What is the deadline for filing a Medicare claim?
These include:
- Applicable law requires a longer filing period
- Provider agreement specifically allows for additional time
- In Coordination of Benefits situations, timely filing is determined from the processing date indicated on the primary carrier's explanation of benefits (EOB) or explanation of payment (EOP)
Is there a time limit for filing for Medicare?
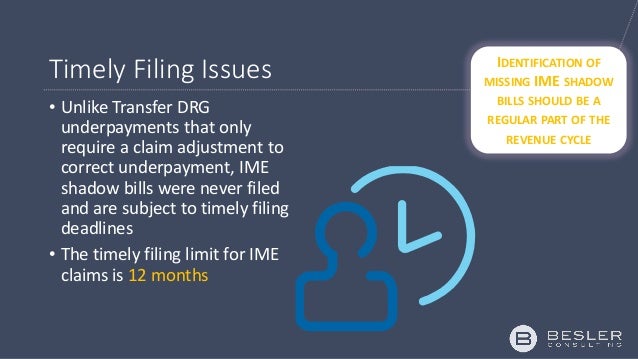
What is the time limit for submission of a Medicare claim? Medicare claims must be filed no later than 12 months (or 1 full calendar year) after the date when the services were provided. If a claim isn’t filed within this time limit, Medicare can’t pay its share.
What is meritain health timely filing limit?
When you partner with meritain health, an aetna company, you help The timely filing limit for aetna is now only 90 days Most providers have 120 days from the date of service to file a claim. But the world's not perfect. Sometimes you get the wrong insurance information. Sometimes you send in the claim but for some reason, we didn't get it.
How to manually file a claim with Medicare?
- A copy of the bill
- Your Medicare information
- The doctor’s NPN (call the doctor who treated you and ask them for it)
What is timely filing limit?
In medical billing, a timely filing limit is the timeframe within which a claim must be submitted to a payer. Different payers will have different timely filing limits; some payers allow 90 days for a claim to be filed, while others will allow as much as a year.
Is there a limit on Medicare claims?
In general, there's no upper dollar limit on Medicare benefits. As long as you're using medical services that Medicare covers—and provided that they're medically necessary—you can continue to use as many as you need, regardless of how much they cost, in any given year or over the rest of your lifetime.
What is timely filing limit for Unitedhealthcare?
within 90 daysYou should submit a request for payment of Benefits within 90 days after the date of service. If you don't provide this information to us within one year of the date of service, Benefits for that health service will be denied or reduced, as determined by us.
Can I submit a paper claim to Medicare?
The Administrative Simplification Compliance Act (ASCA) requires that as of October 16, 2003, all initial Medicare claims be submitted electronically, except in limited situations. Medicare is prohibited from payment of claims submitted on a paper claim form that do not meet the limited exception criteria. web page.
How are Medicare days counted?
A part of a day, including the day of admission and day on which a patient returns from leave of absence, counts as a full day. However, the day of discharge, death, or a day on which a patient begins a leave of absence is not counted as a day unless discharge or death occur on the day of admission.
What is a benefit period in Medicare?
A benefit period begins the day you're admitted as an inpatient in a hospital or SNF. The benefit period ends when you haven't gotten any inpatient hospital care (or skilled care in a SNF) for 60 days in a row. If you go into a hospital or a SNF after one benefit period has ended, a new benefit period begins.
What is Medicare timely filing Aetna?
We require providers to submit claims within 180 days from the date of service unless otherwise specified within the provider contract.
What is the timely filing limit for Aetna?
We've changed the standard nonparticipating-provider timely filing limit from 27 months to 12 months for traditional medical claims.
What is timely filing for Cigna?
The claim must be received within 120 days from date of service to be considered timely.
Does Medicare accept handwritten claims?
Medicare to Reject Handwritten Claims. Providers who wish to continue to submit paper claims may do so as long as they are printed and as long as the only handwriting included in the claim is in a signature field. Software programs are available that will allow providers to print information into a CMS 1500 form.
What is the difference between paper claims and electronic claims?
Paper claims that are almost obsolete are still used by certain payers. To send out paper claims, billers will have to enter claim details in the forms provided by insurance companies and send the completed details across. In contrast electronic claims are created and sent to clearinghouses/insurers via their EHRs.
What is the difference between CMS 1500 and ub04?
When a physician has a private practice but performs services at an institutional facility such as a hospital or outpatient facility, the CMS-1500 form would be used to bill for their services. The UB-04 (CMS-1450) form is the claim form for institutional facilities such as hospitals or outpatient facilities.
