Medicare covers part-time or intermittent in-home skilled nursing care at a patient’s residence. These services are provided less than seven days a week or less than 8 per day across a 21 day span. If the patient is at a skilled nursing facility, the services will be covered by Part A and B Medicare.
What does Medicare cover for in-home care?
Medicare will cover the cost of medically necessary equipment prescribed by a doctor for in-home use. This includes items such as canes or walkers, wheelchairs, blood sugar monitors, nebulizers, oxygen, and hospital beds.
How much does Medicare pay for home health care?
Your costs in Original Medicare $0 for home health care services. 20% of the Medicare-approved amount for Durable Medical Equipment (DME). Before you start getting your home health care, the home health agency should tell you how much Medicare will pay.
Does Medicare cover 24-hour in-home care?
Medicare doesn’t cover 24-hour in-home care. If you need this level of care, your doctor may recommend that you or a loved one enter a skilled nursing home facility, which is covered by Medicare. You will only qualify for in-home care if part-time or intermittent skilled nursing care is needed, as mentioned before.
Does Medicare Part C cover in-home care?
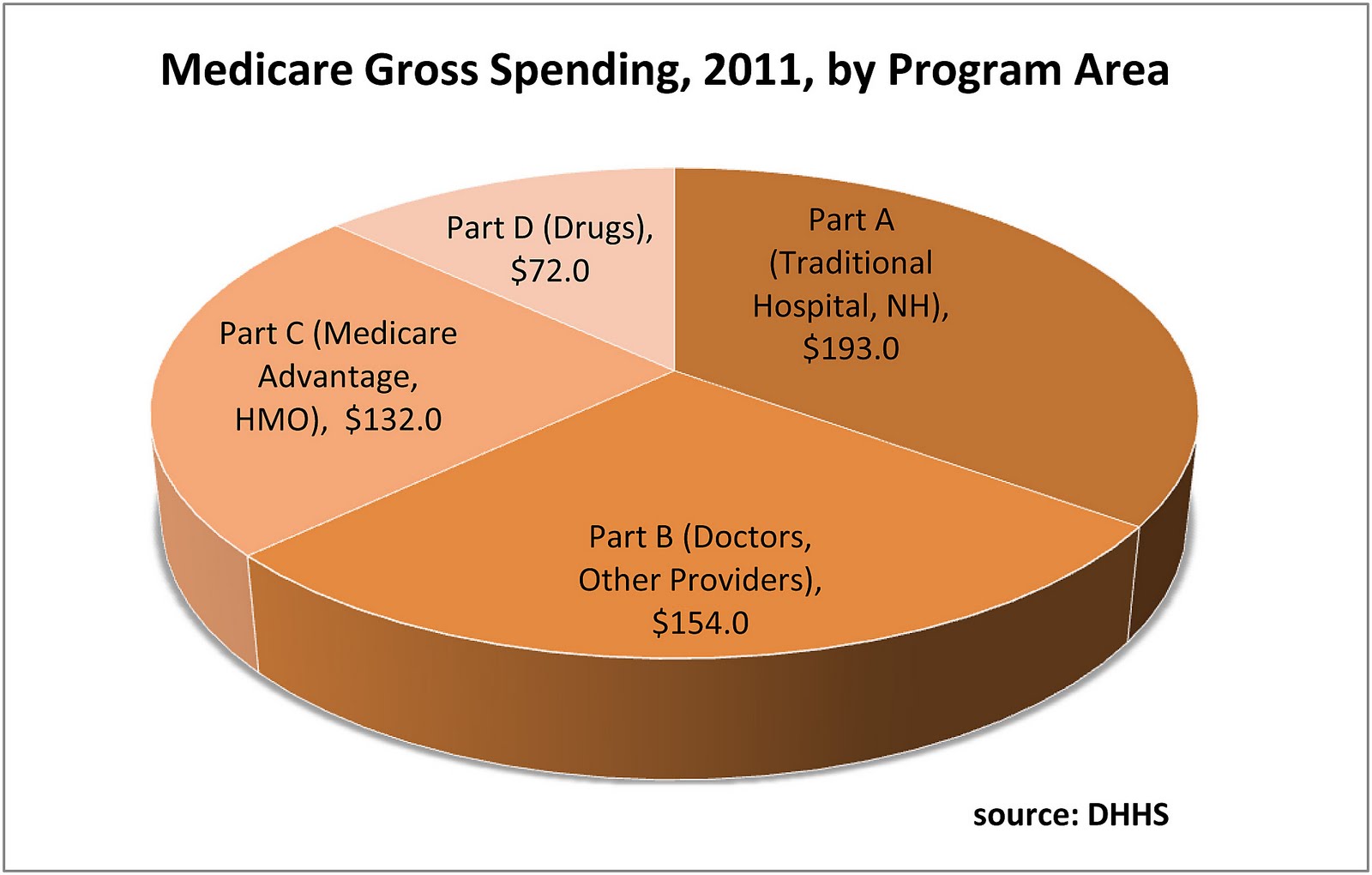
Medicare Advantage plans are an alternative to traditional Medicare (Medicare Part A and Part B), both of which don’t cover non-skilled in-home health care. Not all Medicare Part C plans have the same coverage and benefits.
