
What are ConnectiCare Medicare Advantage plans?
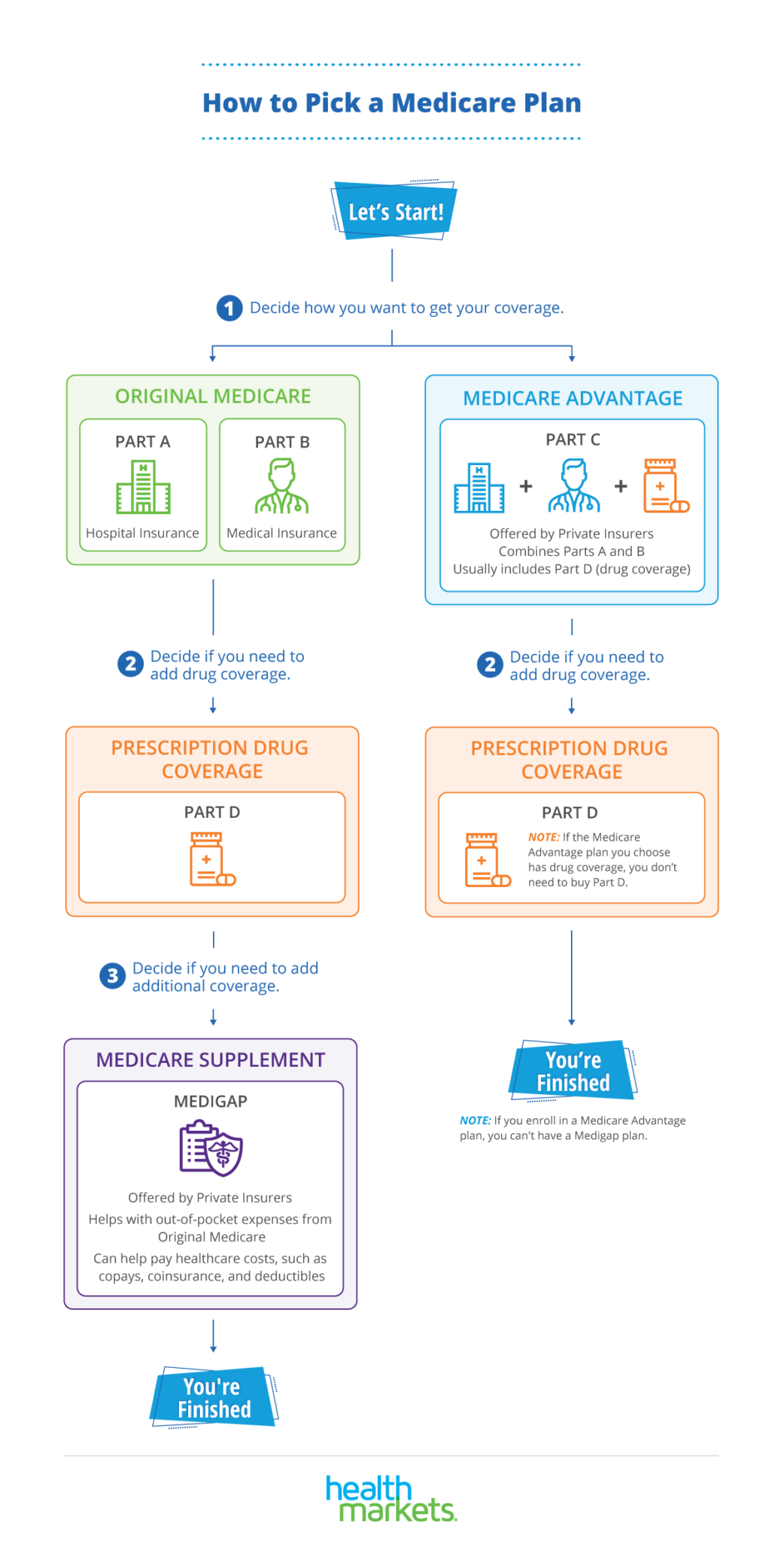
ConnectiCare Medicare Advantage plans include a number of Medicare Advantage Plans. These plans, sometimes called "Part C," provide all of a member's Part A (hospital coverage) and Part B (optional medical coverage) coverage and offer extra benefits too.
What is ConnectiCare Part C?
What is Part C? ConnectiCare is a managed care company that provides Medicare Advantage (Part C) plans throughout Connecticut. Every ConnectiCare Part C plan covers as least as much as original Medicare, plus some extras like prescription drug, dental, and vision coverage.
How does ConnectiCare work with patients choosing a PCP?
ConnectiCare will communicate to your patients how they may select a new PCP. ConnectiCare Medicare Advantage plans include a number of Medicare Advantage Plans. These plans, sometimes called "Part C," provide all of a member's Part A (hospital coverage) and Part B (medical coverage) and may offer extra benefits too.
What information will ConnectiCare provide to the Centers for Medicare&Medicaid?
• ConnectiCare will disclose to the Centers of Medicare & Medicaid Services (CMS) all information that is necessary to evaluate and administer our Medicare Advantage plans, and to establish and facilitate a process for current and prospective members to exercise choice in obtaining Medicare services.
Is ConnectiCare an Advantage plan?
ConnectiCare is a managed care company that provides Medicare Advantage (Part C) plans throughout Connecticut. Every ConnectiCare Part C plan covers as least as much as original Medicare, plus some extras like prescription drug, dental, and vision coverage.
What is ConnectiCare choice plan?
Our plan covers up to 90 days per inpatient mental health stay. Our plan also covers 60 “lifetime reserve days” as long as the stay is covered under the plan. Our plan covers up to 190 days in a lifetime for inpatient mental health services in a psychiatric hospital.
Is ConnectiCare part of Obamacare?
HARTFORD — ConnectiCare changed course Tuesday and will now remain part of the state's federally subsidized health insurance exchange next year.
Is ConnectiCare nationwide?
ConnectiCare has a nationwide network of pharmacies where new prescriptions can be filled using a member's ID card. For prescriptions obtained within the United States, the member can fill the prescription at any of 50,000 participating pharmacies and pay only the appropriate copayment.
Is ConnectiCare a Medicaid plan?
ConnectiCare Insurance Company, Inc. is an HMO D-SNP plan with a Medicare contract and a contract with the Connecticut Medicaid Program.
What is a qualified health plan Access Health CT?
Qualified Health Plan (QHP) An insurance plan that is certified by Access Health CT, provides Essential Health Benefits, follows established limits on cost -sharing (like deductibles, co-payments, and out-of-pocket maximum amounts), and meets other requirements.
What is Obamacare called in CT?
Access Health CTAccess Health CT is Connecticut's official health insurance marketplace, where you can shop, compare and enroll in quality healthcare plans; and it is the only place where you can qualify for financial help to lower your costs, and if eligible, enroll in free or low-cost coverage through HUSKY Health Program (Medicaid/ ...
Who owns ConnectiCare?
ConnectiCare Capital, LLCConnectiCare / Parent organization
What is the difference between POS and HMO?
As with an HMO, a Point of Service (POS) plan requires that you get a referral from your primary care physician (PCP) before seeing a specialist. But for slightly higher premiums than an HMO, this plan covers out-of-network doctors, though you'll pay more than for in-network doctors.
Can I use ConnectiCare in other states?
What happens if I am away from home and need prescription medication? Look for a participating pharmacy. Most pharmacy chains all over the USA participate with the ConnectiCare network. If you use a non-participating pharmacy, you are responsible for the full cost of the prescription at the time of purchase.
Is ConnectiCare part of EmblemHealth?
EmblemHealth's family of companies includes ConnectiCare, one of Connecticut's leading health plans; AdvantageCare Physicians, a primary and specialty care practice; and WellSpark, a digital wellness company.
Is Husky a ConnectiCare?
Access Health CT offers a range of Qualified Health Plan (QHP) options from private health insurance providers [e.g. Anthem, ConnectiCare Benefits (individual plans only), UnitedHealthcare, Healthy CT and affordability programs through the Department of Social Services (i.e. Medicaid (HUSKY A and D)), Children's Health ...
What Makes ConnectiCare Plans Stand Out?
Our plans are designed with you in mind. Find the quality, personalized health care you deserve at a reasonable price. NOTE: Open enrollment for 2021 plans has ended. But in some cases, you can enroll in an individual health plan if you qualify for a Special Enrollment Period. Learn more on our enroll page.
Looking for Group Plans?
Are you an employer looking for affordable health care? ConnectiCare offers quality coverage for small and large groups to keep your employees healthy.
