Oral anti-nausea drugs: Medicare helps pay for oral anti-nausea drugs you use as part of an anti-cancer chemotherapeutic regimen if they’re administered before, at, or within 48 hours of chemotherapy or are used as a full therapeutic replacement for an intravenous anti-nausea drug.
Full Answer
What drugs are covered by Medicare drug plans?
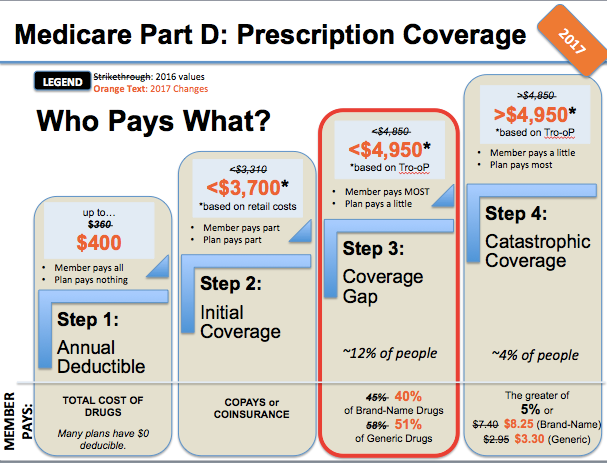
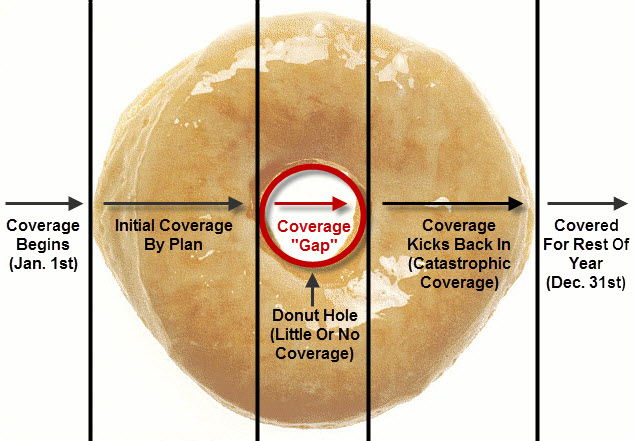
After your deductible has been satisfied, you will enter the Post-Deductible (also called Initial Coverage) stage, where you pay your copay and your plan covers the rest of the drug cost. Copay Range. $748. In the Donut Hole (also called the Coverage Gap) stage, there is a temporary limit to what Medicare will cover for your drug.
Are oral cancer drugs covered by Medicare?
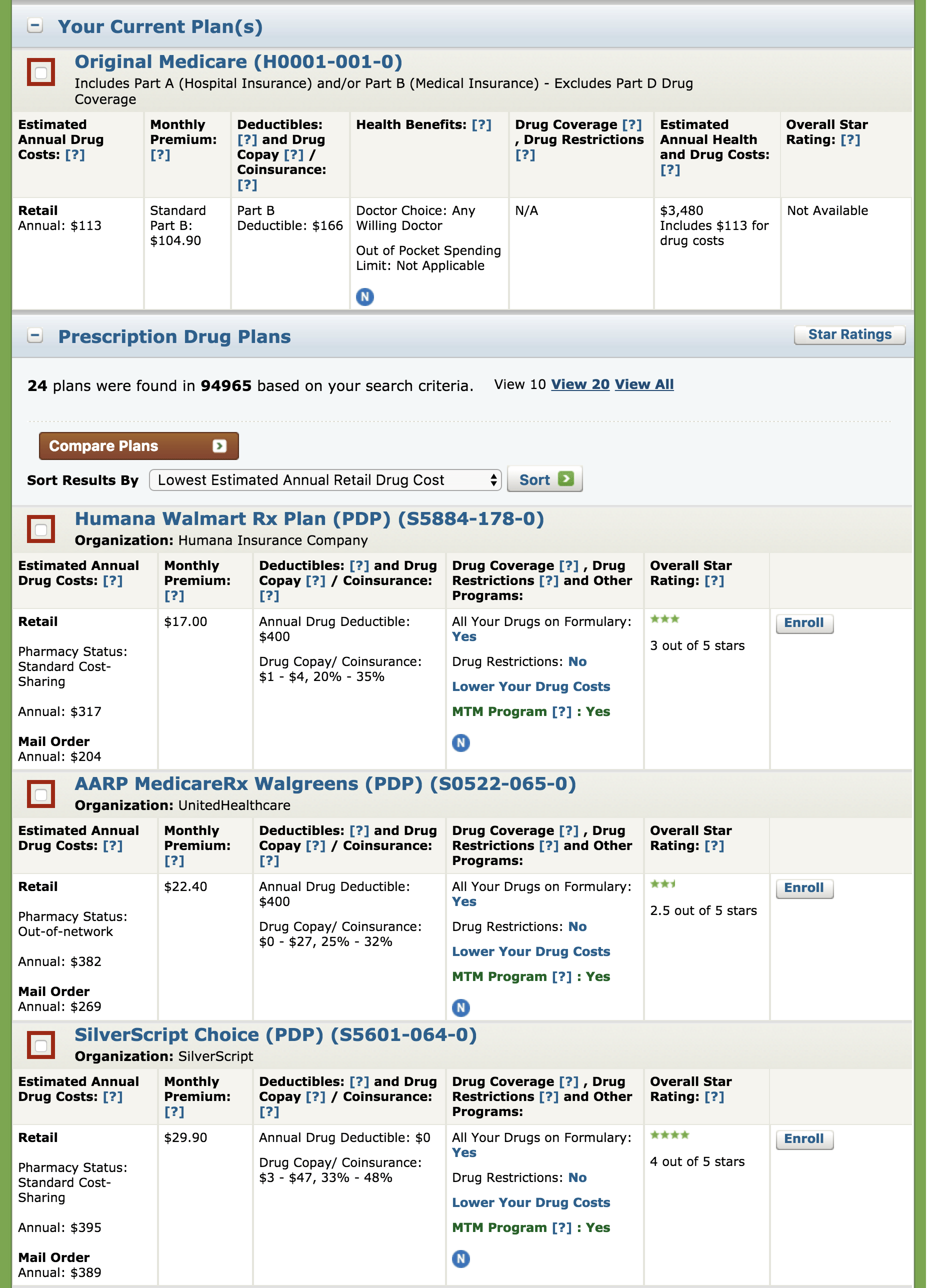
Feb 01, 2013 · Medicare drug plans that cover Oracea Oracea I was just going over drug plans or Medicare part d prescription drug plans that cover Oracea. This is the skin disease that is like a rash. Well the retail drug itself costs over $400. WOW. It is very expensive and Cigna seems to cover the most in Pennsylvania when it comes to medicare.
What do I need to know about Medicare prescription drug coverage?
Below is the formulary, or list of prescription drugs available to enrollees, for every 2019 Medicare Advantage Plan in Michigan and 2019 Medicare Part-D in Michigan plans that offers additions coverage for Oracea 40mg/1 in Van-Buren county Michigan. A formulary is a list of prescription medications that are covered if you choose to enroll with that plan.
What are the different tiers of Medicare drug plans?
Select your area of coverage to compare Medicare Prices for Oracea NDC#00299382230 . ... 2022 Medicare Advantage Plans; 2022 Medicare Part-D Plans; 2021-2014 Medicare. 2021 Medicare Advantage Plans ... Resources. State Health Insurance Assistance Programs SHIP; Articles; Select Page. Compare Medicare Drug Prices for Oracea. Select Your State to ...
Is Oracea covered by Medicare?
No. In general, Medicare prescription drug plans (Part D) do not cover this drug. Be sure to contact your specific plan to verify coverage information. A limited set of drugs administered in a doctor's office or hospital outpatient setting may be covered under Medical Insurance (Part B).
Is there a generic for Oracea?
Oracea is a brand-name drug used to treat skin lesions caused by rosacea. The generic version of Oracea is doxycycline.
Are doxycycline and Oracea the same thing?
