Aetna Medicare’s pharmacy network includes limited lower cost preferred pharmacies. You can find more information on the limitations at https://www.aetnamedicare.com/en/footers/disclaimers.html. CVS Caremark® Mail Service Pharmacy is our preferred network mail order service.
Full Answer
What is the preferred pharmacy for Aetna?
Jan 18, 2022 · CVS Caremark® Mail Service Pharmacy | Aetna Medicare CVS Caremark® Mail Service Pharmacy For medications you fill regularly Your plan offers a long-term supply (up to a 90-day or 100-day prescription, depending upon your plan), at select retail pharmacies and mail order. Please refer to your plan benefit information for more details.
What pharmacy does Aetna use?
Aetna Medicare | Rx Delivery Enjoy preferred pharmacy copays on mail prescriptions Delivery from CVS Caremark® Mail Service Pharmacy is convenient. Depending on your plan, you may save money on 90-day refills of the medicines you take regularly. Log in to your Caremark.com account to get started today.
How to find Aetna Medicare providers?
CVS Caremark Mail Service Pharmacy. P.O. Box 94467 Palatine, IL 60094-4467. NPI# 1427096809. CA Non-resident License # 1631. CVS Caremark Mail Service Pharmacy. P.O. Box 94467. Palatine, IL 60094-4467. NPI# 1033185186. CA Non-resident License # 540
What is the phone number for Aetna?
Feb 23, 2022 · Through a mail-order pharmacy: For a long-term supply (up to a 90-day or a 100-day prescription, depending on your plan) Order a refill when you have a 22-day supply left. For eye-drop medication. Order a refill when you have a 27-day supply left. If you order too early, the pharmacy won’t give you the refill until the approved date.
What mail order company does Aetna use?
Rx CVS Caremark®Rx CVS Caremark® Mail Order Pharmacy - Aetna | Home Delivery Service for Prescription Drugs & Medications.
Does Aetna use CVS Caremark?
Your secure Caremark account. Aetna Medicare partners with CVS Caremark®. This enables us to provide you with quality prescription drug coverage. And the services you need to easily manage your benefits.
Is OptumRx and Caremark the same?
OptumRx replaced CVS/Caremark on January 1, 2017 in administering prescription drug benefits for about 632,000 CalPERS members and their families.Oct 21, 2021
Does Aetna Medicare Rx Select have mail order?
For medications you fill regularly. Your plan offers a long-term supply (up to a 90-day or 100-day prescription, depending upon your plan), at select retail pharmacies and mail order.Jan 18, 2022
What is mail order pharmacy?
A “mail-order” prescription means that you don't have to pick up your medication from a pharmacy; instead, it is delivered to your doorstep. This article compares the benefits and challenges of mail-order vs. traditional pharmacies so that you can decide which option is best for you.Nov 11, 2019
What is Caremark mail order?
Your mail service plan, administered by CVS Caremark, includes mail order pharmacy service. For medicines you or your family members take regularly, the CVS Caremark Mail Service Pharmacy will deliver them to you -– at no extra cost. Mail service saves time and trips to your local retail pharmacy.
Is OptumRx a mail order pharmacy?
Prescriptions: Most prescription orders are shipped via USPS First Class Mail. Once OptumRx receives your complete order for a new prescription, your medications should arrive within ten business days. Completed refill orders should arrive to your home in about seven business days.
How does OptumRx work?
Order up to a 90-day supply of medications you take regularly. You can submit your order via phone, mail, online or through the OptumRx App. Additionally, your physician can electronically submit your prescription to OptumRx. OptumRx fills your order and mails it to you within seven days of placing the order.
Can I use OptumRx at Walgreens?
1 The OptumRx Walgreens90 Saver program allows you to get 90-day supplies of your maintenance medications at any of approximately 9,800 Walgreens pharmacies nationwide or through OptumRx home delivery — the choice is yours.
How do I use CVS Caremark mail-order?
Get started by signing in or registering for an account at caremark.com. Then select Start Prescription Delivery by Mail. You'll go right to our check drug cost and coverage tool, where you can easily search for your medication, request a new prescription, and submit an order.
Can I use Express Scripts with Aetna?
If you work in one of these states and select Aetna for your medical benefits, Express Scripts will be your pharmacy provider. Just like your medical plan covers visits to your doctor, your Express Scripts prescription plan covers the medicine your doctor prescribes.
How do I set up a mail-order prescription?
You can sign up for mail order by sending in your insurer's mail order form with your prescription. Another option is to have your healthcare provider phone or fax it in. You can usually submit refills online, over the phone or through a mobile app.3 days ago
Secure and safe medicines by mail
It's important to take your prescription medicines regularly. You can receive 90-day supplies of many drugs by mail, saving you trips to the drug store and missed doses. With your secure Caremark account you have access to:
We offer three easy ways to start delivery by mail
1. Ask your doctor to electronically prescribe your medicines to CVS Caremark Mail Service Pharmacy, NPI 1881952851. Your prescription will be delivered immediately.
Disclaimer
The typical number of business days after the mail order pharmacy receives an order for you to receive your shipment is up to 10 days. Enrollees have the option to sign up for automated mail order delivery. If your mail order drugs do not arrive within the estimated time frame, please contact us toll free at 1-866-235-5660, (TTY: 711).
