Medicare Part B (Medical Insurance) covers some diabetes supplies, including: Blood sugar (glucose) testing monitors. Blood sugar test strips. Insulin. Lancet devices and lancets.
Full Answer
Which glucose meters are covered by Medicare?
Blood Sugar Monitor Coverage Blood sugar monitors Medicare Part B (Medical Insurance) covers blood sugar (glucose) monitors as durable medical equipment (DME) that your doctor prescribes for use in your home. Your costs in Original Medicare After you meet the Part B Deductible , you pay 20% of the Medicare-Approved Amount (if your supplier accepts
Are glucometers covered by Medicare?
Mar 28, 2018 · Original Medicare Part B covers some diabetic supplies, including: Blood sugar (glucose) test strips Blood glucose monitors, lancet devices, and lancets Glucose control solutions for checking the accuracy of test strips and monitors Insulin if you are using a medically necessary insulin pump (see below) Therapeutic shoes or inserts (see below) There may be …
Is glucometer covered by insurance?
Sep 10, 2018 · Medicare treats glucose monitors and blood sugar test strips as durable medical equipment (DME) under Medicare Part B. If your physician prescribes glucose monitoring at home, your durable medical equipment costs are generally covered at 80 percent of the Medicare-approved amount, once your deductible is met.
Does Medicare cover glucose monitors?
Jan 15, 2022 · Medicare also covers the Dexcom G5 CGM, which is another continuous glucose monitoring system. The Dexcom G5 and FreeStyle Libre are different than insulin pumps, which can monitor and administer insulin. Medicare also covers some types of insulin pumps. A person can talk to their doctor about what monitoring approach may be best for them.
What brand of glucose meter is covered by Medicare 2021?
A2: Starting January 1, 2021, covered meters include: OneTouch Verio Reflect ®, OneTouch Verio Flex®, OneTouch Verio® and OneTouch Ultra 2®.
What brand of glucose meter does Medicare 2022 cover?
Accu-Chek ® is ALWAYS COVERED on Medicare Part B.
What brand of glucose meter does Medicare 2020 cover?
This just in: Medicare will now cover Abbott's FreeStyle Libre real-time continuous glucose monitoring (CGM) system.Jan 4, 2018
Does Medicare cover the cost of glucose meters?
If you use insulin and require frequent adjustments to your insulin regimen/ dosage, Medicare may cover a continuous glucose monitor if your doctor determines that you meet all of the requirements for Medicare coverage, including the need to frequently check your blood sugar (4 or more times a day) and the need to ...
How many diabetic test strips will Medicare pay for?
Medicare Part B covers the same type of blood glucose testing supplies for people with diabetes whether or not they use insulin. However, the amount of supplies that are covered varies. Uses insulin, they may be able to get up to 100 test strips and lancets every month, and 1 lancet device every 6 months.Aug 16, 2018
Does Medicare cover glucometer for prediabetes?
Medicare may bill you for any diagnostic care you receive during a preventive visit. Part B also covers certain diabetic supplies, including: Glucose monitors. Blood glucose test strips.
Does Medicare Part B pay for diabetic test strips?
Part B covers certain doctors' services, outpatient care, medical supplies, and preventive services. covers some diabetic test supplies, including blood sugar test strips, as durable medical equipment (DME). for these: Most doctor services (including most doctor services while you're a hospital inpatient)
Does Medicare pay for A1c test?
Hemoglobin A1c Tests: Your doctor might order a hemoglobin A1c lab test. This test measures how well your blood glucose has been controlled over the past 3 months. Medicare may cover this test for anyone with diabetes if it is ordered by his or her doctor.
Is Livongo covered by Medicare?
The Centers for Medicare and Medicare Services has recognized chronic disease management company Livongo as an enrolled provider for Medicare Advantage members, the startup announced this morning in a release.Apr 30, 2019
Does Medicare cover CGM type 2 diabetes?
Yes. The Dexcom G6 Continuous Glucose Monitoring (CGM) System is covered by Medicare for patients who meet the Medicare coverage criteria. Medicare coverage for therapeutic CGM includes certain beneficiaries who have either type 1 or type 2 diabetes and intensively manage their insulin.Jan 31, 2022
Does Medicare cover diabetic test strips 2022?
If you've met your Part B deductible (which is $233 in 2022), you will pay 20 percent of the Medicare-approved amount for diabetic testing supplies. Medicare pays the other 80 percent. Depending on the type of equipment or supplies you need, you may need to: rent the equipment.Nov 19, 2021
Does Medicare Cover One Touch test strips?
OneTouch® test strips are ALWAYS covered on Medicare Part B and $0 with most supplemental health plans. * With their red, white and blue Medicare Part B card alone, your patients pay just $1.66 for a box of 50ct test strips.
What Are Glucose Monitors Used for?
