Full Answer
What screening labs are covered by Medicare?
Types of labs covered by Medicare include: doctors’ offices; hospital labs; independent labs; nursing facility labs; other institution labs
Are labs covered by Medicare?
When ordered by a physician, lab work is generally covered by Medicare Part B. Part B (Medical Insurance) helps cover medically necessary services and care in an outpatient setting, such as a doctor’s office.
Are lab tests covered under Welcome to Medicare?
clinical diagnostic laboratory services when your doctor or practitioner orders them. You usually pay nothing for Medicare-approved clinical diagnostic laboratory services. Laboratory tests include certain blood tests, urinalysis, tests on tissue specimens, and some screening tests. A laboratory that meets Medicare requirements must provide them.
Does Quest labs take Medicaid?
To get started, click on the state below where your Quest testing is performed: There are Local Coverage Determinations (LCDs) issued by the Medicare Administrative Contractors (MACs) and National Coverage Determinations (NCDs) issued by the Centers for Medicare & Medicaid Services (CMS).

What Labs can I use with Medicare?
Medicare will pay for clinical diagnostic lab tests that your doctor orders if they are medically necessary. Typically, you will not have to pay anything for the tests. Lab tests could include urinalysis, blood tests, tests on tissue specimens and screening tests.
Is Medicare a labcorp or quest?
Medicare covers tests performed at Quest, as long they're medically necessary and the specific facility accepts Medicare. Medicare Part B or Medicare Advantage (Part C) will cover the cost of your tests.
Does Medicare cover routine blood work?
The blood test must be deemed medically necessary in order to be covered by Medicare. Original Medicare (Medicare Part A and Part B) does not cover routine blood work as part of a general physical examination or screening.
Does labcorp take Medicare insurance?
Labcorp Coverage Labcorp will bill Medicare. Medicare will determine coverage and payment. The Labcorp LabAccess Partnership program (LAP) offers a menu of routine tests at discounted prices.
Does Medicare Part B cover lab tests?
Part B covers certain doctors' services, outpatient care, medical supplies, and preventive services. covers medically necessary clinical diagnostic laboratory tests, when your doctor or provider orders them. You usually pay nothing for Medicare-covered clinical diagnostic laboratory tests.
How often will Medicare pay for labs?
every 5 yearsBoth Original Medicare and Medicare Advantage cover a cholesterol screening test every 5 years.
Does Medicare pay for blood work every 6 months?
Medicare Part B also covers 80 percent of the Medicare-approved cost of preventive services you receive from your doctor or other medical provider. This includes wellness appointments, such as an annual or 6-month checkup.
Does Medicare pay for lipid panel blood test?
Medicare covers cholesterol testing as part of the covered cardiovascular screening blood tests. Medicare also includes tests for lipid and triglyceride levels. These tests are covered once every 5 years.
Does Medicare cover vitamin B12 blood test?
The Centers for Medicare & Medicaid Services also do not provide coverage for routine testing for vitamin B12 deficiency. There is agreement within the literature that serum vitamin B12 testing should be used to diagnose vitamin B12 deficiency in symptomatic and high-risk populations.
Is Quest Diagnostics or LabCorp better?
Labcorp is most highly rated for Compensation and benefits and Quest Diagnostics is most highly rated for Compensation and benefits....Overall Rating.Overall Rating3.43.6Management2.93.1Culture3.23.43 more rows
Is LabCorp and Quest Diagnostics the same company?
LabCorp is the parent company of Quest Diagnostics and offers core laboratory services such as clinical chemistry, immunology, infectious disease, and molecular testing. On the other hand, Quest Diagnostics offers many services much in the same way.
Does quest take medical?
Coverage for Quest services is not universal, however. In several states, Quest provides covered diagnostic services as part of a limited package that has been approved by Medicaid. In California, for example, Medicaid does pay for Quest services that fall within an approved package, such as prenatal services, H.
Does Quest Diagnostics accept Aetna Medicare?
Quest Diagnostics®* is our national preferred lab provider for Aetna members. Their labs offer many advantages.
How do I call Medicare?
(800) 633-4227Centers for Medicare & Medicaid Services / Customer service
How does Medicare determine medical necessity?
Insurance companies provide coverage for care, items and services that they deem to be “medically necessary.” Medicare defines medical necessity as “health-care services or supplies needed to diagnose or treat an illness or injury, condition, disease, or its symptoms and that meet accepted standards of medicine.”
Does quest take medical?
Coverage for Quest services is not universal, however. In several states, Quest provides covered diagnostic services as part of a limited package that has been approved by Medicaid. In California, for example, Medicaid does pay for Quest services that fall within an approved package, such as prenatal services, H.
What are laboratory tests?
Laboratory tests include certain blood tests, urinalysis, tests on tissue specimens, and some screening tests.
What is part B in medical?
Clinical laboratory tests. Part B covers certain doctors' services, outpatient care, medical supplies, and preventive services. Health care services or supplies needed to diagnose or treat an illness, injury, condition, disease, or its symptoms and that meet accepted standards of medicine.
What does Medicare Part B cover?