How long does it take to fill a maintenance prescription?
Ask your doctor to write two prescriptions for your maintenance drug: A 30-day supply for you to fill at your local pharmacy. A 90-day supply (with three refills) Fill out the order form. Then mail it to us with your 90-day prescription. Be sure to include your method of payment.
What are the benefits of home delivery?
The perks of home delivery 1 Get more -- Depending on your plan, you can get up to a 90-day supply of medicine instead of a 30-day supply. And standard shipping is always free. 2 Save time – Refill your prescriptions just once every three months — with no trips to the pharmacy. You can re-order online, by phone or by mail. 3 Don’t worry -- Registered pharmacists check all orders for accuracy. Your medicine is securely packed, then mailed quickly to you. If you have an emergency, you can call our pharmacists anytime.
How long does it take to refill a prescription?
There are time guidelines for refilling your drugs. At a retail pharmacy: For a 30-day prescription. Order a refill when you have a 7-day supply left. For eye-drop medication. Order a refill when you have a 9-day supply left. Through a mail-order pharmacy:
How long does it take for eye drops to arrive?
For eye-drop medication. Order a refill when you have a 27-day supply left. If you order too early, the pharmacy won’t give you the refill until the approved date. You can get prescription drugs shipped directly to your home. Often, mail-order drugs arrive within 7 to 10 days.
How to save money on generics?
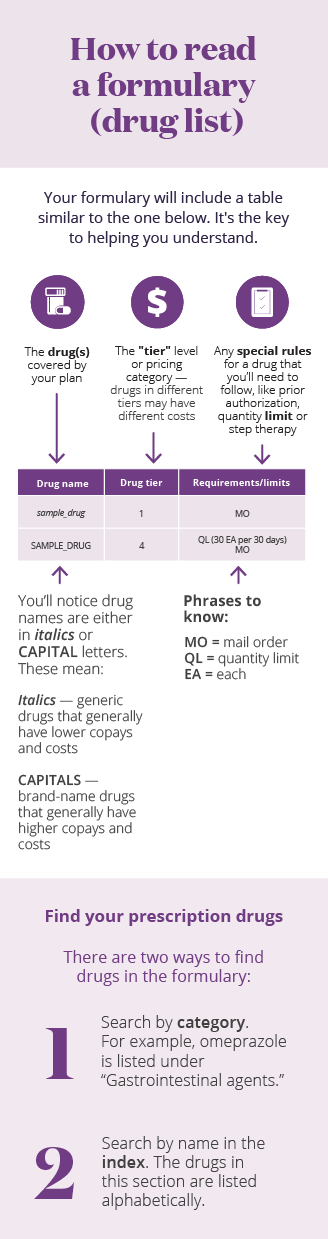
Save money by using generics. Sometimes you can save money by asking your doctor to prescribe the generic version of a brand-name medicine. Generic versions of brand-name drugs: Have the same active ingredients in the same amounts. Typically cost less.
Is there a network pharmacy?
There’s no network pharmacy close or open 24 hours. You need a prescription drug that nearby network or mail-order pharmacies don’t often stock, like drugs for rare medical conditions. You get a Part D prescription drug from an out-of-network provider pharmacy from: An emergency room.
Does Aetna have pharmacies?
Aetna Medicare Part D plans have a network of pharmacies throughout the country. It includes major retail pharmacy and grocery store chains and local independent pharmacies. The Pharmacy Search tool lets you see preferred and standard pharmacies in your area. You’re required to use a pharmacy in the network to fill your prescriptions.
Find a pharmacy near you
Medicare Part D plans have a network of pharmacies. Usually you must use a network pharmacy for the plan to pay for your prescription. Different plans may have different pharmacy networks, so it's always best to check.
Need help with Medicare enrollment?
Call a licensed agent at 1-855-335-1407 (TTY: 711) , Monday to Friday, 8 AM to 8 PM.
Get member help
Aetna members have access to contact information and resources specific to their plans.
How long does it take to get a prescription from mail order?
You should expect to get your prescription drugs 7 to 14 business days from the time the mail‐order pharmacy receives the order. If you don’t receive your prescription drug (s) within this time frame, please call us at the number on your ID card. You may have the option to sign up for automated mail‐order delivery.
Is Aetna search tool copyrighted?
By using this search tool, you acknowledge and agree that this search tool and all of the data belongs exclusively to Aetna Inc. and is protected by copyright and other law. This search tool is provided solely for the personal, noncommercial use of current and prospective Aetna members and providers. Use of any robot, spider or other intelligent agent to copy content from this search tool, extract any portion of it or otherwise cause the search tool to be burdened with unwarranted high access or transaction activity is strictly prohibited. Aetna reserves all rights to take appropriate civil, criminal or injunctive action to enforce these terms of use.
Can I use pharmacy finder for Aetna?
You can use the pharmacy finder tool to find network pharmacies for Aetna Medicare plans. We call them network pharmacies because we’ve contracted with them to provide prescription drugs to Aetna Medicare plan members. In most cases, your prescriptions are covered under our plan only if they’re filled either:
