Just the essentials...
- The QMB or Qualified Medicare Beneficiary Program is a Medicare Savings Program.
- Medicaid has four savings programs for eligible persons to save on Medicare costs
- The Qualified Medicare Beneficiary Program can cover premiums, deductibles, copays, and coinsurance
- Medicaid determines Medicare Savings Programs participation by income and need
How do you qualify for Medicare QMB?
You may be eligible if:
- You receive Medicare Part A,
- Your income must not be more than $1073/month for one person or $1,452/month for a couple (These amounts change every April), and
- Your assets do not exceed $7,970 for yourself or $11,960 if you have one or more dependents living with you.
How do you qualify for QMB program?
You may be eligible if:
- You receive Medicare Part A,
- Your income must not be more than $867/month for one person or $1,167/month for a couple (These amounts change every April), and
- Your assets do not exceed $4,000 for yourself or $6,000 if you have one or more dependents living with you.
What is the income limit for QMB?
Someone can enroll in a QMB program providing they meet the monthly income limits. For an individual, the limit is $1,084 per month. For a married couple, the combined income must be less than $1,457 per month. The income limits are slightly higher in Alaska and Hawaii.
What does QMB only mean for Medicaid eligibility?
What Does Medicaid QMB Cover? Medicaid QMB, which stands for Qualified Medicare Beneficiary, is a program designed specifically for individuals that qualify for both Medicare and Medicaid coverage and that are financially unstable.
What does QMB mean on Medicare?
Qualified Medicare BeneficiaryIf you're among the 7.5 million people in the Qualified Medicare Beneficiary (QMB) Program, Medicare providers aren't allowed to bill you for services and items Medicare covers, including deductibles, coinsurance, and copayments. If a provider asks you to pay, that's against the law.
How do you qualify to get $144 back from Medicare?
How do I qualify for the giveback?Are enrolled in Part A and Part B.Do not rely on government or other assistance for your Part B premium.Live in the zip code service area of a plan that offers this program.Enroll in an MA plan that provides a giveback benefit.
Why did I get an extra payment from Social Security this month?
The extra payment compensates those Social Security beneficiaries who were affected by the error for any shortfall they experienced between January 2000 and July 2001, when the payments will be made. Who was affected by the mistake? The mistake affected people who were eligible for Social Security before January 2000.
Can I get Medicare Part B for free?
While Medicare Part A – which covers hospital care – is free for most enrollees, Part B – which covers doctor visits, diagnostics, and preventive care – charges participants a premium. Those premiums are a burden for many seniors, but here's how you can pay less for them.
What is QMB in Medicare?
Qualified Medicare Beneficiary (QMB) Program. If you’re a Medicare beneficiary, you know that health care costs can quickly add up. These costs are especially noticeable when you’re on a fixed income. If your monthly income and total assets are under the limit, you might be eligible for a Qualified Medicare Beneficiary program, or QMB.
What is a qualified Medicare beneficiary?
The Qualified Medicare Beneficiary program is a type of Medicare Savings Program (MSP). The QMB program allows beneficiaries to receive financial help from their state of residence with the costs of Medicare premiums and more. A Qualified Medicare Beneficiary gets government help to cover health care costs like deductibles, premiums, and copays.
What is a QMB premium?
The Part A monthly premium (if applicable) The Part B monthly premium and annual deductible. Coinsurance and deductibles for health care services through Parts A and B. If you’re in a QMB program, you’re also automatically eligible for the Extra Help program, which helps pay for prescription drugs.
What is Medicare qualified?
A Qualified Medicare Beneficiary gets government help to cover health care costs like deductibles, premiums, and copays. Recipients must meet all criteria to qualify for the program assistance.
What is the QMB in North Carolina?
In North Carolina QMB is called MQB. If you live in Nebraska, Federal QMB is replaced with full Medicaid.
Why do you need a QMB with Advantage?
Pairing an Advantage Special Needs Plan with your QMB is a great way to protect yourself from unexpected health costs. It also provides extra benefits at an affordable price.
How to enroll in QMB?
The first step in enrollment for the QMB program is to find out if you’re eligible. A quick and easy way to do this is to call your local Medicaid office. The next step is to complete an application. You can request Medicaid to provide you with an application form or locate a QMB program application from your state online.
