
What are alternative payment models?
Types of APMs
- APMs. Meet the statutory definition of an APM. ...
- MIPS APMs. MIPS APMs have MIPS eligible clinicians participating in the APM on their CMS-approved participation list.
- Advanced APMs. ...
- Advanced & MIPS APMs. ...
- All-Payer/Other-Payer Option. ...
What is Medicare alternative payment model?
- Comprehensive ESRD Care Model (all tracks)
- Comprehensive Primary Care Plus Model (all tracks)
- Next Generation ACO Model
- Oncology Care Model (all tracks)
- Medicare Shared Savings Program (all tracks)
- Medicare ACO Track 1+ Model
- Bundled Payments for Care Improvement Advanced
- Maryland Total Cost of Care Model
- Vermont All-Payer ACO Model
How does Medicare calculate secondary payment?
How does Medicare calculate secondary payment? Medicare's secondary payment will be based on the full payment amount (before the reduction for failure to file a proper claim) unless the provider, physician, or other supplier demonstrates that the failure to file a proper claim is attributable to a physical or mental incapacity of the ...
What does Medicare pay as the secondary payer?
The Medicare secondary payment is $100. When Medicare is the secondary payer, the combined payment made by the primary payer and Medicare on behalf of the beneficiary is $3,000. The beneficiary has no liability for Medicare-covered services since the primary payment satisfied the $520 deductible.
What payment system is used by Medicare and Medicaid?
Prospective Payment Systems (PPS)Prospective Payment Systems (PPS) was established by the Centers for Medicare and Medicaid Services (CMS). PPS refers to a fixed healthcare payment system.
What is healthcare payment model?
Healthcare reimbursement models are billing systems by which healthcare organizations get paid for the services they provide to patients, whether by insurance payers or patients themselves.
What is Medicare alternative payment model?
An Alternative Payment Model (APM) is a payment approach that gives added incentive payments to provide high-quality and cost-efficient care. APMs can apply to a specific clinical condition, a care episode, or a population.
What are two types of payment models?
There are two basic types of bundled payment models: retrospective payment systems and prospective payment systems. In a retrospective payment system, payers retain a fee-for-service (FFS) arrangement and continue to compensate providers directly. But they also track total costs against the predetermined target price.
How many types of payment models are there in healthcare?
There are eight basic health care payment methods available in the world, these methods are more specific [11].
How does Medicare payment work?
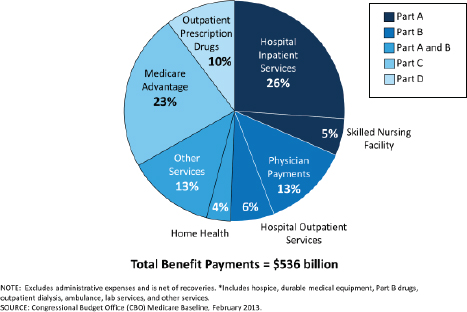
Medicare pays for 80 percent of your covered expenses. If you have original Medicare you are responsible for the remaining 20 percent by paying deductibles, copayments, and coinsurance. Some people buy supplementary insurance or Medigap through private insurance to help pay for some of the 20 percent.
Is Medicare Advantage an alternative payment model?
Advanced Alternative Payment Models Clinicians can qualify based on their participation in Medicare, Medicare Advantage (MA), Medicaid, and private sector models.
What is the difference between MIPS and APM?
MIPS stands for Merit-Based Incentive Payment System, while APM stands for Alternative Payment Model. Health care providers need to begin the verification process this year, and the first payments under these systems will be made in 2019. Both MIPS and APMs are processes that use value-based payment models.
What advanced payment models?
Advanced Alternative Payment Models (APMs) is a track of the Quality Payment Program that offers incentives for meeting participation thresholds based on your levels of payments or patients through Advanced APMs. If you achieve these thresholds, you become a qualifying APM participant (QP).
What is the best payment model in healthcare?
And fee-for-service is still the most widely used payment model, although its dominance is expected to wane over time. “Fee-for-service has been the dominant payment mechanism for decades,” says Bill Kramer, executive director for national health policy at the Pacific Business Group on Health.
What are the four modes of paying for health care?
In the U.S., there are four basic modes of paying for health care:Public health insurance programs, including Medicaid and Medicare.State employee health plans.Private health insurance plans (both individual and employer-provided group)Out-of-pocket costs for consumers.
What are the models of payment?
We consider how three broad payment models stack up against these criteria: fee-for-service (FFS), episode-based payment (EBP), and population-based payment (PBP).