How long does it take for Medicare to extend a timely filing?
When this exception is met, timely filing will be extended six months following the month in which you or the beneficiary received notification of retroactive Medicare entitlement.
How long does it take to file a Medicare claim?
In general, Medicare claims must be filed to the Medicare claims processing contractor no later than 12 months, or 1 calendar year, from the date the services were furnished. This includes resubmitting corrected claims that were unprocessable.
What happens if a Medicare claim is late?
In this instance, you may only charge the beneficiary for deductible or coinsurance amounts that would have been applied if Medicare payment had been made .
What to do if you believe an administrative error leads to the untimely filing of a claim?
If you believe an administrative error lead to the untimely filing of a claim, please provide a statement from the beneficiary, their representative or yourself as to how the error was known, when it was corrected, and a written report by Medicare or the Medicare contractor describing how its error caused failure to file within the time limit; or copie s of a CMS or Medicare contractor letter or other written notice reflecting the error. There must be a clear and direct relationship between the administrative error and the late filing of the claim.
What is the through date on a claim?
For inpatient hospital or inpatient skilled nursing facility claims that report span dates of service, the “Through” date on the claim is used to determine timely filing.
How many exceptions does CMS allow?
The CMS allows four exceptions to timely filing. Let’s discuss each of the four exceptions.
Can you waive Medicare if you don't know if you have Medicare?
Best practice: Obtain all medical insurance cards from the Medicare beneficiary. Not knowing a patient had Medicare or not knowing that Medicare should have been primary is not grounds to waive timely filing. Ask the patient if they are entitled to Medicare and if Medicare is primary or secondary.
What happens if claims are submitted after the time frame?
If claims submitted after the timely frame set by insurances, then those claims will be denied by insurance companies as CO 29-The time limit for filing has expired.
What to do if claim history states the claim was submitted to wrong insurance or submitted to the correct insurance but not received?
If claim history states the claim was submitted to wrong insurance or submitted to the correct insurance but not received, appeal the claim with screen shots of submission as proof of timely filing (POTF) and copy of clearing house acknowledgement report can also be used.
How long does Medicare have to file a claim?
As a result of the Patient Protection and Affordable Care Act (PPACA), all claims for services furnished on/after January 1, 2010, must be filed with your Medicare Administrative Contractor (MAC) no later than one calendar year (12 months) from the date of service (DOS) or Medicare will deny the claim.
What is the "from" and "through" date on a claim?
For institutional claims that include span DOS (i.e., a "From" and "Through" date on claim), "Through" date on claim is used for determining DOS for claims filing timeliness
What is the time limit for filing a claim?
Timely filing limit is the time duration from service rendered to patients and submitting claims to the insurance companies. For example, if any patient getting services on the 1st of any month then there is a time limit to submit his/her claim to the insurance company for reimbursement. It is 30 days to 1 year and more and depends on insurance companies.
When do you have to submit a claim for MHBP?
The claim must submit by December 31 of the year after the year patient received the service, unless timely filing was prevented by administrative operations of the Government or legal incapacity. Once we pay benefits, there is a three-year limitation on the re-issuance of uncashed checks. Claim Address- MHBP Medical Claims PO Box 8402 London, KY 40742
How long does it take to file a CO 29?
It is 30 days to 1 year and more and depends on insurance companies. The patient or medical billing agency’s responsibility to submit his/her claim to insurance within the timely filing limit otherwise claims will be denied due to timely filing exceeded (CO-29).
How long do you have to file a claim with Medicare?
A: Per Medicare guidelines, claims must be filed with the appropriate Medicare claims processing contractor no later than 12 months (one calendar year) after the date of service (DOS). Claims must be processed (paid or denied/rejected) by Medicare to be considered filed/submitted. Claims with missing, invalid or incomplete information that prevents Medicare from processing them, also known as "returned to provider/RTPs" (Part A) and "return unprocessable claims/RUCs" (Part B), are NOT considered filed/submitted. RUCs and RTPs must be corrected and resubmitted for processing. Claims submitted after one calendar year from the DOS will be denied or rejected.
How long does it take for Medicare to process a claim?
A: Per Medicare guidelines, claims must be filed with the appropriate Medicare claims processing contractor no later than 12 months (one calendar year) after the date of service (DOS). Claims must be processed (paid or denied/rejected) by Medicare to be considered filed/submitted.