What is QMB in Medicare?
The QMB program is a state program that helps covers the cost of Medicare premiums, deductibles and coinsurance that Medicare beneficiaries usually pay. You may be eligible for the QMB program if you are entitled to Medicare Part A coverage, and have limited income and resources. If you are eligible, your state’s Medicaid program may pay for your Medicare Part B premium, Part A and Part B deductibles, and coinsurance.
What is QMB insurance?
The QMB program covers the cost of Medicare premiums, deductibles and coinsurance that Medicare beneficiaries usually pay. It means that your state covers these Medicare costs for you, and you have to pay only for anything that Medicare normally does not cover.
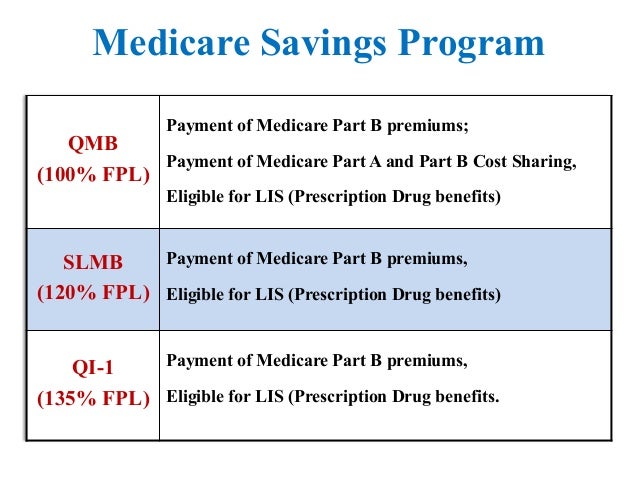
What is a SLMB?
The Specified Low-Income Medicare Beneficiary Program. If your income is too high to qualify for QMB but is not more than 20 percent above the federal income poverty level, you may receive Specified Low-Income Medicare Beneficiary (SLMB) coverage, which pays for your Medicare Part B monthly premium only. You will, however, pay for Medicare ...
What if my income is too high for SLMB?
If your income is too high for help under SLMB, you may qualify under the Qualifying Individual (QI) program. If your income is more than 20 percent but no more than 35 percent above the national poverty level, your state may pay your Medicare Part B premium .
How to contact Medicare.org?
Call us at (888) 815-3313 — TTY 711 to speak with a licensed sales agent.
Why do I have to apply for QI each year?
The QI program must be applied for each year because assistance is provided from a limited pool of funds on a first-come, first-served basis. Individuals who received the benefit in the last month of the previous year will be given priority.
Does QMB supplement Medicare?
QMB does not supplement your Medicare coverage but instead ensures that you will not be precluded from coverage because you cannot afford to pay the costs associated with Medicare. Keep in mind that some states require you to pay a small co-payment when you see a doctor.
How much does QMB pay for Medicare?
It can pay deductibles that can total more than $1,400 per year for Part A and more than $190 for Part B. The QMB can also pay copays that apply to services used by participants. The overall amount of these payments depends on upon the services used.
What is QMB program?
The QMB Program is the Qualified Medicare Beneficiary program; Medicaid pays premiums for Part A and for Part B. It pays deductibles, coinsurance, and copays for Part B. The program accepts applicants with incomes as high as 100 percent of the federal poverty guideline. The QDWI Program is the qualified disabled and working individuals program;
What does QMB cover?
The QMB covers costs associated with Original Medicare and Part D Prescription Drugs. The QMB can pay Medicare Part A premiums. For those that purchase Medicare Part A, this is a substantial monthly expense.
What does qualified Medicare cover?
The Qualified Medicare Beneficiary Program can cover premiums, deductibles, copays, and coinsurance
What percentage of Medicare Part B is covered by QMB?
In Medicare Part B, there is a common relationship of 80 percent coverage by Medicare and 20 percent by the client. The QMB program can pay part of the prescription drug costs for participants in a Medicare Part D: Prescription Drugs plan.
What is the QMB limit for 2020?