Will Medicare cover skilled nursing care?
Medicare will pay for what’s considered intermittent nursing services, meaning that care is provided either fewer than seven days a week, or daily...
Will Medicare cover physical, occupational, and speech therapy?
Medicare will pay for physical therapy when it’s required to help patients regain movement or strength following an injury or illness. Similarly, i...
Does Medicare cover durable medical equipment?
Medicare will cover the cost of medically necessary equipment prescribed by a doctor for in-home use. This includes items such as canes or walkers,...
Does Medicare cover medical social services?
Medicare will pay for medically prescribed services that allow patients to cope with the emotional aftermath of an injury or illness. These may inc...
Who’s eligible for in-home care through Medicare?
Medicare enrollees are eligible for in-home care under Medicare Parts A and B provided the following conditions are met: The patient is under the c...
Will Medicaid pay for long-term care services?
Many Medicare enrollees are qualify for Medicaid due to their limited incomes and assets. Unlike Medicare, Medicaid covers both nursing home care a...
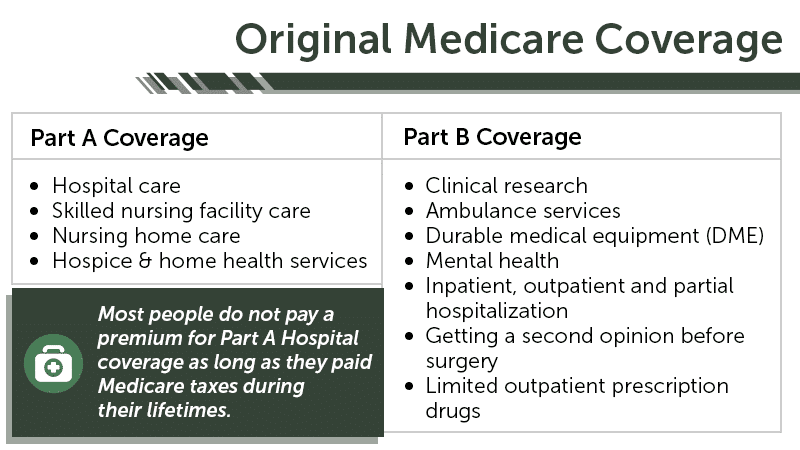
What is Medicare Part A?
Medicare Part A (Hospital Insurance) and/or Part B (Medical Insurance) will help cover the costs of in-home health services if you are being treated by a doctor who creates a plan of care and reviews it regularly.
What is DME in home care?
Medical supplies for use in the home, such as durable medical equipment (DME) In-home care should be ordered by your physician to help you recover from an illness or injury, regain your independence and self-sufficiency, maintain or improve your condition, and/or slow any progressive decline.
How many hours of skilled nursing per week?
Your doctor must certify that you require one of these services: Intermittent skilled nursing care, defined by Medicare as less than 7 days per week or less than 8 hours each day over a period of 21 days or less. Physical therapy, speech language pathology, or occupational therapy.
What does it mean to be comfortable in your own home?
The comforts of home can mean different things to different people. It may include sleeping in your own bed, curling up in your favorite chair, or enjoying a view of your garden from the kitchen window. When you are recovering from an illness or injury, your own home may provide the best environment to help you heal.
What is the wide range of services?
The wide range of services can include: Coordination of care with your medical providers. In-home care should be ordered by your physician to help you recover from an illness or injury, regain your independence and self-sufficiency, maintain or improve your condition, and/or slow any progressive decline.
Is home health care the best?
Home health care may be the best solution to your needs. Home health services can be just as effective as treatment you would receive in a hospital or skilled nursing facility and may be less expensive. The wide range of services can include: Coordination of care with your medical providers. Monitoring serious illness.
Is home health insurance covered by Medicare?
When you are recovering from an illness or injury, your own home may provide the best environment to help you heal. If your doctor recommends it and you meet the criteria, your in-home health services may be covered by your Medicare insurance. Home health care may be the best solution to your needs.
Who is covered by Part A and Part B?
All people with Part A and/or Part B who meet all of these conditions are covered: You must be under the care of a doctor , and you must be getting services under a plan of care created and reviewed regularly by a doctor.
What is an ABN for home health?
The home health agency should give you a notice called the Advance Beneficiary Notice" (ABN) before giving you services and supplies that Medicare doesn't cover. Note. If you get services from a home health agency in Florida, Illinois, Massachusetts, Michigan, or Texas, you may be affected by a Medicare demonstration program. ...