What is the comorbidity payment for speech language pathology?
Currently, the diagnoses that trigger a speech-language pathology comorbidity payment within Section I800 of the MDS are limited to amyotrophic lateral sclerosis (ALS), oral and laryngeal cancers, and speech, language, and swallowing disorders due to CVA.
Is PT and OT reimbursement for comorbidities?
PT and OT are not reimbursed for comorbidities. Another key distinction is that PT and OT payments decrease as the episode goes on (known as a variable per diem payment) while speech-language pathology payment is consistent across the episode.
What is an APM in healthcare?
APMs require healthcare organizations (often a hospital and affiliated physician practices) to align themselves with the goal of taking better care of a population of patients, often defined by a geographic region. A common example of an APM is a Medicare Shared Savings Plan (MSSP) also known as an Accountable Care Organization (ACO).
What is the final rule for CMS 2021?
In the 2021 Final Rule, CMS announced 2021 would be the final year for web interface and APMs will need to begin participating in the APM Performance Pathway (APP). In addition, CMS announced reporting can happen at the APM entity, individual, and group/TIN level.
What is an advanced APM?
An Advanced APM is similar to an APM, with some additional criteria. The APM requires participants to use certified EHR technology. The APM bases payment on quality measures comparable to those in the MIPS quality performance category.
Do CMS APMs have unique reporting requirements?
Most CMS APMs have unique reporting requirements. APMs that are considered MIPS APMs may participate in MIPS at the APM entity level. In the past, many APMs have reported via the web interface mechanism, a sampling methodology for reporting on a specific set of attributed patients.
Zipcode to Carrier Locality File
This file is primarily intended to map Zip Codes to CMS carriers and localities. This file will also map Zip Codes to their State. In addition, this file contains an urban, rural or a low density (qualified) area Zip Code indicator.
Provider Center
For a one-stop resource web page focused on the informational needs and interests of Medicare Fee-for-Service (FFS) providers, including physicians, other practitioners and suppliers, go to the Provider Center (see under "Related Links" below).
Overview
In July 2018, CMS finalized a new case-mix classification model, the Patient Driven Payment Model (PDPM), that, effective beginning October 1, 2019, will be used under the Skilled Nursing Facility (SNF) Prospective Payment System (PPS) for classifying SNF patients in a covered Part A stay.
Fact Sheets
This section includes fact sheets on a variety of PDPM related topics.
PDPM Frequently Asked Questions
This section contains frequently asked questions (FAQs) related to PDPM policy and implementation.
PDPM Training Presentation
This section includes a training presentation which can be used to educate providers and other stakeholders on PDPM policy and implementation.
PDPM Resources
This section includes additional resources relevant to PDPM implementation, including various coding crosswalks and classification logic.
What is the payment model for healthcare?
There are several payment models in the United States federal healthcare system. The traditional method is Fee-for-Service (FFS), where providers are paid for each healthcare service they do, including tests. Another payment method is the capitation model, in which a contract is entered by a state, a health plan, and the CMS.
What is Medicare paid for?
In the traditional models, providers are paid by Medicare for each separate service given to a person during a course of treatment or a single illness. According to CMS, the traditional payment model can lead to less coordination between healthcare providers and healthcare settings.
What is BPCI in Medicare?
Share on Pinterest. BPCI can potentially improve patient care and lower Medicare healthcare costs. The Center for Medicare and Medicaid Innovation (CMMI), also known as the Innovation Center, works with the Centers for Medicare and Medicare Services (CMS) on developing and testing new ideas. One such idea involves innovative health care payment ...
How much did Medicare lower the cost of joint replacement?
In the first year Medicare lowered the cost of a joint replacement by an average $453. The CJR was a mandatory program for care providers. Many other bundled payment programs are voluntary for service providers. Data suggests it showed typical hospitals could improve care.
What is bundled payment?
Bundled payment is a potential new way to pay Medicare service providers. Medicare is testing the process to assess if it will improve care and reduce costs. In this article, we look at the Medicare bundled payments system, including the most recent models, and compare it to the traditional payment processes.
When did Medicare start testing BCPI?
Medicare started four tests of the BCPI in 2013. The first was done in 2016, with two more in 2018. The most recent report was released in June 2020. In 2018, the CMS reported that 1,547 Medicare providers and suppliers signed agreements to take part in the BCPI Advanced model.
What are the disadvantages of Medicare?
Disadvantages. Medicare found the fee-for-service payments were lower for clinical episodes during testing. However, overall spending increased due to rewards to the hospitals for reducing costs. Changing the bundles can be difficult in the computerized system.
What percentage of healthcare payments will be bundled by 2021?
While fee-for-service models are still the standard, the use of bundled payments is growing. In fact, McKesson and ORC International predicts that 17 percent of healthcare payments will be bundled payments by 2021. There’s some debate about which services should be bundled.
What is value based healthcare?
A value-based healthcare system is one where physicians and other healthcare providers are paid based on patient outcomes rather than on each service they provide. Value-based systems track the quality of care and reward providers for meeting goals and maintaining standards.
What is bundled payment?
Bundled payments are a type of medical billing encouraged by Medicare. These payments charge you for an entire procedure or hospital stay rather than each individual service you received. Bundled payments can lower your overall costs. Medicare provides incentives to providers who use bundled payments. The use of bundled payments is expected ...
What are bundled services?
Healthcare services that are commonly bundled include: hip replacement. knee replacement. labor and delivery. pacemaker insertion. treatment for congestive heart failure. treatment for heart attack.
Why is value based care important?
According to the Centers for Medicare and Medicaid Services (CMS), value-based care aims to achieve: better care for individuals. better health for populations.
When did the Affordable Care Act change?
For example, the Affordable Care Act of 2010 required bundled payments for hip and knee replacements and for cardiac care. This changed in November 2017, when the Trump administration and CMS canceled the mandate.
Does Medicare use bundled payments?
Medicare encourages the use of bundled payments as an APM and provides incentives for providers who use the bundled payment model. The use of bundled payments is expected to increase with time as part of an overall shift in U.S. healthcare models.
What is alternative payment model?
An Alternative Payment Model (APM) is a payment approach that gives added incentive payments to provide high-quality and cost-efficient care. APMs can apply to a specific clinical condition, a care episode, or a population.
What is an advanced APM?
An Advanced APM is a track of the Quality Payment Program that offers a 5 percent incentive for achieving threshold levels of payments or patients through Advanced APMs. If you achieve these thresholds, you are excluded from the MIPS reporting requirements and#N#payment adjustment#N#.
Speech-Language Pathology Case-Mix Factors
- Under the PDPM, payment for patients with speech-language pathology needs will be determined by the presence of the following five case-mix factors: 1. the patient's primary diagnosis, 2. the presence of one or more of twelve comorbidities (aphasia; CVA, TIA, or stroke; hemiplegia or hemiparesis; TBI; tracheostomy care while a resident; ventilator ...
Speech-Language Pathology Diagnosis Codes
- Diagnosis codes (International Classification of Diseases or ICD-10) have two distinct roles under PDPM. They are used to identify the primary diagnosis and secondary or treating diagnosis(es). Primary Diagnosis: SNFs assign an ICD-10 code to report the patient’s primary diagnosis, which is the reason for the SNF stay. The primary diagnosis is coded within Section I0200B and maps to a clinical category. Speech-language pathology related primary diag…
Payment For Speech-Language Pathology Services Is Unique
- It is also important to note that payment for speech-language pathology services is different from payment for occupational and physical therapy (OT and PT). For example, ASHA successfully advocated for the inclusion of comorbidities in the speech-language pathology portion of the SNF payment. PT and OT are not reimbursed for comorbidities. Another key distinction is that PT and OT payments decrease as the episode goes on (known as …
Practical Tips For Succeeding Under PDPM
- Although PDPM is meant to alleviate pressures to provide as much therapy as possible, it does not address industry-developed pressures such as productivity requirements. It also creates potential new challenges for SLPs. For example, the additional payment for patients on mechanically altered diets may create unintended payment incentives to place patients on mechanically altered diets unnecessarily or keep patients on them long…
Asha Resources
- Free ASHA Webinars and Podcast
This two-part series about PDPM dispels the myths surrounding the transition, discusses your role in patient care, and demonstrates the value of speech-language pathology in skilled nursing facilities. 1. Webinar Part 1: Know the Facts! (Video duration: 1 hr., 15 min.); view transcript[PDF] 2. Webinar Part 2: Know Your Value! (Video duration: … - ASHA Resources
1. Letter: ASHA, AOTA, APTA Joint Letters to Consumer Groups[PDF] (May 15, 2020) 2. PAC Consumer Fact Sheet: How Medicare Determines Payment for Your Therapy Services in Nursing Homes or Home Health Care[PDF] (May 15, 2020) 3. Presentation Recording: ASHA Discussions with SNF Leadership on the Impact of P…
Other Resources