If you have been diagnosed with diabetes, a glucose monitor can help you manage your disease and prevent complications, according to the National I...
Medicare Coverage of Glucose Monitors
Under Original Medicare (Part A and Part B), Part A covers health-care expenses you incur as an inpatient in a hospital, while Part B covers your o...
How Does Medicare Treat Durable Medical Equipment?
Medicare treats glucose monitors and blood sugar test strips as durable medical equipment (DME) under Medicare Part B. If your physician prescribes...
Are There Other Options For Medicare Coverage of Glucose Monitors?
Some Medicare beneficiaries choose to receive their Original Medicare benefits (except hospice care) through the Medicare Advantage (Medicare Part...
Would You Like to Know More About Medicare Coverage of Glucose Monitors?
If you have questions about Medicare coverage for home glucose monitors, or would like more information about Medicare plan options to help you bet...
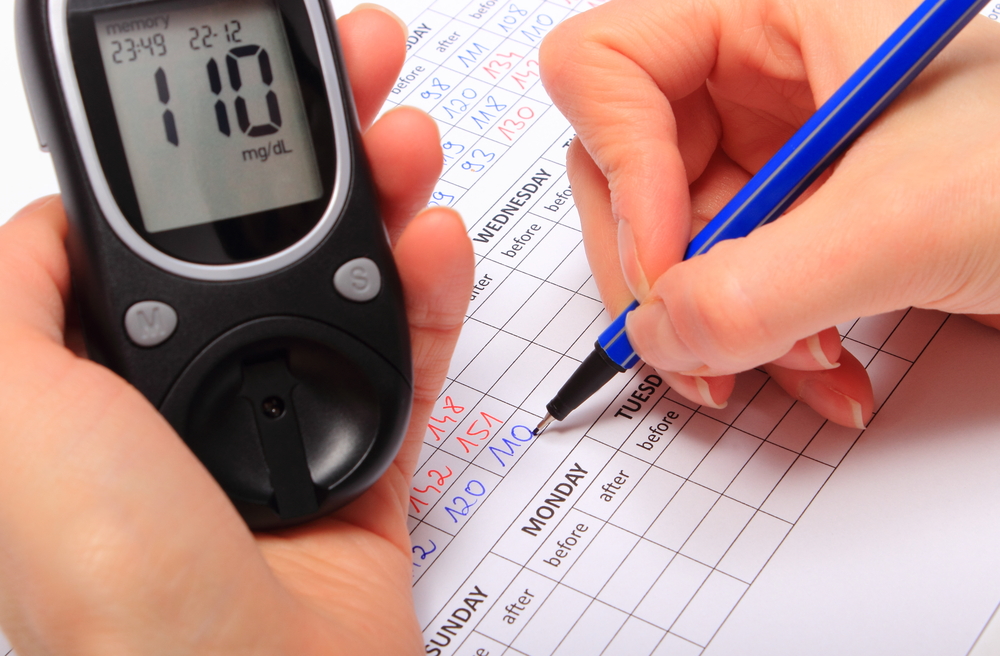
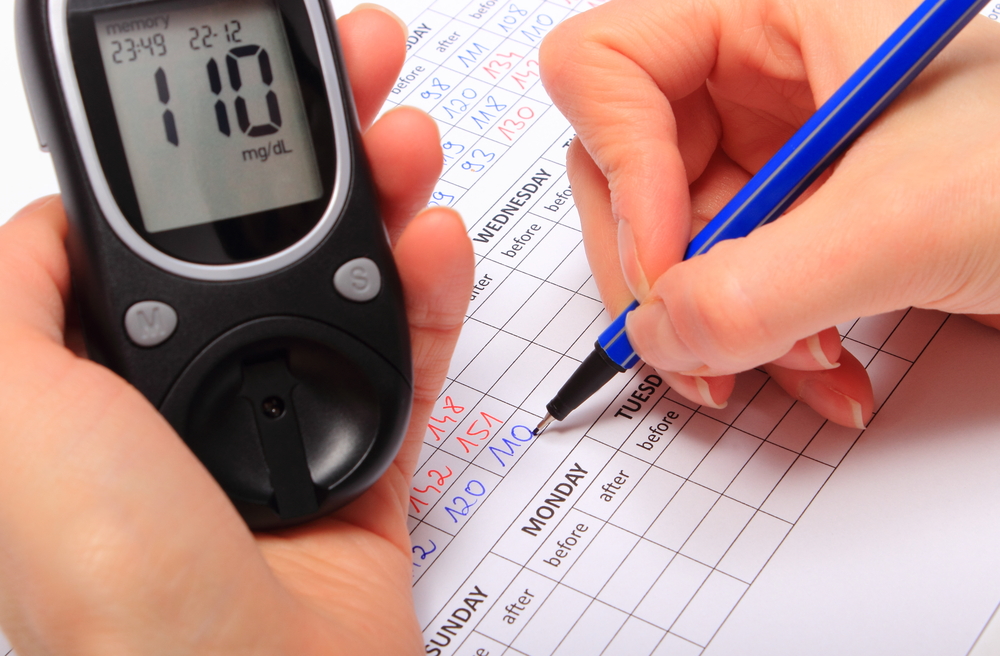
What is a glucose monitor?