Part B also covers durable medical equipment, home health care, and some preventive services.
Is my test, item, or service covered?
Find out if your test, item or service is covered. Medicare coverage for many tests, items, and services depends on where you live. This list includes tests, items, and services (covered and non-covered) if coverage is the same no matter where you live.
How Often Does Medicare Pay for Blood Work?
Medicare pays for medically necessary blood work a doctor orders, as well as screening laboratory testing. Medicare may limit how often you can have these tests and the amount they pay. Examples include:
Does Medicare Part B Cover Lab Tests?
Medicare Part B will cover medically necessary laboratory tests, provided your doctor orders the test, and a Medicare-approved lab runs the test. Part B is the Medicare portion that covers medical services, including doctor’s visits.
Does Medicare Cover LabCorp or Quest?
Medicare covers medically necessary lab tests from LabCorp and Quest. These are two large laboratories that provide outpatient laboratory testing.
What Types of Lab Work Are Covered by Medicare?
Medicare covers a wide range of lab work, including blood tests to check cholesterol levels and liver function, or urinalysis to screen for infection or diabetes. Medicare will also cover diagnostic testing, such as X-rays and CT scans, when medically necessary.
Your Deductibles
For Part A, you will have a deductible per each benefit period of $1,484 as of 2021. This benefit period starts when you are admitted as an inpatient. You won’t have to pay coinsurance for days 1 through 60, but if your inpatient stay is longer than that, you should expect to pay a coinsurance.
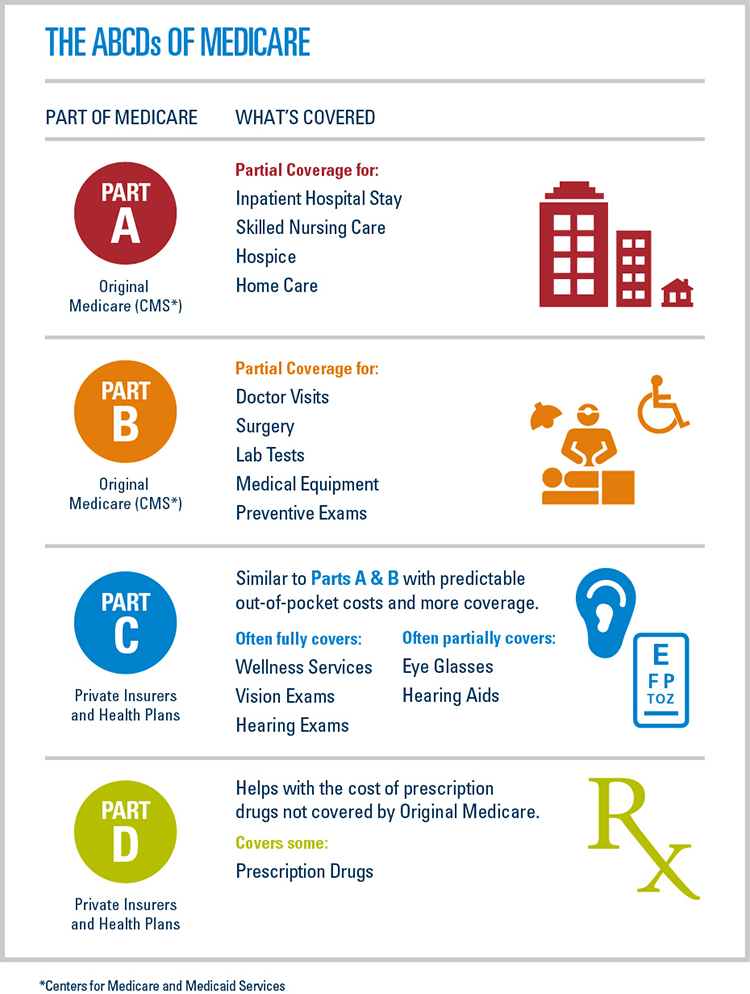
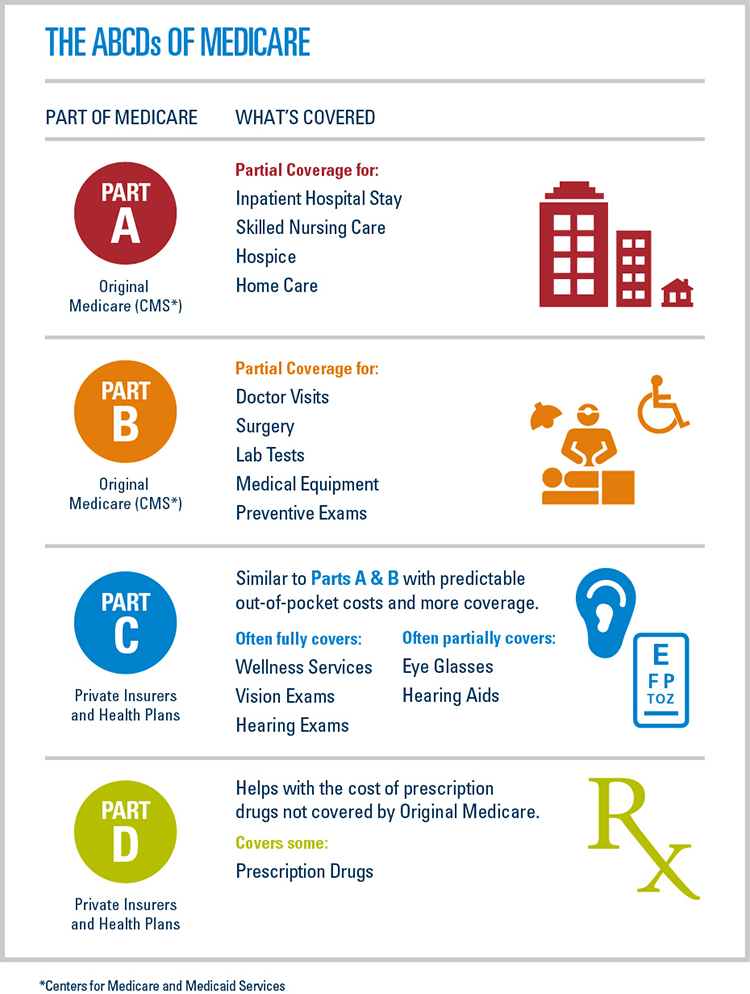
Parts A and B
Now that you know what costs you can expect, let’s further discuss the coverage of these two parts. Medicare Part A covers inpatient care in a hospital or a skilled nursing facility. It also provides coverage for hospice care, some home health services, and typically includes room and board as well as general nursing services.
Give Turning 65 Solutions A Call Today!
With all of the changes that go into effect over time, you need someone who understands what’s covered and how this impacts you and your out-of-pocket costs. That’s why we are the experts when it comes to understanding Medicare coverage. Give us a call today if you want help navigating through these waters!
How often does Medicare cover mammograms?
once a year if you meet criteria. *Medicare covers diagnostic mammograms more often if your doctor orders them. You are responsible for the 20 percent coinsurance cost. Other nonlaboratory diagnostic screenings Medicare covers include X-rays, PET scans, MRI, EKG, and CT scans.
What is Medicare Part A?
Medicare Part A offers coverage for medically necessary blood tests. Tests can be ordered by a physician for inpatient hospital, skilled nursing, hospice, home health, and other related covered services. Medicare Part B covers outpatient blood tests ordered by a physician with a medically necessary diagnosis based on Medicare coverage guidelines.