Start Shopping
Browse our affordable, comprehensive health care plans for individuals under 65 and their families.
What is ConnectiCare in Connecticut?
ConnectiCare is a managed care company and subsidiary of New York–based healthcare insurer, EmblemHealth. It offers Medicare Advantage (Part C) plans to people who live in Connecticut. The ConnectiCare network of providers, including general practitioners and specialists, can be found throughout the entire state of Connecticut ...
What is ConnectiCare Flex?
Like all HMOs that include a Point-of-Service (POS) option, ConnectiCare Flex plans give you the ability to use out-of-network providers throughout the United States. There are three Flex plan levels, indicated by numbers 1, 2, and 3. All three plans are available in all eight Connecticut counties.
What is a Part C plan?
What is Part C? Takeaway. at a glance. ConnectiCare is a managed care company that provides Medicare Advantage (Part C) plans throughout Connecticut. Every ConnectiCare Part C plan covers as least as much as original Medicare, plus some extras like prescription drug, dental, and vision coverage.
Does ConnectiCare offer Medicare Part D?
As discussed above, certain ConnectiCare Advantage plans include Medicare Part D prescription drug coverage. ConnectiCare doesn’t sell any stand-alone Part D plans. You must use ConnectiCare in-network pharmacies to get the most coverage for your prescription medications. Like all Medicare plans that provide prescription drug coverage, ...
Do you have to enroll in Medicare to get a Part C?
To buy a Part C plan, you must first enroll in original Medicare. By law, Part C plans are required to cover at least as much as original Medicare. Many Part C plans, including some ConnectiCare plans, also cover extras that original Medicare doesn’t. These extras may include:
Does ConnectiCare cover prescriptions?
ConnectiCare’s plans vary in terms of copays, deductibles, and covered services. Some, but not all, ConnectiCare Part C plans include prescription drug coverage.
Who is ConnectiCare underwritten by?
ConnectiCare Medicare Supplement insurance plans are underwritten by ConnectiCare Insurance Company, Inc. (ConnectiCare), an EmblemHealth Company. Coverage is subject to all terms, conditions, limitations and exclusions set forth in the applicable ConnectiCare Medicare Supplement policy.
How much is ConnectiCare deductible in 2021?
This is a high deductible plan that pays the same benefits as Plan G after you have paid the calendar year deductible of $2,370 in 2021. This means ConnectiCare will not begin to pay until your covered out-of-pocket expenses exceed $2,370 in 2021.
What is Plan G for 2021?
Plan G also provides coverage for the Part A deductible ($1,484 in 2021), skilled nursing facility coinsurance, foreign emergency care, and 100% coverage of excess charges above what Medicare will pay on Part B .
What is the Medicare Supplement phone number?
Please refer to the Medicare Supplement policy for the full terms and conditions of coverage or call 877-224-5995 (TTY: 711) for more information.
Does ConnectiCare pay for Medicare?
ConnectiCare pays Part A and Part coinsurance (20 percent of Medicare-approved expenses), Medicare pays 80 percent. Please note: You can only enroll in this plan if you were eligible for Medicare before January 1, 2020.
Does ConnectiCare pay for hospitalizations?
Plan B also provides coverage for the Part A deductible ($1,484 in 2021). This is the amount you pay before Medicare begins to pay for hospitalizations.
Is ConnectiCare endorsed by the government?
The Medicare Supplement insurance plans, ConnectiCare and agents/producers are not connected with or endorsed by the U.S. Government or the federal Medicare program. The purpose of this communication is the solicitation of insurance. Premium and benefits vary by Medicare Supplement plan selected. Contact may be made by an insurance agent ...
How many people are in Medicare Advantage?
Amounts vary by plan. It’s easy to see why more than 24 million people nationwide are enrolled in Medicare Advantage plans.1.
What is Medicare for ALS?
What is Medicare? Medicare is a federal health insurance program that provides health coverage for individuals age 65 and older. It also covers certain people under age 65 with disabilities and those with End-Stage Renal Disease (ESRD) and Amyotrophic Lateral Sclerosis (ALS, also known as Lou Gehrig's disease).
How long do you have to wait to get Medicare if you are 65?
You may also be new to Medicare due to disability. Typically, there is a 24-mont h waiting period before you qualify for Medicare Part B.