A glucose monitor measures your blood sugar (glucose) levels so you can make informed decisions about eating, exercising, and taking prescription medications, such as insulin. According to the NIH, one way to monitor your glucose levels is by using a finger-stick device to collect a drop of blood, which you put into a glucose monitor on a set schedule each day. An alternative site glucose monitor allows blood samples from areas such as your palm or thigh, according to the Mayo Clinic. As well as a glucose monitor, you may also need other testing supplies, such as lancets, glucose test strips, and a glucose control solution. Medicare coverage of glucose monitors Under Original Medicare (Part A and Part B), Part A covers health-care expenses you incur as an inpatient in a hospital, while Part B covers your outpatient care, including some glucose monitoring supplies and durable medical equipment. Medicare does not generally cover “continuous glucose monitoring,” which (according to the NIH) involves a sensor inserted under your skin for several days to a week. If your health-care provider recommends a different way to monitor your blood sugar other than the finger-stick glucose monitor, you might want to check with Medicare to see whether it’s covered. You can reach a Medicare representative 24 hours a day, seven days a week, if you call 1-800-MEDICARE (1-800-633-4227). TTY users can call 1-877-486-2048. If you have a Medicare Advantage plan, call your plan to ask about this coverage. How does Medicare treat durable medical equipment Continue reading >>
How many pairs of shoes does Medicare cover?
Medicare Part B covers one pair of custom-molded shoes (including inserts) or one pair of depth-inlay shoes per calendar year. Medicare also covers two additional pairs of inserts each calendar year for custom-molded shoes and three pairs of inserts each calendar year for depth-inlay shoes.
What are the preferred test strips for Ascensia?
For Abbott monitors, the preferred test strips include FreeStyle®, FreeStyle Lite®, and Precision Xtra®. For Ascensia monitors, the preferred test strips include Contour®, Contour®NEXT, Breeze®2, Elite®, and Autodisc®. Prior Authorization Required If your patient chooses to use a test strip that is not FreeStyle, FreeStyle Lite, Precision Xtra, Contour, Contour®NEXT, Breeze 2, Elite, or Autodisc, you will need to complete a prior authorization form on your patient’s behalf. If the prior authorization is not approved, the non-preferred test strips will not be a covered pharmacy benefit for your patient, and he or she will be responsible for the entire cost of the test strips. If the request for the non-preferred test strips is approved, your patient will be charged the highest level of cost-sharing. Free Blood Glucose Meters Both Abbott and Ascensia blood glucose meters are available at no cost to our members. Below is a comparison chart of important features of the blood glucose meters and corresponding test strips. The preferred brands rank high in patient satisfaction and can be used in several test sites, as listed below. Abbott Diabetes Care Ascensia Diabetes Care Blood Glucose Meter FreeStyle FreeStyle Freedom Lite Precision Xtra Contour Breeze 2 Contour® Next One Contour® Next EZ Contour® Next Sample size (uL) 0.3 0.3 0.6 0.6 1.0 0.6 0.6 0.6 Test time 5 seconds 5 seconds 5 seconds 5 seconds 5 seconds 5 seconds 5 seconds 5 seconds Approved test sites Fingertip, hand, forearm, upper arm, thigh, calf Fingertip, hand, forearm, Continue reading >>
Does Medicare pay for DME?
Medicare will only cover your DME if your doctors and DME suppliers are enrolled in Medicare. Doctors and suppliers have to meet strict standards to enroll and stay enrolled in Medicare. If your doctors or suppliers aren’t enrolled, Medicare won’t pay the claims submitted by them.
Does Medicare pay for blood sugar monitors?
How often is it covered? Medicare Part B (Medical Insurance) covers blood sugar monitors as durable medical equipment (DME) that your doctor prescribes for use in your home. Who's eligible? All people with Part B are covered. Your costs in Original Medicare If your supplier accepts assignment, you pay 20% of the Medicare-approved amount, and the Part B deductible applies. Medicare pays for different kinds of DME in different ways. Depending on the type of equipment: You may need to rent the equipment. You may need to buy the equipment. You may be able to choose whether to rent or buy the equipment. Medicare will only cover your DME if your doctors and DME suppliers are enrolled in Medicare. Doctors and suppliers have to meet strict standards to enroll and stay enrolled in Medicare. If your doctors or suppliers aren’t enrolled, Medicare won’t pay the claims submitted by them. It’s also important to ask your suppliers if they participate in Medicare before you get DME. If suppliers are participating suppliers, they must accept assignment. If suppliers are enrolled in Medicare but aren’t “participating,” they may choose not to accept assignment. If suppliers don't accept assignment, there’s no limit on the amount they can charge you. To find out how much your specific test, item, or service will cost, talk to your doctor or other health care provider. The specific amount you’ll owe may depend on several things, like: Other insurance you may have How much your doctor charges Whether your doctor accepts assignment The type of facility The location where you get your test, item, or service Continue reading >>
Does Medicare cover freestyle libre?