What is the purpose of blood test?
Blood tests are an important diagnostic tool doctors use to screen for risk factors and monitor health conditions. A blood test is generally a simple procedure to measure how your body is functioning and find any early warning signs. Medicare covers many types of blood tests. Trusted Source.
How much is Medicare Part B 2021?
You have to meet your annual deductible for this coverage as well. In 2021, the deductible is $203 for most people. Remember, you also have to pay your monthly Part B premium, which is $148.50 in 2021 for most beneficiaries.
How much does a blood test cost?
The costs are based on the particular test, your location, and the lab used. Tests can run from a few dollars to thousands of dollars. That’s why it’s important to check that your test is covered before you have it done.
Does Medigap cover out of pocket costs?
Medigap (Medicare supplemental insurance) plans can help pay for some out-of-pocket costs like coinsurance, deductibles, or copayments of covered screenings and other diagnostic tests.
Does Medicare cover 20 percent coinsurance?
You have to pay your 20 percent coinsurance as well as your deductible and any copays. Remember to go to providers that accept assignment to avoid charges Medicare won’t cover. Helpful links and tools. Medicare offers a tool you can use to check which tests are covered.
Why is blood testing important?
Blood tests play a crucial role in the diagnosis, monitoring and treatment of a large number of diseases. Many patients and doctors rely on blood test results to create a holistic treatment plan geared toward overall wellness, but blood tests can also be vital when determining whether a current treatment is effective or not.
Does Medicare cover lab testing?
It’s important to make this distinction because Medicare benefits often aren’t available for lab testing that a patient has sought out on his or her own. Medicare Part A (Hospital Insurance) may also provide coverage for blood testing when such tests are administered in a hospital or skilled nursing facility setting.
Does Medicare cover blood work?
Aside from simple and routine blood testing, Medicare benefits also offer coverage for a range of associated diagnostic tests, including urinalysis, tissue testing and screenings for certain diseases when a medical order has been provided.
Is blood testing covered by Medicare?
In the vast majority of cases, blood testing is covered by Medicare Part B. Part B (Medical Insurance) provides benefits for medically necessary care administered in a physician’s office or in an outpatient clinical setting.
Can Medicare provide blood tests?
It’s worth noting that some blood tests can provide improper readings due to medications, so always clarify with your physician what medications to take and which to avoid prior to having your blood drawn. Medicare Provides For More Than Just Blood Testing.
Can you get diagnostic tests with Medicare?
This essentially means that Medicare recipients are able to receive diagnostic services for almost any illness with a doctor ’s orders as long as the testing is medically necessary and carried out at a Medicare-ap proved facility.