The 2020 asset or allowed financial resource limit was $7,860 for an adult individual or $11,800 for a married couple. The states usually exclude the values of the below-listed items.
How much does the QI program pay?
The QI savings program pays Medicare Part B premiums that range from $144.60 per month and upwards depending on fines and income.
What does QMB mean for medicaid?
What Does Medicaid QMB Cover? Medicaid QMB, which stands for Qualified Medicare Beneficiary , is a program designed specifically for individuals that qualify for both Medicare and Medicaid coverage and that are financially unstable.
What is qualified Medicare Beneficiary?
The Qualified Medicare Beneficiary program works to help cover Medicare Part A and Part B premiums, as well as the costs of coinsurance, copayments, and deductibles. All of these costs can add up quickly, especially if you require a variety of different medical services. This program is able to provide full payment of both ...
What is the difference between Medicare and Medicaid?
Original Medicare is available to individuals 65 years of age or older and individuals with certain disabilities. Medicaid insurance caters to individuals with low income and provides an affordable, government-funded healthcare option for this demographic. The QMB program has specific income requirements that must be met, ...
How many people were in the QMB in 2016?
The amounts of the QMB requirements and the poverty line generally coincide, but it is good to be aware of both. In 2016, there were approximately 7.5 million individuals that are a part of the QMB program. In fact, nearly one out of every eight Medicare recipients was a member of this program.
What is the income limit for QMB?
In 2019, the monthly income limits for individuals is $1,060 and the monthly income limit for a married couple is $1,430. There is also a limit on resources, which is set at $7,730 for individuals and $11,600 for married couples. Additionally, you must also be at or below the annual federal poverty level. The amounts of the QMB requirements and the poverty line generally coincide, but it is good to be aware of both.
Is Medigap covered by QMB?
It is important to note that if you are currently using a Medigap plan, the premiums associated with it are not covered by the QMB program. In addition, you should also be aware that states can impose laws specific to Medicaid, Medicare, and QMB programs.
Can you be billed for Medicare Part A and Part B?
This means that you should not be billed for any approved care you receive under Medicare Part A or Part B that is received at a Medicare-approved facility by an approved provider. There should be no major exceptions to this other than the restrictions on care that Original Medicare puts in place.
What are the benefits of QMB?
Benefits of the QMB program include: 1 Medicare Part A & B premiums paid back in your Social Security Check 2 Medicare Part D premium reduced or covered through the Low Income Subsidy (LIS) / Extra Help program 3 Medication costs reduced to $0 – $10 for most medications through the LIS / Extra Help program 4 No Donut Hole / Coverage Gap 5 Medicare deductibles paid by Medicaid 6 Medicare coinsurance and copays within prescribed limits paid
Where can I find the SSI limits?
The limits are updated quarterly and can be found on the SSI-Related Programs Financial Eligibility Standards Chart.
Does Medicare pay for hospital visits?
No copays for doctors, hospital visits, or medical procedures for Medicare approved expenses.
Can a trust pay a beneficiary?
With either example, AGED as the Trustee may use the money in the trust to pay bills and expenses for the individual (known as the beneficiary), as long as the expenses are for the sole benefit of the beneficiary, and are not paid for by government benefits. Examples of bills paid from the trust include, but are not limited to, mortgage, rent, facility bills, utilities, repairs, auto insurance, auto payment, etc. However, the trust cannot pay the beneficiary directly, as this could disqualify them from the QMB program.
Does Medicaid count overage?
Setting up a Pooled Trust allows you to place your over income and/or over asset (or both) into the trust, making this overage no longer “countable” for Medicaid purposes. This means that while Medicaid acknowledges your total income and/or assets, they deduct the income and/or assets placed into the trust from the total, so that it no longer counts against you.
What does QMB mean in Medicare?
QMB stands for “Qualified Medicare Beneficiary” and is a cost assistance program designed to help individuals who are eligible for both Medicare and Medicaid, a circumstance that is known as “dual eligibility.”
What is QMB insurance?
The QMB program helps pay for the full cost of Medicare Part A and Part B premiums along with complete coverage of deductibles, copayments and coinsurance. QMB offers the most comprehensive coverage of the programs available to dual-eligible beneficiaries.
