Key Findings Race and ethnicity, dual eligibility, and potentially disabling condition status were associated with Medicare fee-for-services beneficiaries’ 30-day readmissions. The readmission rate by race and ethnicity ranged from 13.8% among non-Hispanic White beneficiaries to 19.4% among non- Hispanic Black beneficiaries.
Why are hospital readmissions bad?
4 rows · Jul 16, 2019 · For AMI, the 30-day readmission rate was 0.2 percentage point (CI, −0.2 to 0.6 percentage point) ...
How to use telehealth to reduce readmission rates?
However, among index admissions appearing in HEDIS, 14.4% for AMI, 18.4% for CHF, and 13.9% for pneumonia resulted in a readmission. Patients in Medicare Advantage had lower unadjusted readmission rates than those in traditional Medicare for all 3 conditions (16.6% vs. 17.1% for AMI, 21.4% vs. 21.7% for CHF, and 16.3% vs. 16.4% for pneumonia).
What is the new Medicare rate?
Jul 16, 2021 · The hazard ratio for 30-day readmission was 0.47 (95% confidence interval [CI] 0.33-0.68, P<0.0001). The hazard ratio for 1-year readmission was 1.45 (95% CI 1.19-1.76, P<0.001). Conclusions:This is one of the first studies of …
How do readmission rates affect revenue?
May 02, 2012 · Under Medicare's Inpatient Prospective Payment System (IPPS), as included in the Affordable Care Act (ACA), there will be adjustments to payments made for excessive readmissions in acute care hospitals during fiscal years beginning on or after October 1, 2012. A readmission is defined as: being admitted at the same or different hospital within ...

What is Medicare readmission rate?
How many Medicare beneficiaries are readmitted within 30 days every year?
What percentage of 30-day readmission rates for Medicare beneficiaries are unplanned?
What percentage of patients are readmitted?
What is the hospital readmissions reduction program?
What factors contribute to hospital readmissions among older adults?
How do you calculate readmission rate?
What is the Medicare 30-day readmission rule?
Does Medicare penalize hospitals for readmissions?
Why are readmission rates so high?
What diagnosis has the highest readmission rate?
What is 30-day readmission rate?
When did the Hospital Readmissions Reduction Program start?
The Hospital Readmissions Reduction Program (HRRP) was created by the 2010 Affordable Care Act and began in October 2012 as an effort to make hospitals pay more attention to patients after they leave. Readmissions occurred with regularity — for instance, nearly a quarter of Medicare heart failure patients ended up back in the hospital within 30 days in 2008 — and policymakers wanted to counteract the financial incentives hospitals had in getting more business from these boomerang visits.
How many hospitals are exempt from Medicare?
An additional 2,216 hospitals are exempt from the program because they specialize in children, psychiatric patients or veterans. Rehabilitation and long-term care hospitals are also excluded from the program, as are critical access hospitals, which are treated differently because they are the only inpatient facility in an area. Of the 3,046 hospitals for which Medicare evaluated readmission rates, 82% received some penalty, nearly the same share as were punished last year.
Is Medicare cutting Medicare payments?
The federal government’s effort to penalize hospitals for excessive patient readmissions is ending its first decade with Medicare cutting payments to nearly half the nation’s hospitals.
How to reduce avoidable readmissions?
Reducing avoidable readmissions requires that hospitals build partnerships with other providers and the community to address social risk factors and promote continuous care when a patient is discharged from the hospital. Partnerships with community service providers can facilitate the transition of patients back into the community and ensure continuity of care for patients following hospitalization. Many hospitals already have relationships within their communities through community benefit activities associated with non-profit status. Hospitals may leverage and build on their community benefits activities and programs to address social determinants that lead to readmissions by connecting patients to community programs. For example, a referral to a community-based organization may ensure that a patient has transportation access for a follow-up visit post-discharge. This can be supported through informal or formal agreements with primary care providers and practices that promote data-sharing and cooperation. These are essential to maintaining the continuity of care. They will ensure that the next care provider is aware of the patient’s status and care information. Community partners can direct at-risk patients to needed care following hospitalization. Community partners can also address other non-medical factors that could lead to readmissions such as issues related to social support, health literacy, and food and housing security. In addition, hospitals may benefit from developing or strengthening their relationship with public health officials. These partnerships can increase access to local level data to inform readmission reduction efforts. In places where these partnerships already exist, hospitals could focus on strengthening them.
How does communication improve patient care?
