
Full Answer
What does UHC cost and who will pay?
health factors, with no cost-sharing. The preventive care services covered are those preventive services specified in the health care reform law. UnitedHealthcare also covers other routine services, which may require a copayment, coinsurance or deductible. Always refer to your plan documents for your specific coverage.
What is Medicare complete United Healthcare Plan?
What is Medicare Complete by United Healthcare? MedicareComplete is the brand name for UnitedHealthcare’s family of Medicare Advantage plans, many of which also carry the AARP brand. At a minimum, they offer the same coverage as Medicare Parts A and B and in some cases also include a prescription drug component.
What is Medicare dual complete?
What type of coverage do you get if you are dual eligible for Medicare and Medicaid?
- Qualified Medicare Beneficiary (QMB) Program. This program helps pay for Medicare Part A and Part B premiums, deductibles, coinsurance and copayments.
- Specified Low-Income Medicare Beneficiary (SLMB) Program. The SLMB program helps pay for Medicare Part B premiums.
- Qualifying Individual (QI) Program. ...
- Qualified Disabled Working Individual (QDWI) Program. ...
What is AARP Medicare complete?
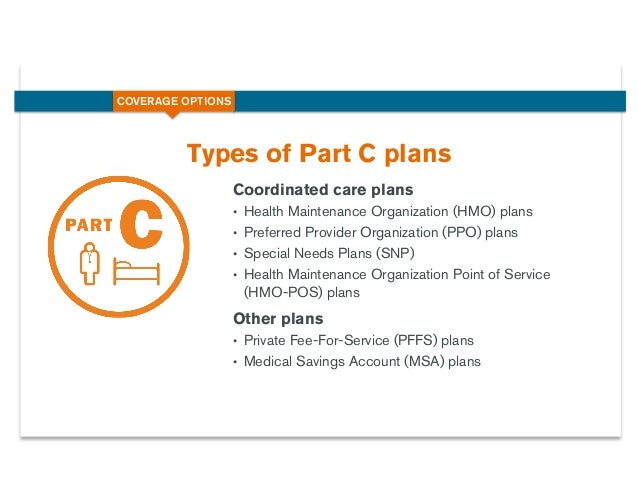
The AARP Medicare complete plan is a type of Medicare advantage policy, and not a Medicare supplement. Medicare advantage also goes by the name of Part C, which is a combination of traditional Medicare benefits and a private insurance policy merged together to provide an all-in-one plan for seniors.
What is the difference between Medicare Advantage and Medicare Complete?
Consider if you want coverage for dental, vision and other extra benefits. Medicare Advantage plans cover everything Original Medicare covers plus more, so if you want things like dental, vision or fitness benefits, a Medicare Advantage plan may be the right choice. Think about what your total costs could be.
What UHC complete?
A UnitedHealthcare Dual Complete plan is a DSNP that provides health benefits for people who are “dually-eligible,” meaning they qualify for both Medicare and Medicaid. Who qualifies? Anyone who meets the eligibility criteria for both Medicare and Medicaid is qualified to enroll in a DSNP.
What are 4 types of Medicare plans?
There are four parts of Medicare: Part A, Part B, Part C, and Part D.Part A provides inpatient/hospital coverage.Part B provides outpatient/medical coverage.Part C offers an alternate way to receive your Medicare benefits (see below for more information).Part D provides prescription drug coverage.
What is the difference between AARP Medicare Complete and AARP Medicare Advantage?
About AARP Dental Insurance AARP MedicareComplete plans are forms of Medicare Advantage health care insurance plans. Medicare Advantage plans are offered through private companies, which develop agreements with Medicare to provide some Medicare benefits to those who sign up with them.
What is UnitedHealthcare dual complete choice?
UnitedHealthcare Dual Complete Special Needs Plans (SNP) offer benefits for people with both Medicare and Medicaid. These SNP plans provide benefits beyond Original Medicare, such as transportation to medical appointments and routine vision exams.
Is UHC dual complete a Medicare replacement plan?
That includes both inpatient and outpatient care and durable medical equipment (DME). As a Medicare Advantage plan, UHC Dual Complete plans can also cover benefits that Original Medicare doesn't cover, such as hearing, vision, dental and prescription drug coverage covered by Medicare Part D.
What are the top 3 Medicare Advantage plans?
Best Medicare Advantage Providers RatingsProviderForbes Health RatingsCMS ratingHumana5.03.6Blue Cross Blue Shield5.03.8Cigna4.53.8United Healthcare4.03.81 more row•Feb 25, 2022
What is the most popular Medicare Advantage plan?
AARP/UnitedHealthcare is the most popular Medicare Advantage provider with many enrollees valuing its combination of good ratings, affordable premiums and add-on benefits. For many people, AARP/UnitedHealthcare Medicare Advantage plans fall into the sweet spot for having good benefits at an affordable price.
What parts of Medicare are free?