There is an acute difference however between doxycycline (Oracea, Galderma), which is 40mg of doxycycline in a controlled dosing manner (and an anti-inflammatory dose), and low-dose antibiotics.Dec 28, 2015
How do you find out what drugs are covered by Medicare?
Get information about specific drug plans and health plans with drug coverage in your area by visiting Medicare.gov/plan-compare or by calling 1-800-MEDICARE (1-800-633-4227). TTY users can call 1-877-486-2048.
How long can you stay on Oracea?
ORACEA should not be used for the treatment or prevention of infections. It is not known if ORACEA is: effective for use for longer than 16 weeks. safe for use longer than 9 months.
Does Oracea cause weight gain?
Approximately 5% of patients taking Oracea reported either loss of appetite and or nausea as a side effect of the medication. There were no reports of weight gain as a side effect from patients taking Oracea. If the weight gain persists you should be evaluated by your physician.
How long do you take Oracea for rosacea?
Oracea should not be used for the treatment or prevention of infections. It is not known if Oracea is: effective for use for longer than 16 weeks. safe for use longer than 9 months.Aug 23, 2021
What is the best antibiotic for rosacea?
Oral medications such as tetracycline, doxycycline, and minocycline, all have been proven to keep rosacea's bacterial component under control and also seem to have an anti-inflammatory benefit. Topical products such as metronidazole and clindamycin work in much the same way.
How long can you stay on doxycycline for rosacea?
Systemic treatment They are usually prescribed for 6–12 weeks, and this can be variable, depending on the severity of the rosacea. Doxycycline 50–100 mg once daily is recommended as initial oral therapy. Further courses may be required, as inflammatory rosacea is chronic and often recurs.
What drugs are not covered by Medicare Part D?
Medicare does not cover:Drugs used to treat anorexia, weight loss, or weight gain. ... Fertility drugs.Drugs used for cosmetic purposes or hair growth. ... Drugs that are only for the relief of cold or cough symptoms.Drugs used to treat erectile dysfunction.More items...
Why do doctors not like Medicare Advantage plans?
If they don't say under budget, they end up losing money. Meaning, you may not receive the full extent of care. Thus, many doctors will likely tell you they do not like Medicare Advantage plans because the private insurance companies make it difficult for them to get paid for the services they provide.
What drugs are covered under Medicare Part B?
Drugs that are covered by Medicare Part B include the following.Certain Vaccines. ... Drugs That Are Used With Durable Medical Equipment. ... Certain Antigens. ... Injectable Osteoporosis Drugs. ... Erythropoiesis-Stimulating Agents. ... Oral Drugs for ESRD. ... Blood Clotting Factors. ... Immunosuppressive Drugs.More items...•Jan 11, 2022
Medicare drug plans that cover Oracea
I was just going over drug plans or Medicare part d prescription drug plans that cover Oracea. This is the skin disease that is like a rash. Well the retail drug itself costs over $400. WOW. It is very expensive and Cigna seems to cover the most in Pennsylvania when it comes to medicare.
Follow Blog via Email
Enter your email address to follow this blog and receive notifications of new posts by email.
How to get prescription drug coverage
Find out how to get Medicare drug coverage. Learn about Medicare drug plans (Part D), Medicare Advantage Plans, more. Get the right Medicare drug plan for you.
What Medicare Part D drug plans cover
Overview of what Medicare drug plans cover. Learn about formularies, tiers of coverage, name brand and generic drug coverage. Official Medicare site.
How Part D works with other insurance
Learn about how Medicare Part D (drug coverage) works with other coverage, like employer or union health coverage.
What is a drug plan's list of covered drugs called?
A plan’s list of covered drugs is called a “formulary,” and each plan has its own formulary. Many plans place drugs into different levels, called “tiers,” on their formularies. Drugs in each tier have a different cost. For example, a drug in a lower tier will generally cost you less than a drug in a higher tier.
How many drugs does Medicare cover?
All Medicare drug plans generally must cover at least 2 drugs per drug category, but plans can choose which drugs covered by Part D they will offer. The formulary might not include your specific drug. However, in most cases, a similar drug should be available.
What is formulary exception?