Effective clinician-patient communication is directly linked to improved patient satisfaction, adherence, and health outcomes. 55 Communication is essential to the care process and to preventing avoidable readmissions. However, providers often have limited time to develop a personal connection with patients and ensure appropriate patient-provider communication during the inpatient stay. The goal of effective communication is patients’ ability to understand three things: (1) their diagnosis and its implications for care, (2) care choices, including what requires attention, and (3) discharge instructions, including what signs and symptoms trigger a return visit, when to return for a routine follow-up, and how to take the prescribed medications.36 Low health literacy, mistrust, or language barriers can influence a patient’s understanding.36,56-59 Patients from minority racial and ethnic backgrounds, as well as patients with disabilities, are often dissatisfied in their experiences with communicating with their clinicians.60,61
Which census division had the highest rate of readmission?
Census division: The South Atlantic Census Division had the highest representation in the study sample (21.9%); the Mountain Division represented the smallest geographic subgroup (5.3%). Medicare beneficiaries residing in the New England Census Division had the highest rate of 30- day readmission (15.5%), and those from the Mountain Division had the lowest (12.3%).
What is readmissions disparity?
In addition, populations made vulnerable through public policies, social inequity, and social bias are known to be at heightened risk for hospital readmissions, and this increased likelihood is known as a readmissions disparity. Understanding the drivers of readmissions disparities can help to improve health outcomes for Medicare beneficiaries, particularly for those who are vulnerable, and in containing readmissions-related costs.
What are the objectives of the 30-day readmission study?
Study Objectives and Research Questions This study sought to analyze whether demographic, clinical, and geographic characteristics were associated with 30-day hospital inpatient readmissions in Medicare fee-for-service (FFS) beneficiaries; specifically, whether key demographic, clinical, and geographic groups known to be disproportionately impacted by social risk factors had higher rates of 30-day hospital inpatient readmission. This report details the relationships identified between readmissions and race and ethnicity, potentially disabling condition status, Medicare-Medicaid dual eligibility status, and rurality, stratified by level of index hospital quality rating, primary diagnoses at index
What is the purpose of the readmission analysis?
The overarching purpose of the analysis was to identify disparities in readmissions across levels of the above indicators of interest (e.g. race and ethnicity groups), stratified by (1) discharge settings (e.g. home/self-care, skilled nursing facility, home health care, inpatient rehabilitation facility), (2) levels of hospital quality, (3) a select set of high-frequency diagnoses, and (4) Census divisions. A more nuanced understanding of such associations supports the CMS Office of Minority Health’s goal to achieve health equity across all Medicare beneficiaries.
How long does it take for a hospital to readmission?
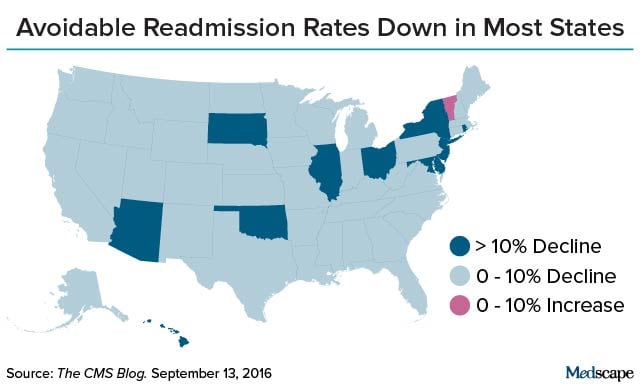
CMS defines hospital readmissions as inpatient stays that occur within 30 days of discharge from the index admission (i.e. initial inpatient hospitalization) (CMS, 2018). Hospital readmissions are considered a core health care quality indicator due to the fact that they can be the direct result of substandard care during index hospitalization, poor discharge planning, and/or poor coordination of post-acute care services (Feigenbaum et al., 2012). While overall readmission rates have decreased over time, data from 2006–2015 suggest that there are consistent racial and ethnic- and geographic-related disparities in hospital readmissions (Desai et al., 2016; Martsolf et al., 2016). Additional research concerning hospital readmissions suggests that factors such as hospital size and type affect readmissions (Gerhardt et al., 2013; Martsolf et al., 2016). Moreover, lower- quality hospitals tend to have higher rates of readmission than do higher-quality hospitals (Krumholz et al., 2017).
What is RQ3 in hospitalization?
RQ3: Setting of discharge from index hospitalization
What are the other post acute care settings?
Other post-acute care settings included discharges to court/law enforcement, federal hospitals, and other types of health care institutions not specified elsewhere.