What is a dual eligible special needs plan?
This is a particular type of Medicare Advantage plan with a benefits package that is tailored to the needs of those with the limited income and resources common among Medicaid recipients.
How to apply for QMB?
To apply for the QMB program, contact your state Medicaid program . Please not that if your income or financial resources are close to the totals listed above, you should still apply, as you may potentially be eligible.
Can a QMB provider charge other Medicare beneficiaries?
Federal law prohibits providers from billing beneficiaries enrolled in the QMB program for any such costs. This law even pertains to non-participating providers, who are allowed to charge other Medicare beneficiaries more for care.
Do you have to be on Medicare to qualify for QMB?
You must be eligible for both Medicare and Medicaid to be eligible for QMB benefits. While Medicare’s eligibility requirements are federally mandated, each state may set its own qualifying restrictions for Medicaid.
Does QMB cover Medicaid?
The QMB improper billing protection even extends to health care providers who do not accept Medicaid. That means QMB members may receive care from a provider who does not accept Medicaid and still receive protection from deductibles, copayments and coinsurance.
What is QMB in Medicare?
QMB is one is of four Medicare Savings Programs designed to assist those with limited financial resources to more easily access Medicare coverage. These programs are federally funded and administered through state-run Medicaid agencies.
What is QMB program?
Beneficiaries who qualify for the QMB program automatically receive assistance with the costs of their prescription drugs through Extra Help. Also known as the Part D Low Income Subsidy, this program limits the costs you pay out of pocket to a few dollars per prescription.
How does QMB work?
The QMB program makes Medicare more accessible by paying for premiums, deductibles and cost-sharing of Medicare-covered expenses. About 7.7 million people, or 12.5% of people with Medicare coverage, receive assistance through the QMB program.
How to apply for qualified medicaid?
To apply for the Qualified Medicare Beneficiary program, contact your state Medicaid agency. Medicare encourages you to fill out an application if you think you might be eligible, even if your resources exceed the limits posted on their website.
What happens if you are charged for QMB?
If you're charged, advise the provider that you're enrolled in the QMB program. If you've made a payment while enrolled in the program, you're entitled to a refund.
Can a qualified Medicare beneficiary bill you?
Under the Qualified Medicare Beneficiary Program, health care providers are not permitted to bill you for Medicare services. QMB pays for:
Do you have to pay deductibles on QMB?
Once you're enrolled in the QMB program, you're no longer legally obligated to pay for deductibles, coinsurance or co-payments for any services or items covered by Medicare Part A or B.
What is QMB program?
Since the QMB program aims to help individuals with low income, it places limits on the monthly income and financial resources available to you. If you exceed these limits, you may not be eligible for the program. Generally, participation is limited to individuals who meet the federal poverty level.
How to apply for QMB?
To apply for the QMB program, you’ll need to contact your state Medicaid office. You can check online to find your state’s office locations, or call Medicare at 800-MEDICARE. The documentation you’ll need varies by state, but your application process will likely include submissions of identification, proof of Medicare coverage, and financial information.
How to enroll in QMB?
To enroll in the QMB program, you first need to be enrolled in Medicare Part A. The next step is to review your income and assets to see if you fall below the limits set by Medicare. But remember there are exceptions to those limits, and you’re encouraged to apply even if your income or assets exceed them.
How long does it take to get a QMB denial?
Once you submit your application, you should receive a confirmation or denial within about 45 days. If you’re denied, you can request an appeal. Enrollment in any of the MSPs must be renewed each year. Even when your QMB is active, you may at times be wrongfully billed for items or services that it covers.
What is Medicare for older adults?
Medicare is meant to provide affordable healthcare coverage for older adults and other individuals in need. Even so, out-of-pocket costs can add up.
Can you be wrongfully billed for QMB?
Even when your QMB is active, you may at times be wrongfully billed for items or services that it covers. Contact Medicare for any billing problems. Be sure to carry documentation of your participation in the QMB program and show it to your providers.
Do you have to be a resident to qualify for QMB?
You must be a resident of the state in which you’re applying for the QMB program, and you must already be enrolled in Medicare Part A. Assets that aren’t counted when you apply for the QMB program include: your primary home.