Coverage includes all Medicare patients with diabetes who use insulin and who meet the eligibility criteria2. The factory-calibrated FreeStyle Libre system is the only CGM system recognized by Medicare that requires no user calibration whatsoever (either by fingerstick or manual data entry).
Is Accu Chek covered by Medicare?
Stick with the brand you trust—don't let them switch your test strips! Some test strip suppliers may tell you otherwise, but Accu-Chek products are still covered by Medicare Part B at the same low co-pay1 as all other brands.2 They may even try switching you to another brand.
What percentage of Medicare deductible is covered for glucose monitoring?
If your physician prescribes glucose monitoring at home, your durable medical equipment costs are generally covered at 80 percent of the Medicare-approved. amount, once your deductible is met.
What is a glucose monitor?
A glucose monitor measures your blood sugar (glucose) levels so you can make informed decisions about eating, exercising, and taking prescription medications, such as insulin.
How to monitor glucose levels?
According to the NIH, one way to monitor your glucose levels is by using a finger-stick device to collect a drop of blood, which you put into a glucose monitor on a set schedule each day. An alternative site glucose monitor allows blood samples from areas such as your palm or thigh, according to the Mayo Clinic.
Does Medicare cover glucose monitoring?
Medicare does not generally cover “ continuous glucose monitoring,” which (according to the NIH) involves a sensor inserted under your skin for several days to a week. If your health-care provider recommends a different way to monitor your blood sugar other than the finger-stick glucose monitor, you might want to check with Medicare ...
Does Medicare cover hospice?
Part A covers hospice care when you have a Medicare Advantage plan. Medicare Advantage plans cover glucose monitors in the same way as Medicare Part B and often offer additional benefits, such as vision, dental, and prescription drug coverage. Some types of Medicare Advantage plans use provider networks, and may reduce the amounts you pay ...
What is Part B for diabetes?
In addition to diabetes self-management training, Part B covers medical nutrition therapy services if you have diabetes or renal disease. To be eligible for these services, your fasting blood sugar has to meet certain criteria. Also, your doctor or other health care provider must prescribe these services for you.
How long can you have Medicare Part B?
If you’ve had Medicare Part B for longer than 12 months , you can get a yearly “Wellness” visit to develop or update a personalized prevention plan based on your current health and risk factors. This includes:
How often do you have to have your eyes checked for glaucoma?
Part B will pay for you to have your eyes checked for glaucoma once every 12 months if you’re at increased risk of glaucoma. You’re considered high risk for glaucoma if you have:
What is the A1C test?
A hemoglobin A1c test is a lab test that measures how well your blood sugar has been controlled over the past 3 months. If you have diabetes, Part B covers this test if your doctor orders it.
What is diabetes self management training?
Diabetes self-management training helps you learn how to successfully manage your diabetes. Your doctor or other health care provider must prescribe this training for Part B to cover it.
Does Medicare cover diabetes?
This section provides information about Medicare drug coverage (Part D) for people with Medicare who have or are at risk for diabetes. To get Medicare drug coverage, you must join a Medicare drug plan. Medicare drug plans cover these diabetes drugs and supplies:
Does Part B cover insulin pumps?
Part B may cover insulin pumps worn outside the body (external), including the insulin used with the pump for some people with Part B who have diabetes and who meet certain conditions. Certain insulin pumps are considered durable medical equipment.
What is CMS in healthcare?
The Centers for Medicare & Medicaid Services (CMS) has developed a variety of educational resources for use by health care professionals and their staff as part of a broad outreach campaign to promote awareness and increase utilization of preventive services covered by Medicare. For more information about coverage, coding, billing, and reimbursement of Medicare-covered preventive services and screenings, visit
Does Medicare cover therapeutic shoes?
If a beneficiary has Medicare Part B, has diabetes, and meets certain conditions (see below), Medicare will cover therapeutic shoes if they need them. The types of shoes that are covered each year include one of the following:
Does Medicare pay for insulin pumps?
In the Original Medicare Plan, the beneficiary pays 20 percent of the Medicare-approved amount after the yearly Part B deductible. Medicare will pay 80 percent of the cost of the insulin pump. Medicare will also pay for the insulin that is used with the insulin pump.