3rd – 5th Level of Appeals
| Level of Appeal | Time Limit for Filing Request | Time Limit for Filing Request |
| Third Level of Appeal: Administrative La ... | 60 days from the date of receipt of the ... | Current Amount in Controversy (AIC) requ ... |
| Fourth Level of Appeal: Department Appea ... | 60 days from the date of receipt of the ... | None |
| Fifth Level of Appeal: Federal Court Rev ... | 60 days from date of receipt of the Appe ... | Current AIC requirement can be found on ... |
Where to get help in making a Medicare appeal?
an appeal no matter how you get your Medicare. For more information, visit Medicare.gov/appeals, or call 1-800-MEDICARE (1-800-633-4227). TTY users can call 1-877-486-2048. Can someone file an appeal for me? If you want help filing an appeal, you can appoint a representative. Your representative can help you with the appeals steps explained
Who can assist with a Medicare appeal?
You can get help filing your appeal from your doctor, family members, attorneys, or advocates. As a Medicare beneficiary, you have certain rights. One of them is the right to appeal a Medicare decision that you think is unfair or will jeopardize your health. The Medicare appeals process has several levels.
When can I file an appeal to a Medicare claim?
You must file this appeal within 180 days of getting the denial of your first appeal. Medicare Advantage. With Medicare Advantage plans, you're dealing not only with Medicare, but with the rules set by the private insurance company that runs your program.
How to appeal a higher Medicare Part B premium?
There are 7 qualifying life-changing events:
- Death of spouse
- Marriage
- Divorce or annulment
- Work reduction
- Work stoppage
- Loss of income from income producing property
- Loss or reduction of certain kinds of pension income
What happens if OMHA does not issue a decision?
When can an ALJ request a reconsideration?
How long does it take for an OMHA to issue a remand order?
About this website

What are the five levels of the Medicare appeals process?
The Social Security Act (the Act) establishes five levels to the Medicare appeals process: redetermination, reconsideration, Administrative Law Judge hearing, Medicare Appeals Council review, and judicial review in U.S. District Court. At the first level of the appeal process, the MAC processes the redetermination.
How many levels of Medicare appeals are there?
5 levelsThe appeals process has 5 levels. If you disagree with the decision made at any level of the process, you can generally go to the next level. At each level, you'll get instructions in the decision letter on how to move to the next level of appeal.
What is the last level of appeal for Medicare claims?
The levels are: First Level of Appeal: Redetermination by a Medicare Administrative Contractor (MAC) Second Level of Appeal: Reconsideration by a Qualified Independent Contractor (QIC) Third Level of Appeal: Decision by the Office of Medicare Hearings and Appeals (OMHA)
What is a Level 2 appeal?
Second Level of Appeal: Reconsideration by a Qualified Independent Contractor. Any party to the redetermination that is dissatisfied with the decision may request a reconsideration.
What is a Level 1 appeal?
The first level of an appeal for Original Medicare is called a redetermination. A redetermination is performed by the same contractor that processed your Medicare claim. However, the individual that performs the appeal is not the same individual that processed your claim.
What is a first level appeal?
Any party to the initial claim determination that is dissatisfied with the decision may request a redetermination.
When a Medicare claim is appealed the final fifth level of the appeal process is the quizlet?
Rationale: The fifth level of appeal is the Federal District Court. If the provider or the patient is not satisfied with the Council's decision, a request for a hearing before a federal district court can be requested within 60 days as long as the amount of the appeal meets or exceeds $1460 for 2015.
Can providers appeal denied Medicare claims?
If you disagree with a Medicare coverage or payment decision, you can appeal the decision. Your MSN contains information about your appeal rights. If you decide to appeal, ask your doctor, other health care provider, or supplier for any information that may help your case.
What percentage of Medicare appeals are successful?
For the contracts we reviewed for 2014-16, beneficiaries and providers filed about 607,000 appeals for which denials were fully overturned and 42,000 appeals for which denials were partially overturned at the first level of appeal. This represents a 75 percent success rate (see exhibit 2).
What is a Medicare appeal?
An appeal is the action you can take if you disagree with a coverage or payment decision by Medicare or your Medicare plan. For example, you can appeal if Medicare or your plan denies: A request for a health care service, supply, item, or drug you think Medicare should cover.
What is a lower level of care denial?
Lower level of care" is a denial that applies when the following occurs: • Care provided on an inpatient basis is typically provided on an outpatient basis. • Outpatient procedure could have been done in the provider's office. • Skilled nursing care could have been performed by a home health agency.
How do you win a Medicare appeal?
File a written request asking Medicare to reconsider its decision. You can do this by writing a letter or by filing a Redetermination Request form with the Medicare administrative contractor in your area. The address should be listed on your Medicare summary notice.
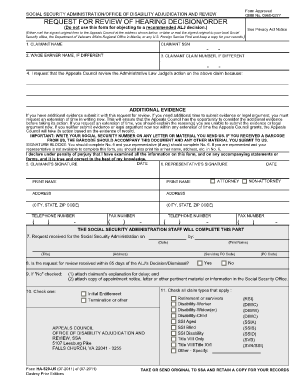
Requesting an ALJ Hearing | HHS.gov
What do I need to know to request a Medicare hearing with an Administrative Law Judge (ALJ)? You have the right to appeal any issue not decided entirely in your favor regarding your Medicare eligibility, enrollment, premium, or coverage of items or services under Part A & B, Part C, or Part D of the Medicare program.. You can request a hearing before an Administrative Law Judge (ALJ) if you ...
Appeals Level 3: Decision by the Office of Medicare Hearings and ...
You may request a decision by OMHA, based on a hearing before an Administrative Law Judge (ALJ) or, in certain circumstances, a review of the appeal record by an ALJ or attorney adjudicator.
Forms Needed for Your Level 3 Appeal | HHS.gov
Form Description; Request for Escalation to Medicare Appeals Council Form OMHA-384 Form OMHA-384 (Large Print) If your Medicare Part A or Part B appeal of a Qualified Independent Contractor (QIC) reconsideration is pending at OMHA and the adjudication period has elapsed, this form may be used to request escalation of your appeal to the Medicare Appeals Council. Escalation is not available for ...
5 things to know when filing an appeal | Medicare
If you decide to file an appeal, ask your doctor, health care provider, or supplier for any information that may help your case. If you think your health could be seriously harmed by waiting for a decision about a service, ask the plan for a fast decision.
MEDICARE RECONSIDERATION REQUEST FORM — 2nd LEVEL OF APPEAL
yes i have evidence to submit. department of health and human services centers for medicare & medicaid services . omb exempt . medicare reconsideration request form — 2nd level of appeal
Mailing addresses for Medicare Appeals - Novitas Solutions
State. PO Box number. 4 digit zip. Arkansas, Louisiana, Mississippi Part A . 3103. 1819. Colorado, New Mexico, Texas Part A. 3113. 1828. Indian Health Services Part A
How to contact Medicare about ALJ hearing?
You can find more information about the ALJ hearing process at the Office of Medicare Hearings and Appeals website, or call us at 1-800-MEDICARE (1-800-633-4227).
How much is the minimum amount for a hearing in 2021?
To get a hearing or review by OMHA, the amount of your case must meet a minimum dollar amount. For 2021, the required minimum amount is $180. The "Reconsidered Determination" may include a statement that tells you if your case is estimated to meet the minimum dollar amount.
What happens if you ask OMHA for a decision without a hearing?
If you have asked OMHA for a decision without a hearing, but the ALJ decides a hearing is necessary, the ALJ will let you know when the hearing will be. If no hearing is held, either an ALJ or attorney adjudicator will review the information in your appeal record and issue a decision.
What is the waiver of right to an ALJ hearing?
The "Waiver of Right to an Administrative Law Judge (ALJ ) Hearing" form (Form OMHA-104). A written request stating that you don't wish to appear before an ALJ at a hearing (including a hearing held by phone or video-teleconference) Even if you waive the ALJ hearing, a hearing may still be held by an ALJ if the other parties in your case who were ...
Can an OMHA make a decision without a hearing?
You can ask OMHA to make a decision without holding a hearing (based only on the information that's in your appeal record). The ALJ or attorney adjudicator may also issue a decision without holding a hearing if evidence in the hearing record supports a decision that's fully in your favor.
Can you waive an ALJ hearing?
Even if you waive the ALJ hearing, a hearing may still be held by an ALJ if the other parties in your case who were sent a notice of hearing (for example, your provider) don’t also waive the ALJ hearing, or if the ALJ believes a hearing is necessary to decide your case.
What is the ABN for Medicare?
If you have Original Medicare and your doctor, other health care provider, or supplier thinks that Medicare probably (or certainly) won’t pay for items or services, he or she may give you a written notice called an ABN (Form CMS-R-131).
What to do if you are not satisfied with the IRE decision?
If you’re not satisfied with the IRE’s reconsideration decision, you may request a decision by OMHA, based on a hearing before an Administrative Law Judge (ALJ) or, in certain circumstances, a review of the appeal record by an ALJ or an attorney adjudicator.
How long does it take for an IRE to review a case?
They must get this information within 10 days after the date you get the notice telling you your case file has been sent to the IRE. The IRE’s address is on the notice.
Does CMS exclude or deny benefits?
The Centers for Medicare & Medicaid Services (CMS) doesn’t exclude, deny benefits to, or otherwise discriminate against any person on the basis of race, color, national origin, disability, sex, or age in admission to, participation in, or receipt of the services and benefits under any of its programs and activities, whether carried out by CMS directly or through a contractor or any other entity with which CMS arranges to carry out its programs and activities.
Do doctors have to give advance notice of non-coverage?
Doctors, other health care providers, and suppliers don’t have to (but still may) give you an “Advance Beneficiary Notice of Noncoverage” for services that Medicare generally doesn’t cover, like:
What does "I" mean in CMS?
