
18.1% of US residents have Medicare. Fraud, abuse, and waste account for up to 10% of overall healthcare expenditures. Medicare invests roughly $700 billion in its services. Medicare lost $2 billion to a single fraud. The US healthcare expenditures are estimated to reach 6.2 trillion by 2028.
What is the Medicare fraud rate?
His office pointed us to various documents that analyzed the problem of improper payments, an issue that mixes fraud together with nominally legal activities such as referring patients for more tests than are necessary. This suggested Roskam was using an inflated estimate of fraud. However, a recent study tends, in the worst-case analysis, to support Roskam’s figures.
Does the JAMA article stop at Medicare?
The JAMA article doesn’t stop at Medicare and Medicaid. It also looks at fraud in the health care sector as a whole, both public and private. The fraud rates don’t change much when the private sector is included.
What is the number to call for Medicare fraud?
1-800-557-6059 | TTY 711, 24/7. The above scenario is just one example of a recent type of Medicare scam. Let’s take a deeper look at Medicare fraud, including the types of scams to be aware of and how you and your loved ones can stay safe.
Why is it important to identify Medicare fraud?
Identifying Medicare fraud and abuse helps to maintain the integrity of the program, keep costs down and prosecute criminals. As a Medicare beneficiary, it is your duty to do your part in helping to combat Medicare fraud for the benefit of all. 1 Schulte, Fred.
What are some examples of Medicare abuse?
One example of Medicare abuse is when a doctor makes a mistake on a billing invoice and inadvertently asks for a non-deserved reimbursement. Medicare waste involves the overutilization of services that results in unnecessary costs to Medicare.
What is Medicare scam?
Medicare scams, like the one described above involving Medicare cards, are when individuals pose as health care providers to gather and use a Medicare beneficiary’s personal information to receive health care or money they are not entitled to.
How to protect yourself from Medicare fraud?
There are some additional things you can do and keep in mind to protect yourself from Medicare fraud: When you receive your new Medicare card in the mail, shred your old one. Also, be aware that Medicare will not contact you to verify information or to activate the card.
How long is the man in jail for Medicare fraud?
The man faces up to 10 years in prison for each of the six counts of fraud. A former health care executive in Texas admitted to her role in a $60 million Medicare fraud scheme that included overdosing hospice patients in order to maximize profits. She faces up to 10 years in prison.
What is the False Claims Act?
The False Claims Act protects the government from being sold substandard goods or services or from being overcharged. It holds people accountable who knowingly submit or cause to be submitted a false or fraudulent Medicare claim.
Health Insurance Fraud Statistics
Healthcare fraud in the US isn’t as uncommon as one may be led to believe. However, various corrective actions have been taken, and the rate of insurance fraud in the healthcare system has decreased.
Auto Insurance Fraud Statistics
Staged crashes, false or overblown reports, faking information… All these cause harm to insurers and can be extremely dangerous. The most extensive damage, $10 billion a year, is caused by unidentified drivers, people who used fake IDs or lied in other ways to get their cars insured.
Insurance Antifraud Statistics
In 48 states, insurance fraud is defined as a specific crime, while 30 states have insurer fraud defined as a specific insurance crime. Currently, eight US states don’t have dedicated insurance fraud bureaus.
The Bottom Line
It’s evident that insurance fraud hurts a lot of people, not just the “big evil corporations.” As we’ve seen from the statistics about fraud complaints and especially about car insurance fraud, the dangers of evading paying insurance premiums, or worse, staging accidents to collect insurance payouts aren’t just monetary.
What percentage of Americans are concerned about insurance fraud?
Most consumers are concerned about insurance fraud. Americans also show increasing tolerance for specific forms of unethical insurance behavior: 78% percent say they are concerned about insurance fraud. 88% say it’s unethical to misrepresent a claim to obtain payment for an uncovered loss, compared to 93% in 1997.
How many states have insurance fraud?
48 states make insurance fraud a specific crime. 30 states make insurer fraud a specific insurance crime. Oregon is the only state without an insurance fraud law of any kind. 42 states and the District of Columbia have an insurance fraud bureau. Most deal with all lines of insurance.