What happens if you don't enroll in Medicare?
Turning 65? If you’re turning 65 or are over 65 and new to Medicare, it’s time to start exploring your Medicare options. Medicare has guidelines and time frames for enrollment. If you don’t enroll when you are first eligible, there could be late enrollment penalties. To avoid these penalties, it’s wise to contact us or Medicare 4 to 6 months ...
Is MA covered by Medicare?
MA plans are run by private companies that are approved by Medicare, like ConnectiCare. They include all of your Part A and Part B coverage, plus extra benefits and services like routine care, dental services, and wellness programs. Medicare Part D is prescription drug coverage. Medicare Part D is not offered by Medicare itself.
Does Medicare have a monthly premium?
May offer additional benefits beyond Original Medicare, like routine care, fitness and dental. Have one monthly plan premium or, in some cases, no monthly plan premium (in addition to your Part B premium). Convenience – all your medical and prescription drug benefits offered through a single health plan.
Does Medicare pay 80% of your deductible?
After you meet your Part A deductible and your Part B deductible, generally Medicare pays 80% of covered costs and you pay 20%. You must continue to pay your Part B monthly premium. Offered by private companies, like ConnectiCare. Include both Medicare Part A and Part B coverage.
Enrolling in a Medicare Supplement Plan
Medicare Supplement Insurance is open for enrollment all year long. We’ve made enrolling as easy as possible. See below for eligibility and enrollment information.
Plan Description
Medicare Supplement plans, also referred to as Medigap plans, help pay for some of the health care costs not covered by Original Medicare - Part A hospital insurance and Part B medical insurance.
Eligibility and Enrollment
To apply for coverage under one of ConnectiCare’s Medicare Supplement plans, you must:
You Have Options
At ConnectiCare, we offer a wide range of Medicare Supplement insurance plans. You choose the plan with the benefit design that best suits your needs.
When is the annual election for Medicare 2021?
Annual Election Period for 2021 Coverage: October 15, 2020 – December 7, 2020. If you are eligible for Medicare, you can enroll in or switch plans during the Annual Election Period. For example, you can switch from Original Medicare to a Medicare Advantage plan (like a ConnectiCare Medicare Advantage Plan). Your coverage will be effective on ...
How long do you have to enroll in Medicare?
You will have a three-month period to enroll, which begins three months before your Medicare Part B effective date. You will not be able to enroll after your Medicare Part B effective date. If you receive Medicare benefits due to a disability, you can join from three months before to three months after your 25th month of disability.
What is an OEP in Medicare?
The OEP allows individuals enrolled in a Medicare Advantage plan, including newly Medicare Advantage-eligible individuals, to make a one-time election to go to another Medicare Advantage plan or Original Medicare. Individuals using the OEP to make a change may make a coordinating change to add or drop Part D coverage.
How to contact Medicare for late enrollment?
For more information on the Medicare Part B late enrollment penalty and/or Medicare Enrollment Periods, you can contact Medicare directly by calling 1-800-MEDICARE ( 1-800-633-4227 ), TTY: 1-877-486-2048 (24 hours a day/7 days a week) or visit the official website at www.medicare.gov.
What happens if you don't sign up for Medicare?
If you don't sign up for Medicare Part B (Medical Insurance) during your Initial Election Coverage Period*, a 10% penalty may be added to the Part B premium for each 12-month period you could have had Part B but didn’t take it, unless you qualify for the Part B Special Enrollment Period.
Is ConnectiCare part A or B?
You qualify for Medicare Part A; You are enrolled in and continue to pay Medicare Part B; and. You reside in ConnectiCare's service area (entire state of Connecticut). To join and remain eligible for a ConnectiCare Choice Dual (HMO D-SNP) plan, you must be: Entitled to Medicare Part A,
Does ConnectiCare cover urgent care?
Yes. It's important to know that your health plan will be there for you if you have a medical emergency or urgent care situation, especially when you travel. All our plans include coverage for emergency and urgent care. With ConnectiCare HMO and HMO-POS plans, you are covered for these services worldwide. 1.
What is ConnectiCare insurance?
ConnectiCare is a managed care company and subsidiary of New York–based healthcare insurer, EmblemHealth. It offers Medicare Advantage (Part C) and Medicare supplement (Medigap) plans to people who live in Connecticut.
