How does Medicare determine reimbursement rates?
for these:
- Most doctor services (including most doctor services while you're a hospital inpatient)
- Outpatient therapy
- Durable Medical Equipment (Dme) Certain medical equipment, like a walker, wheelchair, or hospital bed, that's ordered by your doctor for use in the home.
How much does Medicare reimburse?
The amount for each procedure or test that is not contracted with Medicare can be up to 15 percent higher than the Medicare approved amount. In addition, Medicare will only reimburse patients for 95 percent of the Medicare approved amount.
What is the Medicare reimbursement percentage?
Types of Medicare reimbursement
- Participating provider. Most providers fall under this category. ...
- Opt-out provider. These providers do not accept Medicare and have signed a contract to be excluded. ...
- Nonparticipating provider. If the provider is not a participating provider, that means they don’t accept assignment. ...
- Special circumstances. ...
What is the Medicare allowable rate?
The rate at which Medicare reimburses health care providers is generally less than the amount billed or the amount that a private insurance company might pay. According to the Centers for Medicare & Medicaid Services (CMS), Medicare’s reimbursement rate on average is roughly 80 percent of the total bill. 1
How much does Medicare pay for medical services?
The Medicare reimbursement rates for traditional medical procedures and services are mostly established at 80 percent of the cost for services provided. Some medical providers are reimbursed at different rates. Clinical nurse specialists are paid 85 percent for most of their billed services and clinical social workers are paid 75 percent ...
Why use established rates for health care reimbursements?
Using established rates for health care reimbursements enables the Medicare insurance program to plan and project for their annual budget. The intent is to inform health care providers what payments they will receive for their Medicare patients.
How many specialists are on the Medicare committee?
Medicare establishes the reimbursement rates based on recommendations from a select committee of 52 specialists. The committee is composed of 29 medical professionals and 23 others nominated by professional societies.
What is the original objective of Medicare?
The original objective was to establish a uniform payment system to minimize disparities between varying usual, customary, and reasonable costs. Today, Medicare enrollees who use the services of participating health care professionals will be responsible for the portion of a billing claim not paid by Medicare.
How much can Medicare increase from current budget?
By Federal statute, the Medicare annual budget request cannot increase more than $20 million from the current budget.
Who needs to be a participant in Medicare?
To receive reimbursement payments at the current rates established by Medicare, health care professionals and service companies need to be participants in the Medicare program.
Does Medicare accept all recommendations?
While Medicare is not obligated to accept all of the recommendations, it has routinely approved more than 90 percent of the recommendations. The process is composed of a number of variables and has been known for lack of transparency by the medical community that must comply with the rates.
What is Medicare reimbursement rate?
A Medicare reimbursement rate is the amount of money that Medicare pays doctors and other health care providers for the services and items they administer to Medicare beneficiaries. CPT codes are the numeric codes used to identify different medical services, procedures and items for billing purposes. When a health care provider bills Medicare ...
How much more can a health care provider charge than the Medicare approved amount?
Certain health care providers maintain a contract agreement with Medicare that allows them to charge up to 15% more than the Medicare-approved amount in what is called an “excess charge.”.
What is the difference between CPT and HCPCS?
The CPT codes used to bill for medical services and items are part of a larger coding system called the Healthcare Common Procedure Coding System (HCPCS). CPT codes consist of 5 numeric digits, while HCPCS codes ...
How much does Medicare pay for coinsurance?
In fact, Medicare’s reimbursement rate is generally around only 80% of the total bill as the beneficiary is typically responsible for paying the remaining 20% as coinsurance. Medicare predetermines what it will pay health care providers for each service or item. This cost is sometimes called the allowed amount but is more commonly referred ...
Is it a good idea to check your Medicare bill?
It’s a good idea for Medicare beneficiaries to review their medical bills in detail. Medicare fraud is not uncommon, and a quick check of your HCPCS codes can verify whether or not you were correctly billed for the care you received.
How does Medicaid work?
Many states deliver Medicaid through managed care organizations, which manage the delivery and financing of healthcare in a way that controls the cost and quality of services. More states are joining this trend because they think it may help manage and improve healthcare costs and quality.
What is FQHC in Medicare?
The FQHC rate is a benefit under Medicare that covers Medicaid and Medicare patients as an all-inclusive, per-visit payment, based on encounters. Tribal organizations must apply before they can bill as FQHCs. Allowable expenses vary by state. Each tribe and state must negotiate the exact reimbursement rate.
What is capitated rate?