What is the federal False Claims Act?
The federal False Claims Act lets whistleblowers earn a portion of federal civil recoveries stemming from exposing fraud against federal healthcare programs. The FCA also can lead to criminal charges. Whistleblowers are often employees at offending healthcare organizations, with unique access to evidence.
How many medical records were breached in 2019?
Nearly 32 million patient medical records were breached in the first half of 2019. More than double the records breached over the entire 2018 calendar year. 2018 saw breaches of more than 15 million patient records. Incidents also rose in the first half of 2019, with 285 breaches reported between January and June.
How many states have laws making counterfeit airbags a specific crime?
Most deal with all lines of insurance. 43 states and the District of Columbia require insurers to report suspected fraud to the state fraud bureau or other agency. 22 states have enacted laws making counterfeit airbags a specific crime.
What is fraud plot?
Fraud plots are getting more complex, often involving multiple industries rather than solely insurance. An insurance investigation, for instance, might reveal evidence of financial fraud. 84 percent of insurance organizations say fraud cases they investigate involve more than one industry.
How much is Medicare improper payment?
Improper Medicare payments totaled $25.74 billion (6.27%) in FY 2020. That’s a drop from $28.91 (7.25%) in FY 2019. The decrease was driven by reductions of improper payment rates for home health and skilled nursing claims.
What is heat in Medicare?
The DOJ, OIG, and HHS established HEAT to build and strengthen existing programs combatting Medicare fraud while investing new resources and technology to prevent and detect fraud and abuse . HEAT expanded the DOJ-HHS Medicare Fraud Strike Force, which targets emerging or migrating fraud schemes, including fraud by criminals masquerading as health care providers or suppliers.
What is the role of third party payers in healthcare?
The U.S. health care system relies heavily on third-party payers to pay the majority of medical bills on behalf of patients . When the Federal Government covers items or services rendered to Medicare and Medicaid beneficiaries, the Federal fraud and abuse laws apply. Many similar State fraud and abuse laws apply to your provision of care under state-financed programs and to private-pay patients.
Is there a measure of fraud in health care?
Although no precise measure of health care fraud exists, those who exploit Federal health care programs can cost taxpayers billions of dollars while putting beneficiaries’ health and welfare at risk. The impact of these losses and risks magnifies as Medicare continues to serve a growing number of beneficiaries.
Is CPT copyrighted?
CPT codes, descriptions and other data only are copyright 2020 American Medical Association. All Rights Reserved. Applicable FARS/HHSAR apply. CPT is a registered trademark of the American Medical Association. Applicable FARS/HHSAR Restrictions Apply to Government Use. Fee schedules, relative value units, conversion factors and/or related components are not assigned by the AMA, are not part of CPT, and the AMA is not recommending their use. The AMA does not directly or indirectly practice medicine or dispense medical services. The AMA assumes no liability of data contained or not contained herein.
Can you give free samples to a physician?
Many drug and biologic companies provide free product samples to physicians. It is legal to give these samples to your patients free of charge, but it is illegal to sell the samples. The Federal Government has prosecuted physicians for billing Medicare for free samples. If you choose to accept free samples, you need reliable systems in place to safely store the samples and ensure samples remain separate from your commercial stock.
How does Medicare fraud affect the healthcare industry?
In fact, it impacts the entire healthcare industry. From wasting funds that could be going towards more medical staff to treat patients to people being denied life-saving procedures , this type of fraud is incredibly dangerous, and one that adds up to millions annually.
How much did Medicare fraud cost in 2018?
In 2018, government and law enforcement agencies participated in one of the largest fraud take downs in healthcare. The fraudulent schemes led to over $2 billion in Medicare and Medicaid losses. Over 600 defendants were charged.
What are the consequences of fraud?
Healthcare professionals also suffer. Not only does fraud make patients highly suspicious of any medications, treatments or procedures, but it can also lead to people not seeking treatment when they need it.
Why are overworked healthcare workers not able to provide optimal care?
One final consequence is less coverage. In an effort to combat Medicare fraud, claims and necessary treatments may be denied.