In a 2019 Final Rule, CMS ended the requirement that appellants sign their appeal requests.In this booklet, “I” or “you” refers to patients, parties, and appellants active in an appeal.
Can a patient transfer their appeal rights?
Patients may transfer their appeal rights to non-participating providers or suppliers who provide the items or services and don’t otherwise have appeal rights. To transfer appeal rights, the patient and non-participating provider or supplier must complete and sign the
How many levels of appeal are there for Medicare?
There are five levels of appeal for services under original Medicare, and your claim can be heard and reviewed by several different independent organizations. Here are the levels of the appeal process: Level 1. Your appeal is reviewed by the Medicare administrative contractor. Level 2.
What happens if Medicare Appeals Council isn't in your favor?
If the decision of the Medicare Appeals Council isn’t in your favor, you can present your case to a judge in federal district court. The amount of money you’re asking Medicare to pay must meet a set amount to proceed with an appeal in court.
What to do if Medicare won't pay for your care?
If Medicare won’t cover your care, you can start the appeals process then. Pay for your continued care out of pocket.
What is the Medicare number?
your Medicare number (as shown on your Medicare card) the items you want Medicare to pay for and the date you received the service or item. the name of your representative if someone is helping you manage your claim. a detailed explanation of why Medicare should pay for the service, medication, or item.
How long does it take for Medicare to issue a decision?
The Office of Medicare Hearings and Appeals should issue a decision in 90 to 180 days. If you don’t agree with the decision, you can apply for a review by the Medicare Appeals Council.
What happens if Medicare refuses to pay for medical care?
If Medicare refuses to cover care, medication, or equipment that you and your healthcare provider think are medically necessary, you can file an appeal. You may also wish to file an appeal if Medicare decides to charge you with a late enrollment penalty or premium surcharge.
How to communicate with Medicare?
If you communicate with Medicare in writing, name your representative in the letter or e-mail. Know that you can hire legal representation. If your case goes beyond an initial appeal, it may be a good idea to work with a lawyer who understands Medicare’s appeals process so your interests are properly represented.
How long does it take to appeal a medical insurance decision?
You can start your appeal by following the instructions on the Notice of Denial of Medical Coverage and filing your appeal within 60 days of the date on this notice.
What to do if you are dissatisfied with Medicare Advantage?
If you are dissatisfied with your Medicare Advantage or Part D prescription drug plan for any reason, you can choose to file a grievance. A grievance is a formal complaint that you file with your plan. It is not an appeal.
What happens if you appeal a MAC denial?
If your appeal is successful, your service or item will be covered. If your appeal is denied, you can move on to the next level by following the instructions on the MAC denial notice. Remember that you can always contact your SHIP for individualized counseling and assistance regarding Medicare denials and appeals.
What to do if denied coverage for a health care service?
Let’s understand what to do if you are denied coverage for a health care service or item. Before you start your appeal, make sure you read all the letters and notices sent by Medicare or your plan.
What is the first level of Medicare appeal?
The first level of an appeal for Original Medicare is called a redetermination . A redetermination is performed by the same contractor that processed your Medicare claim. However, the individual that performs the appeal is not the same individual that processed your claim. The appeal is a new and independent review of your claim.
How long does it take to appeal Medicare?
See the Medicare Summary Notice you received in the mail; your appeal rights are on the last page or back. You can request an appeal within 120 days from the date you received the Medicare Summary Notice.
Who does Medicare contract with?
Your doctor or hospital submits a bill to Medicare. Medicare contracts with private companies (" contractors ") to process medical claims (bills) for health care items and services provided to Medicare beneficiaries.
Is OMHA responsible for levels 1 and 2?
OMHA is not responsible for levels 1, 2, 4, and 5 of the appeals process. OMHA provides additional information on other levels of appeals to help you understand the appeals process in a broad context. Content created by Office of Medicare Hearings and Appeals (OMHA) Content last reviewed on August 5, 2016.
What happens if OMHA does not issue a decision?
If OMHA does not issue a decision, a dismissal, or remand order within the adjudication period specified (with exceptions for timeframe extensions noted), the appellant may send a request to OMHA asking that the appeal, other than an appeal of a QIC dismissal, be escalated to the Council.
When can an ALJ request a reconsideration?
When a request for an ALJ hearing is filed after a QIC has issued a reconsideration, an ALJ or attorney adjudicator issues a decision, dismissal order, or remand to the QIC, as appropriate, no later than the end of the 90 calendar day period beginning on the date the request for hearing is received by the office specified in the QIC's notice of reconsideration, unless the 90 calendar day period has been extended. This timeframe may be extended for a variety of reasons including, but not limited to:
How long does it take for an OMHA to issue a remand order?
After OMHA receives a valid request for escalation, they will issue a decision, dismissal, or remand order if an OMHA adjudicator is able to issue one within 5 calendar days of receiving the request for escalation, or 5 calendar days from the end of the applicable adjudication period (whichever is later).