Part A covers inpatient hospital stays, care in a skilled nursing facility, hospice care, and some home health care. coverage if you or your spouse paid Medicare taxes for a certain amount of time while working. This is sometimes called "premium-free Part A." Most people get premium-free Part A.
What is the biggest disadvantage of Medicare Advantage?
Medicare Advantage can become expensive if you're sick, due to uncovered copays. Additionally, a plan may offer only a limited network of doctors, which can interfere with a patient's choice. It's not easy to change to another plan. If you decide to switch to a Medigap policy, there often are lifetime penalties.
Is AARP Medicare Complete the same as Medicare?
MedicareComplete is the brand name for UnitedHealthcare's family of Medicare Advantage Plans, many of which also carry the AARP brand. At a minimum, they offer the same coverage as Medicare Parts A and B, and in some cases include a prescription drug component as well.
Can you switch from Medicare Advantage back to Original Medicare?
Yes, you can elect to switch to traditional Medicare from your Medicare Advantage plan during the Medicare Open Enrollment period, which runs from October 15 to December 7 each year. Your coverage under traditional Medicare will begin January 1 of the following year.
What is Medicare Supplement Insurance Plan?
Medicare Supplement Insurance Plan. Also called Medigap, these plans help cover some out-of-pocket costs not paid by Original Medicare. Medicare Prescription Drug Plans (Part D) This plan helps pay for prescription drugs and can be used with Original Medicare or Medicare Supplement plans. Get to know Medicare.
What is Medicare insurance?
Medicaid. Medicare insurance plans. Medicare insurance plans are for people 65 or older — or for those who may qualify because of a disability or special condition.
How old do you have to be to qualify for Medicare?
You’re under age 65 and qualify on the basis of disability or other special situation. You’re at least 65 years old and receive extra help or assistance from your state. These plans offer benefits and features beyond Original Medicare, which might also include transportation assistance and prescription drug coverage.
Is UnitedHealthcare a Medicare Advantage?
Plans are insured through UnitedHealthcare Insurance Company or one of its affiliated companies, a Medicare Advantage organization with a Medicare contract. Enrollment in the plan depends on the plan’s contract renewal with Medicare.
What is Medicare Advantage Plan?
Medicare Advantage Plans are substitutes for Original Medicare coverage and were authorized by Congress to shift some of Medicare's cost burden to private insurance companies. Medicare participants who enroll in a Medicare Advantage Plan are covered directly by the private insurance company offering it, to which Medicare pays a premium.
How much is Medicare Part B coinsurance?
For Part B services, most MedicareComplete plans require coinsurance payments, usually a flat-rate amount of $15 to $25, rather than the Original Medicare Part B deductible of 20 percent.
What is a preferred provider organization?
In a PPO, the insurance company pays a portion of charges from out-of-network providers, but at a much lower rate than for in-network.
Does HMO cover out of network?
Health maintenance organization. In an HMO, the insurance company covers the charges only for health care providers in the network; if you go out-of-network for service , those charges won't be covered at all.
Can you turn down Medicare Advantage?
These plans are "guaranteed issue" -- that is, you cannot be turned down for Medicare Advantage or MA-PD coverage, unless you have end-stage renal disease. 00:00. 00:04 08:24.
How to report incorrect information on UnitedHealthcare?
To report incorrect information, email [email protected]. This email box is for members to report potential inaccuracies for demographic (address, phone, etc.) information in the online or paper directories. Reporting issues via this mail box will result in an outreach to the provider’s office to verify all directory demographic data, which can take approximately 30 days. Individuals can also report potential inaccuracies via phone. UnitedHealthcare Members should call the number on the back of their ID card, and non-UnitedHealthcare members can call 888-638-6613 TTY 711.
What is Medicare Advantage?
An alternative to Original Medicare is a Medicare Advantage plan from a private insurance company.
What is a SCO plan?
UnitedHealthcare SCO is a Coordinated Care plan with a Medicare contract and a contract with the Commonwealth of Massachusetts Medicaid program. Enrollment in the plan depends on the plan’s contract renewal with Medicare. This plan is a voluntary program that is available to anyone 65 and older who qualifies for MassHealth Standard and Original Medicare. If you have MassHealth Standard, but you do not qualify for Original Medicare, you may still be eligible to enroll in our MassHealth Senior Care Option plan and receive all of your MassHealth benefits through our SCO program.
What rating system does Medicare use?
Medicare evaluates plans based on a 5-Star rating system.
Does Medicare pay for long term care?
Like most other insurance programs, Original Medicare and Medicare Advantage Plans do not pay for all health care costs. You must pay for deductibles, premiums, coinsurance or copayments. Original Medicare and Medicare Advantage Plans do not pay for long-term care, extended stays in nursing homes or coverage when outside of the country.
Does Medicare Advantage include prescription drug coverage?
Some Medicare Advantage Plans include prescription drug coverage. Or you can enroll in a Medicare Part D plan as an alternative way to get prescription drug coverage. The options you choose affect the cost and level of your coverage.
What is a dual medical plan?