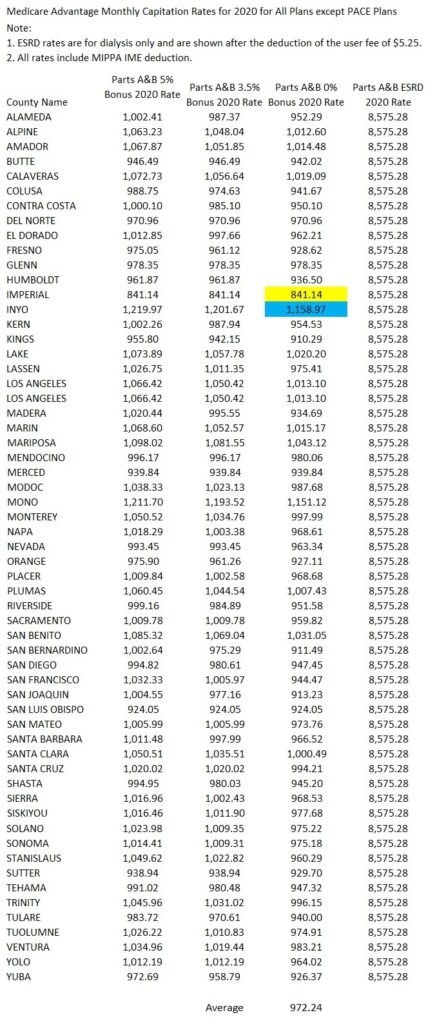
A capitated rate is a contracted rate based on the total number of eligible people in a service area. Funding is supplied in advance, creating a pool of funds from which to provide services. This rate can be more beneficial for providers with a larger client base because unused funds can be kept for future use.
Does LTSS qualify for reimbursement?
LTSS delivered through a CA H facility may qualify for different reimbursement rates. Reimbursement is on a per-cost basis instead of the standard Medicare reimbursement rates. Learn more about critical access hospitals.
Can tribes negotiate with states for Medicaid?
Tribes can negotiate with their states for an enhanced or higher reimbursement rate for Medicaid-covered services based on a 100% Federal Medical Assistance Percentage or any other known factors about a particular state that may affect the negotiation. Learn more about Medicaid financing and reimbursement.
Does each state reimburse for each encounter?
For example, some states reimburse for each service provided during an encounter (a face-to-face interaction between the patient and the healthcare provider), rather than setting a flat fee for each encounter.
Is IHS bill per encounter?
Billing is per encounter, not per specific service. The IHS rate is mandated by the Department of Health and Human Services and is published yearly in the Federal Register. See the 2021 rate information. Allowable services vary by state.
What happens when someone receives Medicare benefits?
When someone who receives Medicare benefits visits a physician’s office, they provide their Medicare information , and instead of making a payment, the bill gets sent to Medicare for reimbursement.
Why do doctors accept Medicare?
The reason so many doctors accept Medicare patients, even with the lower reimbursement rate, is that they are able to expand their patient base and serve more people.
Do you have to pay Medicare bill after an appointment?
For some patients, this means paying the full amount of the bill when checking out after an appointment, but for others , it may mean providing private insurance information and making a co-insurance or co-payment amount for the services provided. For Medicare recipients, however, the system may work a little bit differently.
Can a patient receive treatment for things not covered by Medicare?
A patient may be able to receive treatment for things not covered in these guidelines by petitioning for a waiver. This process allows Medicare to individually review a recipient’s case to determine whether an oversight has occurred or whether special circumstances allow for an exception in coverage limits.
When will Medicare reimbursement be released for 2021?
Find out what this means for you. Published March 16, 2020.
Does Medicare charge out of pocket for a CDC test?
And the CDC announced that it will not be charging any out-of-pocket costs to uninsured persons for the test. You can learn more about Medicare Advantage plans and the benefits they offer by calling to speak with a licensed insurance agent.
What factors affect insurance reimbursement rate for psychotherapy?
Factors that effect your insurance reimbursement rate for psychotherapy: Location, paying more for under-served locales and less for over-served locations. License, education, and specialization. Specialization. Consumer demand at the time of signing your contract.
What is contracted rate?
Your contracted rate for a specific insurance plan or network is set when you sign your initial contract. Insurance companies tend not to change, nor adjust, your rates for inflation if you do not personally request a raise or update of your fee schedule.
Does insurance pay for mental health therapists?
In summary, some private insurance companies reimburse mental health therapists for far more than others. A great way to quickly learn which companies pay the most is to simply ask your colleagues about their experiences with different reimbursement rates for private insurance companies.
Do insurance companies release contracted rate information?
Insurance companies are completely unwilling to release their contracted rate information for reason we’ll discuss shortly and as a result, you don’t know how much you’ll be reimbursed for providing psychotherapy and other mental health services.
Does Medicare cover mental health?
Medicare doesn’t cover all licenses and is far more selective than Medicaid about which providers they will allow into their network. As a result, mental health reimbursement rates for Medicare are higher than Medicaid rates by a substantial margin.