What is a medical social service?
Medical social services. Part-time or intermittent home health aide services (personal hands-on care) Injectible osteoporosis drugs for women. Usually, a home health care agency coordinates the services your doctor orders for you. Medicare doesn't pay for: 24-hour-a-day care at home. Meals delivered to your home.
What is intermittent skilled nursing?
Intermittent skilled nursing care (other than drawing blood) Physical therapy, speech-language pathology, or continued occupational therapy services. These services are covered only when the services are specific, safe and an effective treatment for your condition.
What is the eligibility for a maintenance therapist?
To be eligible, either: 1) your condition must be expected to improve in a reasonable and generally predictable period of time, or 2) you need a skilled therapist to safely and effectively make a maintenance program for your condition , or 3) you need a skilled therapist to safely and effectively do maintenance therapy for your condition. ...
Does Medicare cover home health services?
Your Medicare home health services benefits aren't changing and your access to home health services shouldn’t be delayed by the pre-claim review process.
Do you have to be homebound to get home health insurance?
You must be homebound, and a doctor must certify that you're homebound. You're not eligible for the home health benefit if you need more than part-time or "intermittent" skilled nursing care. You may leave home for medical treatment or short, infrequent absences for non-medical reasons, like attending religious services.
What Is In-Home Care?
In-home care (also known as “home health care”) is a service covered by Medicare that allows skilled workers and therapists to enter your home and provide the services necessary to help you get better.
What Parts Of In-Home Care Are Covered?
In-home care can cover a wide range of services, but they’re not all covered by Medicare. According to the Medicare site, the in-home care services covered by parts A and B include:
How To Get Approved For In-Home Care
There are a handful of steps and qualifications you need to meet to have your in-home care covered by Medicare. It starts with the type of help your doctor says you or your loved one needs and includes other aspects of care.
Cashing In On In-Home Care
Once you qualify for in-home care, it’s time to find the right agency who will provide you or your loved one services. The company you receive your services from is up to you, but they must be approved by Medicare in order for their services to be covered.
How To Pay for In-Home Care Not Covered By Medicare
There may be times when not every part of your in-home care is covered. We already know 20 percent of the durable medical equipment needed to treat you is your responsibility, but there are other services like custodial care or extra round-the-clock care that won’t be covered by Medicare. This is where supplemental insurance (Medigap) comes in.
How long does Medicare pay for custodial care?
Medicare will sometimes pay for short-term custodial care (100 days or less) if it’s needed in conjunction with actual in-home medical care prescribed by a doctor.
How many hours does Medicare pay for a week?
The maximum amount of weekly care Medicare will pay for is usually 28 hours, though in some circumstances, it will pay for up to 35. But it won’t cover 24-hour-a-day care.
What is a long term care policy?
A long-term care policy can help defray the cost of home health aides whose services are strictly custodial in nature. It can also help pay for assisted living facilities, which offer seniors the ability to live independently, albeit with help.
How long does Medicare pay for intermittent nursing?
Medicare will pay for what’s considered intermittent nursing services, meaning that care is provided either fewer than seven days a week, or daily for less than eight hours a day, for up to 21 days. Sometimes, Medicare will extend this window if a doctor can provide a precise estimate on when that care will end.
What is skilled nursing?
Skilled nursing services are generally required to treat an illness or assist in the recovery of an injury. As the name implies, those who provide this care are licensed to administer medical treatment such as injections, catheter changes, wound dressings, and tube feedings.
Does Medicare cover social services?
Does Medicare cover medical social services? Medicare will pay for medically prescribed services that allow patients to cope with the emotional aftermath of an injury or illness. These may include in-home counseling from a licensed therapist or social worker.
Does Medicaid have a higher income limit?
Due to the high cost of long-term care, many states have higher Medicaid income limits for long-term care benefits than for other Medicaid coverage. However, Medicaid’s asset limits usually require you to “spend-down” resources before becoming eligible.
What is nursing home care?
Most nursing home care is. custodial care . Non-skilled personal care, like help with activities of daily living like bathing, dressing, eating, getting in or out of a bed or chair, moving around, and using the bathroom. It may also include the kind of health-related care that most people do themselves, like using eye drops.
What is custodial care?
Custodial care helps you with activities of daily living (like bathing, dressing, using the bathroom, and eating) or personal needs that could be done safely and reasonably without professional skills or training. Part A covers inpatient hospital stays, care in a skilled nursing facility, hospice care, and some home health care.
What is part A in nursing?
Part A covers inpatient hospital stays, care in a skilled nursing facility, hospice care, and some home health care. may cover care in a certified skilled nursing facility (SNF). It must be. medically necessary. Health care services or supplies needed to diagnose or treat an illness, injury, condition, disease, ...