A formulary exception is a drug plan's decision to cover a drug that's not on its drug list or to waive a coverage rule. A tiering exception is a drug plan's decision to charge a lower amount for a drug that's on its non-preferred drug tier.
What happens if you don't use a drug on Medicare?
If you use a drug that isn’t on your plan’s drug list, you’ll have to pay full price instead of a copayment or coinsurance, unless you qualify for a formulary exception. All Medicare drug plans have negotiated to get lower prices for the drugs on their drug lists, so using those drugs will generally save you money.
How many prescription drugs are covered by Medicare?
Plans include both brand-name prescription drugs and generic drug coverage. The formulary includes at least 2 drugs in the most commonly prescribed categories and classes. This helps make sure that people with different medical conditions can get the prescription drugs they need. All Medicare drug plans generally must cover at least 2 drugs per ...
What does Medicare Part D cover?
All plans must cover a wide range of prescription drugs that people with Medicare take, including most drugs in certain protected classes,” like drugs to treat cancer or HIV/AIDS. A plan’s list of covered drugs is called a “formulary,” and each plan has its own formulary.
What is a tier in prescription drug coverage?
Tiers. To lower costs, many plans offering prescription drug coverage place drugs into different “. tiers. Groups of drugs that have a different cost for each group. Generally, a drug in a lower tier will cost you less than a drug in a higher tier. ” on their formularies. Each plan can divide its tiers in different ways.
What is Medicare approved amount?
Medicare-Approved Amount. In Original Medicare, this is the amount a doctor or supplier that accepts assignment can be paid. It may be less than the actual amount a doctor or supplier charges. Medicare pays part of this amount and you’re responsible for the difference.
How long does Medicare cover after kidney transplant?
If you're entitled to Medicare only because of ESRD, your Medicare coverage ends 36 months after the month of the kidney transplant. Part A covers inpatient hospital stays, care in a skilled nursing facility, hospice care, and some home health care. coverage. Transplant drugs can be very costly.
What is Medicare Part A?
Medicare Part A (Hospital Insurance) Part A covers inpatient hospital stays, care in a skilled nursing facility, hospice care, and some home health care. coverage. Transplant drugs can be very costly. If you’re worried about paying for them after your Medicare coverage ends, talk to your doctor, nurse, or social worker.
What is Part B in medical?
Prescription drugs (outpatient) Part B covers certain doctors' services, outpatient care, medical supplies, and preventive services. covers a limited number of outpatient prescription drugs under limited conditions. A part of a hospital where you get outpatient services, like an emergency department, observation unit, surgery center, or pain clinic.
What is a prodrug?
A prodrug is an oral form of a drug that, when ingested, breaks down into the same active ingredient found in the injectable drug. As new oral cancer drugs become available, Part B may cover them. If Part B doesn’t cover them, Part D does.
What happens if you get a drug that Part B doesn't cover?
If you get drugs that Part B doesn’t cover in a hospital outpatient setting, you pay 100% for the drugs, unless you have Medicare drug coverage (Part D) or other drug coverage. In that case, what you pay depends on whether your drug plan covers the drug, and whether the hospital is in your plan’s network. Contact your plan to find out ...
What is Part B covered by Medicare?
Here are some examples of drugs Part B covers: Drugs used with an item of durable medical equipment (DME) : Medicare covers drugs infused through DME, like an infusion pump or a nebulizer, if the drug used with the pump is reasonable and necessary.
What is the donut hole in Medicare?
In the Donut Hole (also called the Coverage Gap) stage, there is a temporary limit to what Medicare will cover for your drug. Therefore, you may pay more for your drug. In the Post-Donut Hole (also called Catastrophic Coverage) stage, Medicare should cover most of the cost of your drug.
What is the post deductible stage of a drug?
After your deductible has been satisfied, you will enter the Post-Deductible (also called Initial Coverage) stage, where you pay your copay and your plan covers the rest of the drug cost.
Does Medicare cover prescription drugs?
No. In general, Medicare prescription drug plans (Part D) do not cover this drug. Be sure to contact your specific plan to verify coverage information. A limited set of drugs administered in a doctor's office or hospital outpatient setting may be covered under Medical Insurance (Part B).