Dual health plans cover eligible doctor visits, hospital stays and prescription drugs. If you have Medicare and Medicaid, chances are you could qualify for a Dual Special Needs Plan (D-SNP). Learn more about D-SNP plans. Find the right Medicare coverage for you.
What is Medicare Supplement insurance?
What are Medicare Supplement insurance plans? Medicare Supplement insurance (sometimes referred to as "Medigap") works with Original Medicare to pay some of the out-of-pocket costs that Parts A and B alone do not.
What is Medicare for seniors?
Medicare is the federal health insurance program for people who are 65 or older, or those under 65 who may qualify because of a disability or another special situation. Medicare helps millions of American seniors and disabled individuals cover some of their health care costs.
Does Medicare cover vision?
Medicare also offers important choices in how you receive benefits – whether through Original Medicare or through a Medicare-approved private insurer that offers prescription drug coverage and additional benefits like vision, hearing, dental, and more. The different parts of Medicare help cover the costs of specific services.
Does Medicare Advantage cover eye exams?
Most Medicare Advantage plans combine hospital, doctor, and drug coverage in one plan, and may include other benefits and features not offered by Original Medicare, including eye exams, eye glasses and corrective lenses, dental exams, cleanings and X-rays, hearing tests and hearing aids, wellness programs and fitness benefits.
How does dual coverage work with Medicare?
How does dual coverage health insurance work with both Medicaid and Medicare? A Dual Special Needs Plan works together with your Medicaid health plan. You’ll keep all your Medicaid benefits. Most dual health insurance plans also give you more benefits and features than you get with Original Medicare.
How to report incorrect information on UnitedHealthcare?
To report incorrect information, email [email protected]. This email box is for members to report potential inaccuracies for demographic (address, phone, etc.) information in the online or paper directories. Reporting issues via this mail box will result in an outreach to the provider’s office to verify all directory demographic data, which can take approximately 30 days. Individuals can also report potential inaccuracies via phone. UnitedHealthcare Members should call the number on the back of their ID card, and non-UnitedHealthcare members can call 888-638-6613 TTY 711.
What rating system does Medicare use?
Medicare evaluates plans based on a 5-Star rating system.
What is a dual special needs plan?
Dual Special Needs Plans are for people who could use some extra help. That may be because of income, disabilities, age and/or health conditions. Dual Special Needs Plans are a type of Medicare Advantage plan. Dual Special Needs Plans are also called D-SNP for short. These names all mean the same thing.
What is a SCO plan?
UnitedHealthcare SCO is a Coordinated Care plan with a Medicare contract and a contract with the Commonwealth of Massachusetts Medicaid program. Enrollment in the plan depends on the plan’s contract renewal with Medicare. This plan is a voluntary program that is available to anyone 65 and older who qualifies for MassHealth Standard and Original Medicare. If you have MassHealth Standard, but you do not qualify for Original Medicare, you may still be eligible to enroll in our MassHealth Senior Care Option plan and receive all of your MassHealth benefits through our SCO program.
What is a Medicare cover summary?
The Coverage Summaries are policies based on existing current Medicare National Coverage Determinations, Local Coverage Determinations, UnitedHealthcare Medical Policies, and applicable UnitedHealthcare Medicare Advantage Plans EOCs and SOBs intended to provide benefit coverage information and guidelines specific to UnitedHealthcare Medicare Advantage Plans . The Coverage Summaries are developed and reviewed by the UnitedHealthcare Medicare Benefit Interpretation Committee. Benefit interpretations for UnitedHealthcare Medicare Advantage Plan members are made on a case-by-case basis using the guidelines in the Coverage Summaries. The Coverage Summaries are subject to change based upon changes in Medicare's coverage requirements, changes in scientific knowledge and technology and evolving practice patterns. Providers are responsible for reviewing the CMS Medicare Coverage Center guidance and in the event that there is a conflict between the Coverage Summaries and the CMS Medicare Coverage Center guidance, the CMS Medicare Coverage Center guidance will govern.
Where is the provider service number on a health card?
For questions, please contact your local Network Management representative or call the Provider Services number on the back of the member’s health ID card.
Who makes medical necessity determinations?
Medical necessity determinations must be made by trained and/or licensed professional medical personnel only . UnitedHealthcare Medicare Advantage Plan members have the right to appeal benefit decisions in accordance with Medicare guidelines as outlined in the UnitedHealthcare Medicare Advantage Plans EOC or SOB.
Do medical necessity determinations have to be made by trained and/or licensed professional medical personnel?
Medical necessity determinations must be made by trained and/or licensed professional medical personnel only.
Can you appeal a Medicare Advantage Plan decision?
UnitedHealthcare Medicare Advantage Plan members have the right to appeal benefit decisions in accordance with Medicare guidelines as outlined in the UnitedHealthcare Medicare Advantage Plans EOC or SOB. Any questions regarding appeals should be directed to the UnitedHealthcare Medicare Advantage Plans Appeals Department identified on the members' identification card.