What is home health care?
Home health care covers a wide range of treatment options that are performed by medical professionals at home. Care may include injections, tube feedings, condition observation, catheter changing, and wound care. Skilled therapy services are also included in home health care, and these include occupational, speech, ...
What percentage of Medicare Part B is DME?
Medicare Part B will cover 80 percent of the Medicare-approved amount for DME as long as the equipment is ordered by your physician and you rent or purchase the devices through a supplier that is participating in Medicare and accepts assignment.
How often do you need to be a skilled nursing nurse?
Treatments must be needed part time, at least once every 60 days, but not more than once daily for up to three weeks. You must be under the care of a physician.
Does Medicare cover speech therapy?
Medical social services may also be covered under your Medicare benefits.
Is home health care a good idea?
Home health care can be a good solution for those patients who need care for recovery after an injury, monitoring after a serious illness or health complication, or medical care for other acute health issues. Medicare recipients may get help paying for home health care if you meet specific criteria.
Do you have to pay 20 percent of Medicare deductible?
You will be required to pay 20 percent out of pocket, and the part B deductible may apply. If you are enrolled in a Medicare Advantage (MA) plan, you will have the same benefits as Original Medicare Part A and Part B, but many MA plans offer additional coverage. Related articles:
Does Medicare pay for home health?
If you do qualify for home health care, Medicare Part A and Part B may help cover the costs associated with your care. You will pay $0 for home health care services. If you require durable medical equipment, or DME, Medicare benefits will help pay for equipment you may need, including items that are designed for medical use in ...
What is Medicare Advantage?
Medicare Advantage, also called Medicare Part C, is the supplemental plan that covers non-skilled in-home care. Medicare Advantage plans are an alternative to traditional Medicare (Medicare Part A and Part B), both of which don’t cover non-skilled in-home health care. Not all Medicare Part C plans have the same coverage and benefits.
How to contact Medicare for a disability?
Even within a state, different areas may have different types of eligibility requirements. For questions, call Medicare at 1-800-MEDICARE (1-800-633-4227) or TTY at 1-877-486-2048.
What is respite care?
Respite Care. Some plans cover respite care, which can come in one of three forms. The first is a short-term stay in a nursing home or an assisted living facility. Many assisted living communities and hospice centers have rooms designated for short-term stay residents.
Can a caregiver take a break from surgery?
Those recovering from surgery or people whose caretakers are on vacation or unable to care for their patient may benefit from this type of respite care. In-home respite care is another option for caregivers who wish to have a break but prefer their loved one to stay at home.
Does Medicare Part C cover caregivers?
Medicare Part C plans have changed to allow some of the newly covered services to be provided by a professional caregiver or family member of the recipient’s choice. However, Medicare Part C-covered caregiver services are limited to a certain number of hours per year.
Does Medicare Cover Home Health Aides?
Medicare covers home health aides as part of a physician-ordered plan of care for you in your home if the following requirements are met:
Who Qualifies for Home Health Services Through Medicare?
You qualify for home health services through Medicare if your medical condition warrants it and you don’t need more than intermittent care. For instance, you may receive home health care after being treated and discharged from the hospital for an illness or injury until you are more self-sufficient.
What Kinds of Home Health Services Does Medicare Cover?
Home health services are provided in your home versus in a hospital or skilled nursing facility. Home health care is less expensive and more convenient for you because it is provided in the comfort of your home. The goals of home health services are to:
What Kind of Medicare Coverage is Best if You Need Home Health Aides?
Home health aide services are covered under Medicare Part A, long as you qualify for home health services and require the services of another skilled professional. Your copay for home health aide services provided within the limits set by Medicare is $0. You can receive your services from any Medicare-approved home health agency.
What Home Health Aides Are Not Covered by Medicare?
Home health aides are also called nurse aides or certified nurse aides who have completed federal and state-mandated training and maintain a license or certification through their state. Medicare will cover licensed or certified aides when their services are part of a plan of care provided by a Medicare-approved home health agency.
What is Home Health Care?
Like the name suggests, home health care involves a wide range of health and social services that are usually performed at a patient’s own home to treat illness, injuries, or other medical conditions.
What Home Health Care Services are Covered by Medicare?
Regardless of whether a patient’s condition is temporary or chronic, Medicare should pay for the following services:
What Home Health Care Services Are Not Covered by Medicare?
For Medicare to pay for medical services, the patient must be under a doctor’s care and should be getting services under a plan that doctors usually review.
Who is Eligible for Medicare Home Health Care Coverage?
To be eligible for Medicare Home Health Care coverage, you must meet the following requirements:
Out of Pocket Expenses: Deductibles & Copays
All Medicare parts have out-of-pocket expenses, with various groups of people being eligible for help to cover them.