What are the benefits of ConnectiCare?
ConnectiCare Medicare Supplement Plan A 1 Medicare Part A coinsurance and hospital coverage up to 365 days after Medicare benefits are used up 2 Part A hospice care coinsurance or copayment 3 Medicare Part B coinsurance or copayment 4 first three pints of blood needed
What is Medicare Supplement Plan?
Medicare supplement plans, or Medigap plans, are optional products offered to people with original Medicare (parts A and B) to help pay for certain out-of-pocket costs. These plans can be used to pay copayments or other items not covered by standard Part A and Part B coverage.
What is Medicare Part A coinsurance?
Medicare Part A hospital coinsurance. all or some of Part A hospice coinsurance or copayments. all or a portion of Medicare Part B coinsurance and copayments. all or some of the cost of up to three pints of blood.
How long does Medicare Part A cover?
Medicare Part A coinsurance and hospital coverage up to 365 days after Medicare benefits are used up. ConnectiCare also offers high-deductible versions of plans F and G. With these plans, 100 percent of covered services are paid after you meet a $2,370 deductible for the year.
What is Medicare Part A and B?
Original Medicare is made up of parts A and B together. There are several choices when it comes to Medicare supplement plans, and each insurer may offer different options. For the 2021 plan year, all Medicare supplement plans from ConnectiCare cover: Medicare Part A hospital coinsurance.
How long does Medicare cover hospital coinsurance?
Medicare Part A coinsurance and hospital coverage up to 365 days after Medicare benefits are used up. Part A hospice care coinsurance or copayment. Medicare Part A deductible. Medicare Part B coinsurance or copayment. first three pints of blood needed.
What is the ConnectiCare eligibility and referral line?
This system requires that you have a touch-tone phone and know your ConnectiCare provider ID number, as well as the member's identification number, to verify eligibility.
What is the PPM number for Connecticare?
If you want a paper copy of this information, you may contact Provider Services at 1-860-674-5850 or 1-800-828-3407. PPM/10.16.
What is a Point of Service High Deductible Health Plan?
Point-of-Service High Deductible Health Plans have an additional Plan deductible requirement for services rendered by non-participating providers. Deductible plans. Members have an in-network deductible for some covered services before coverage for the benefits will apply.
How far in advance do you have to notify ConnectiCare?
If you are relocating out of ConnectiCare's network or retiring, please notify your patients at least ten (10) days in advance, in writing, in addition to notifying ConnectiCare and, if applicable, your contracted PHO/IPA in writing sixty (60) days in advance. ConnectiCare will also notify members of the change thirty (30) days prior to the effective date of the change, or as soon as possible after we become aware of the change.
What is a Part C plan?
These plans, sometimes called "Part C," provide all of a member's Part A (hospital coverage) and Part B (optional medical coverage) coverage and offer extra benefits too. These extra benefits include, but are not limited to, vision, dental, hearing, and preventive services, like annual physicals.
Does ConnectiCare offer Medicare Advantage?
ConnectiCare will communicate to your patients how they may select a new PCP. ConnectiCare Medicare Advantage plans include a number of Medicare Advantage Plans. These plans, sometimes called "Part C," provide all of a member's Part A (hospital coverage) and Part B (medical coverage) and may offer extra benefits too.
Can ConnectiCare terminate a copayment?
ConnectiCare reserves the right to terminate coverage for members who repeatedly fail to make the required copayments, coinsurance or deductibles, subject to the terms outlined in the applicable Member Agreement, Evidence of Coverage, or other governing contract.

Connecticare and EmblemHealth Reciprocity For Network Access
Connecticare to Offer A New Medicare Plan in 2022
- ConnectiCare Choice Dual Vista (HMO D-SNP) is a special needs plan for members with full Medicaid and Medicare that offers over-the-counter benefits, dental, vision, fitness, and hearing benefits in addition to Medicare-covered Part A and Part B services. Providers will need to coordinate the payment for covered services with the Connecticut Medica...
Value-Based Insurance Design and New Benefits
- The EmblemHealth family of companies is pleased to announce our participation in the CMS-approved Value-Based Insurance Design (VBID) Model. This program is designed to promote wellness and advance care planning to help ensure our Medicare members receive medical care that is consistent with their values, goals, and preferences. Plans participating in VBID include th…